AR-V7 Linked to Targeted Therapy Resistance in Prostate Cancer
A new study found that the androgen receptor splice variant 7 is associated with resistance to two therapies for metastatic castration-resistant prostate cancer.
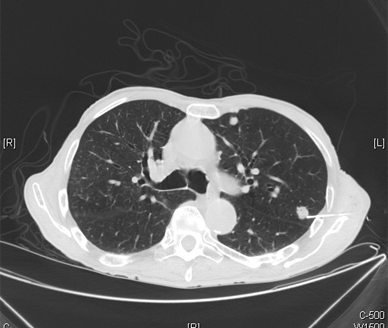
Metastatic prostate adenocarcinoma shown on CT; source: Yale Rosen, Wikimedia Commons
A variant of the androgen receptor, androgen receptor splice variant 7 (AR-V7), is associated with resistance to two therapies for metastatic castration-resistant prostate cancer (CRPC), according to the results of a study published in the New England Journal of Medicine.
Detection of the AR-V7 variant in circulating tumor cells (CTCs) of men with CRPC treated with either enzalutamide or abiraterone correlated with a worse prognosis-a lower prostate-specific antigen (PSA) response, as well as a shorter progression-free survival (PFS) and overall survival. None of the men with CTCs harboring the AR-V7 variant responded to either enzalutamide or abiraterone.
The finding of the resistance to enzalutamide in the presence of the AR-V7 variant was previously presented at the 2014 American Association for Cancer Research Annual Meeting.
“[The authors] report compelling clinical data endorsing the importance of androgen-receptor variants in mediating treatment resistance,” wrote Peter S. Nelson, MD, of the Fred Hutchinson Cancer Research Center in Seattle, in an accompanying editorial.
According to Nelson, a biomarker such as AR-V7 with 100% specificity in predicting a lack of treatment response “would be a major step forward and would probably achieve rapid adoption.” Still, because these results are from a relatively small sample of patients, a larger prospective study is necessary for validation.
Emmanuel S. Antonarakis, MD, assistant professor of oncology at Johns Hopkins Sidney Kimmel Comprehensive Cancer Center in Baltimore, and colleagues tested for the presence of both the full-length androgen receptor messenger RNA (mRNA) and the AR-V7 mRNA in the CTCs of 62 men with metastatic CRPC treated with either enzalutamide or abiraterone. Levels of AR-V7 were lower prior to treatment exposure and increased after post-treatment progression with either therapy.
Of the 31 men treated with enzalutamide, 39% had detectable AR-V7 levels. These men had a 0% PSA response compared with a 53% response in men with no detectable AR-V7 (P = .004). The median PFS was 1.4 months in AR-V7–positive patients compared with 6.0 months in AR-V7–negative patients (P < .001).
Results were similar for men treated with abiraterone. Of the 31 abiraterone-treated patients, 19% had detectable levels of AR-V7, as well as a lower PSA response compared with those with no detectable AR-V7 (0% vs 68%, respectively; P = .004). The abiraterone-treated patients with detectable AR-V7 levels had a median PFS of 1.3 months, while the PFS of men with no detectable AR-V7 has not yet been reached (P < .001). Overall survival was also shorter in men with detectable AR-V7 in both treatment groups.
According to Antonarakis, this is the first study to document the prevalence of AR-V7 in patients treated with either enzalutamide or abiraterone. “In men with metastatic CRPC who have not received either abiraterone or enzalutamide, the prevalence of AR-V7 is about 13%. However, in men with metastatic CRPC who have received both abiraterone and enzalutamide, the prevalence of AR-V7 is about 67%,” said Antonarakis.
Antonarakis cautioned that the enzalutamide and abiraterone cohorts from this study cannot be directly compared because the enzalutamide-treated cohort generally had more advanced disease compared with the abiraterone-treated patients. Still, one of the key messages from this study is the relative common frequency of AR-V7 among men with CRPC.
The researchers are continuing to follow these patients for overall survival and are beginning to incorporate the CTC-based AR-V7 assay into prospective therapeutic trials of both abiraterone and enzalutamide to validate these results in larger patient cohorts.
If validated, because of the 3-day turnaround time for the assay, “we believe that this noninvasive test could be readily used in the future for any patient with CRPC who is contemplating therapy with enzalutamide or abiraterone,” Antonarakis told Cancer Network.