Role of Neoadjuvant Oxaliplatin Unclear in Early Rectal Cancer
The role of oxaliplatin in early-stage rectal cancer may still be unclear, according to the differing disease-free survival results from two studies presented at the 2014 ASCO Annual Meeting.
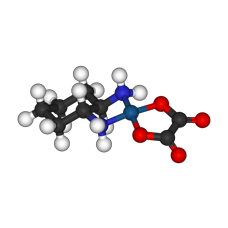
Ball-and-stick model of oxaliplatin
CHICAGO-The role of oxaliplatin in early-stage rectal cancer may still be unclear, according to the differing disease-free survival results from two studies examining its use in preoperative chemoradiotherapy and postoperative chemotherapy regimens presented at the 2014 American Society of Clinical Oncology (ASCO) Annual Meeting.
Claus Rodel, MD, of the University of Frankfurt, Germany, presented results of the German CAO/ARO/AIO-04 trial that showed that adding oxaliplatin to 5-FU-based neoadjuvant chemoradiation and adjuvant chemotherapy improved disease-free survival compared with treatment with 5-FU alone.
In contrast, Hans-Joachim Schmoll, MD, of Martin Luther University Halle-Wittenburg, Germany, presented the results of an interim analysis of the EORTC-PETACC-6 trial that indicated that adding oxaliplatin to capecitabine plus radiotherapy did not improve disease-free survival compared with capecitabine plus radiotherapy alone.
In his discussion of the results of these two studies, Carmen Joseph Allegra, MD, of the University of Florida said that the weight of evidence supports a lack of benefit for the addition of oxaliplatin to fluoropyrimidine-sensitized radiation therapy in the neoadjuvant rectal setting and is not recommended for use in clinical practice.
Oxaliplatin With 5-FU
The CAO/ARO/AIO-04 trial included 1,256 patients with clinically-staged T3-4 or any node-positive rectal cancer. Patients were randomly assigned to preoperative 50.4 Gy plus infusional 5-FU followed by total mesorectal excision surgery and 4 cycles of bolus 5-FU (n = 627), or preoperative 50.4 Gy plus infusional 5-FU and oxaliplatin followed by surgery and 8 cycles of oxaliplatin, leucovorin, and infusional 5-FU (n = 613).
The primary endpoint was disease-free survival and the median follow-up was 50 months. Seventy-six percent of patients in both arms of the trial started adjuvant chemotherapy.
There were 198 disease-free survival events in the 5-FU–alone arm and 159 in the 5-FU/oxaliplatin arm. The 3-year disease-free survival was 71.2% for patients assigned 5-FU alone compared with 75.9% for patients on combination treatment (HR = 0.79; P = .03). No significant difference in overall survival was observed at 3 or 5 years.
“We showed that a regimen of preoperative 5-FU/oxaliplatin chemoradiation therapy with 1 week chemotherapy gap was well tolerated and associated with a high compliance rate and an increased pathologic complete response rate,” Rodel said.
Oxaliplatin With Capecitabine
In the PETACC-6 trial, 1,094 patients with resectable rectal adenocarcinoma were randomly assigned to preoperative chemoradiation with capecitabine followed by 6 cycles of adjuvant chemotherapy with capecitabine with (537 evaluable patients) or without oxaliplatin (544 evaluable patients) before and after surgery.
Only 79% of the patients assigned capecitabine plus radiotherapy and 63% of patients in the oxaliplatin arm started adjuvant chemotherapy. Sixty-nine percent of patients assigned capecitabine alone and 57% of patients assigned the oxaliplatin combination completed the full 6 cycles of treatment.
“Interim results at a median follow-up of 2.6 years indicate no disease-free survival benefit for the addition of oxaliplatin to pre- and postoperative capecitabine,” Schmoll said during his presentation.
At 3 years, 124 disease-free survival events occurred in the capecitabine alone arm and 121 occurred in the oxaliplatin combination arm. The 3-year disease-free survival in the intent-to-treat population was 74.5% for patients assigned capecitabine and 73.9% for capecitabine plus oxaliplatin (HR = 1.04; P = .78).
Looking at the relapse rate at 3 years, the local relapse rate for capecitabine was 7.6% compared with 4.6% for capecitabine plus oxaliplatin; distant relapse was 19.2% for capecitabine compared with 17.6% for capecitabine plus oxaliplatin, both nonsignificant differences.
Results were similar for the overall survival analysis as well, with patients assigned capecitabine having a 3-year overall survival of 89.5% compared with 87.4% for patients assigned the combination (HR = 1.31; P = .179).
Schmoll noted that this interim analysis was early with only 250 out of 440 expected events having occurred. At least 2 more years of follow-up will be needed for the final evaluation.