NLST: Lung Screening Benefits High-Risk Individuals Most
Results from the National Lung Screening Trial showed that screening for lung cancer with low-dose computed tomography yielded the most benefit among individuals who were at highest risk for cancer and less benefit in lower risk people.
Results from the National Lung Screening Trial (NLST) showed that screening for lung cancer with low-dose computed tomography (CT) yielded the most benefit among individuals who were at highest risk for cancer and less benefit in lower risk people.
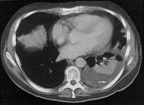
A single CT shows a malignant, left-sided pleural effusion in this patient with adenocarcinoma of the lungs. Note the intrapleural tumor nodule (arrow). Further nodularity is identified posteromedially. The atelectatic left lower lobe floats on the pleural fluid.
“Our findings are a proof of principle that calculating a smoker’s risk of lung cancer death could better predict who among heavy smokers may derive the most benefit from low-dose CT lung screening,” said study lead author Stephanie Kovalchik, PhD, of the National Cancer Institute in Rockville, Maryland. “This information would be useful to screening program planners to better project the benefits and harms of proposed programs.”
The researchers calculated the number of lung cancer deaths prevented among 26,604 participants in the NLST who underwent low-dose CT screening and compared them to 26,554 patients who underwent chest radiography. They divided participants into 5-year lung cancer–death risk quintiles, ranging from 0.15% to 0.55% risk of death in the lowest group up to more than 2% in the highest risk quintile. The results were published on July 18 in the New England Journal of Medicine.
The deaths per 10,000 person-years prevented in the CT group as compared to the radiography group increased according to risk quintile: 0.2 lung cancer deaths prevented in the lowest risk quintile, followed by 3.5, 5.1, 11, and 12 deaths prevented (P = 0.01 for trend). False positives were less likely as risk increased, with the number of false positives per death prevented dropping from 1,648 in the lowest risk group to 64 and 65 in the fourth and fifth quintiles, respectively.
The three highest risk quintiles, or the 60% of participants at highest risk, accounted for 88% of the lung cancer deaths prevented. The lowest risk quintile meanwhile, accounted for only 1% of prevented deaths.
Dr. Kovalchik said in an e-mail that risk stratification could feasibly be used to design screening programs right away. “Because the information needed in the risk calculation, such as smoking history and demographics, can be asked of the patient, the risk calculation could be immediately available with the aid of a nomogram or a computer app,” she said. “However, because the model has only been validated in research cohorts, it should also be validated in a national representative sample of US smokers before it is used to assess lung cancer–death risk in the general population.”
Study Details
The NLST randomized participants to three annual screenings using either low-dose CT or chest radiography. All patients were between the ages of 55 and 74 and had a minimum of 30 pack-years of smoking; patients were only eligible if they had quit 15 years or less before the trial.
In the current analysis, 59% of patients were male in both CT and radiography groups, and about 90% in both groups were white. About 52% in each group were former smokers, and about 34% of participants had at least 60 pack-years of smoking history.