Drug Combo Improves Quality of Life in Multiple Myeloma Patients
Treatment with lenalidomide and dexamethasone improved quality-of-life measures in multiple myeloma patients, according to a study presented at the 2014 ASCO Annual Meeting.
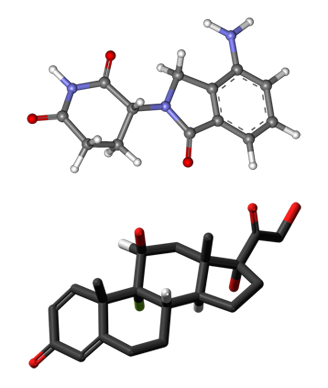
Ball-and-stick model of lenalidomide (top) and dexamethasone (bottom)
Treatment with lenalidomide and low-dose dexamethasone significantly improved some quality-of-life measures over melphalan, prednisone, and thalidomide (MPT) in multiple myeloma patients, according to a new study presented at the 2014 American Society of Clinical Oncology (ASCO) Annual Meeting in Chicago.
“Multiple myeloma is an incurable disease, and it causes a high symptom burden associated with a significant reduction in quality of life,” said Michel Delforge, MD, PhD, of University Hospital Leuven in Belgium, who presented the new study. “Treatment objectives should be to control the disease, to prolong survival, but not at the expense of toxicity.”
The new study was a pre-determined analysis from the FIRST trial, which showed a significant improvement in progression-free and overall survival with continuous treatment with lenalidomide and low-dose dexamethasone (Rd) compared with fixed duration of the same regimen and with MPT. In the new analysis, the two Rd arms were combined because the progression-free survival differences only emerged after 18 months, and the quality-of-life analysis only covered those 18 months.
Thus, there were 1,076 patients in the Rd arm and 547 in the MPT arm. Quality-of-life measures including the EORTC QLQ-C30 and the QLQ-MY20 were administered at baseline, after the first cycle of therapy, and at the end of months 3, 6, 12, and 18, and at study discontinuation. Delforge stressed that compliance with the questionnaires was very high; at 3 months compliance was 95% for Rd patients and 94% for MPT patients. This dropped at 12 and 18 months, however; at the latter time point compliance rates were 85% and 67%, respectively, which was a significant difference.
On the MY20, which measures disease symptoms and is particularly focused on pain, there was a significant improvement in both treatment arms compared to baseline at each time point. “There was a trend toward better symptom improvement with Rd, which reached statistical significance at 3 months, and it might reflect the rapid activity of this treatment,” Delforge said. With regard to patient-reported side effects, Rd yielded a significantly and clinically meaningful reduction compared with MPT at all time points except month 18.
On the QLQ-C30, scores improved from baseline at every time point in both arms, with no difference between the treatments. Not surprisingly, health-related quality of life deteriorated significantly in all patients at disease progression.
“We believe that this improvement in health-related quality of life with Rd, and specifically the reduction in treatment-related side effects, may facilitate patient adherence,” Delforge said. “Longer treatment duration and better adherence may improve outcomes for the patient.”
Luciano Costa, MD, PhD, of the Medical University of South Carolina, was the discussant for the session, and noted that there is no information yet on the effect on neuropathies. “I think we missed an opportunity to revisit the issue of continuous therapy vs fixed duration therapy with later quality-of-life time points that would allow comparison,” he said.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.