Role of Obesity and Exercise in Breast Cancer Survivors
After malignancies of the skin, breast cancer is the most common cancer
Over 60% of the American population meets the criteria for obesity, and obesity is very common in patients with breast cancer. Many studies have shown that obese patients with breast cancer have a worse prognosis compared to normal weight individuals. Tumor characteristics and other factors contribute to this. Exercise could reverse some of the pathophysiologic factors that contribute to this increased risk, and has been shown in some studies to improve survival in patients with breast cancer. In addition to administering anticancer therapy, cancer clinicians should make concerted attempts to get patients to enroll in weight management and exercise programs, which could improve survival in patients with breast cancer.
After malignancies of the skin, breast cancer is the most common cancer among women in North America. Breast cancer constitutes 26% of all cancers and 15% of cancer-related mortalities among women in the United States.[1] With approximately 2.5 million breast cancer survivors, many of these patients will develop either local or distant relapse of their disease.[2] It is therefore important to identify modifiable risk factors influencing disease recurrence. Diet and lifestyle changes are modifiable factors that are relatively easy to change and could affect long-term survival in breast cancer patients. Patients typically look to treating clinicians for advice regarding lifestyle changes that could improve their disease outcome. This article evaluates the impact of obesity and exercise on breast cancer relapse and mortality.
Obesity and Breast Cancer
Obesity is considered a risk factor for breast cancer. With 66% of patients being obese at diagnosis, this is slightly higher than the prevalence of obesity (60%) in the United States generally.[3] In a cohort of 3,993 women with nonmetastatic breast cancer followed for an average of 6.3 years, each 5-kg gain in weight was associated with a 13% increase in breast cancer–specific mortality (P = .01).[4] Postmenopausal women with a body mass index (BMI) of more than 30 kg/ m2 have a relative risk of developing breast cancer ranging from 1.23 (95% confidence interval [CI] = 1.00–1.59) to 2.52 (95% CI = 1.62–3.93).[3,5]
Risk of Death and Recurrence
In some studies, obese patients also seem to have a higher incidence of estrogen receptor (ER)-, progesterone receptor (PR)-, and HER2/neu-negative (“triple-negative”) tumors, which carry a poorer prognosis.[6-8] Chlebowski and colleagues performed a comprehensive literature review including information from 159 references, based on observational studies showing that women who are overweight or who gained weight after breast cancer diagnosis had a greater risk of breast cancer recurrence and death compared with lighter women.[9]
TABLE 1

Studies of Obesity and Breast Cancer Recurrence
In a single-center study of 1,367 patients with breast cancer followed for a median duration of 6.8 years, women in the highest weight category (≥ 175 lb [79 kg]) experienced a 2.5-fold increased risk of dying from breast cancer (hazard ratio [HR] = 2.54; 95% CI = 1.08–6.00; trend P = .02), compared to women in the lowest category of weight (< 133 lb [60 kg]) at diagnosis (Table 1). Also, ER-negative women in the upper 50th percentile of weight with early-stage disease had an almost fivefold increased risk of dying (HR = 4.99; 95% CI = 2.17–11.48; P for interaction = .10) compared with women in the lower 50th percentile of weight and ER-positive tumors. Patients with early-stage cancer (stage I/IIA) who weighed more than 175 lb had a hazard ratio of 2.39 (95% CI = 1.01–5.63) for death.[10]
In a study of 6,792 patients who had been randomized to International Breast Cancer Study Group trials from 1978 to 1993, Berclaz and colleagues showed that patients with a normal BMI had significantly longer overall survival (OS) and disease-free survival (DFS) compared with patients in intermediate BMI or obese categories, after adjusting for other factors.[11] In another study, obese woman had poorer outcomes and lower complete response rates while being treated with adjuvant therapy compared to normal-weight women.[12]
In a recent study from M.D. Anderson Cancer Center, Dawood et al reported that patients with locally advanced breast cancer who were either obese or overweight had a worse overall survival and recurrence-free survival compared to normal-weight patients (P = .001). In this study, obese patients also had a higher incidence of visceral recurrence (liver, lung, brain) compared to normal-weight or underweight patients.[13]
Dignam and colleagues published an analysis of 3,385 patients enrolled in the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-14 trial, a randomized, placebo-controlled trial of ER-positive patients on tamoxifen therapy. The authors looked for an association between obesity and breast cancer recurrence, and they found that obesity increased overall mortality but did not affect breast cancer recurrence.Tamoxifen reduced the risk of breast cancer recurrence and mortality regardless of a patient’s BMI.[14]
Possible Mechanism for Increased Breast Cancer Mortality in Obese Patients
FIGURE 1

Obesity–Breast Cancer Link-
Possible mechanisms of the effect of obesity on breast cancer tumorigenesis. FFA = free fatty acid; IGF-1 = insulin-like growth factor type 1.
One postulated mechanism for increased relapse of breast cancer in obese patients is the increased levels of bioavailable estrogen in these patients due to greater conversion of androgens to estrogen in adipose tissue (Figure 1). Obese postmenopausal woman have been shown to have increased circulating concentrations of estrone and estradiol with concomitant decreased levels of sex hormone–binding globulin, thus leading to increased bioavailable estrogen.[15-18]
Insulin and insulin-like growth factor (IGF-1) levels increase at higher BMIs.[19] Insulin resistance, leading to increased levels of IGF-1, may promote breast tumorigenesis. Higher levels of fasting insulin in one study increased the risk of recurrence and death in breast cancer patients.[20] Obese patients also have more aggressive tumors,[21] are likely to have metastatic lymph nodes,[22,23] are more likely to be ER- and PR-negative,[21,24] and tend to have a complicated surgical course.[25,26] Undertreatment of obese patients with chemotherapy has also been reported.[27,28]
Benefit of Exercise in Patients With Breast Cancer
Evidence
In an epidemiologic study done by Abrahamson et al, 1,264 patients diagnosed with breast cancer were asked about their recreational physical activity by questionnaire (Table 2). Patients with the greatest physical activity 1 year before diagnosis had a modest reduction in the hazard ratio for death (HR = 0.78, 95% CI = 0.56–1.08).[29]
TABLE 2
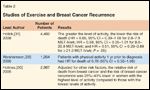
Studies of Exercise and Breast Cancer Recurrence
Holmes and colleagues examined data from 2,987 nurses in the Nurses Health Study diagnosed with stage I, II, or III breast cancers and looked at breast cancer mortality in relation to physical activity level. The study showed that woman engaged in at least 3 metabolic equivalents (MET) of exercise per week had a relative risk of death from breast cancer of 0.80 (95% CI = 0.60–1.06), while those with 9 to 14.0 MET/wk had a relative risk of 0.50 (95% CI = 0.31–0.82). Adjusted for other risk factors, the relative risk of death from breast cancer and the risk of breast cancer recurrence was 25% to 40% lower in women with the highest level of activity, compared to women with the lowest levels of activity. Of note, most of the benefit was seen in women with moderate activity, equivalent to walking 3 to 5 hours a week at an average pace of 2 to 2.9 mph. Patients who were ER- and PR-positive appeared to benefit the most from exercise.[30]
Similar results were reported in a prospective study of breast cancer patients followed from 1998 to 2001 in the Collaborative Women’s Longevity Study (CWLS). Women engaging in greater levels of activity had a significantly lower risk of dying from breast cancer (HR = 0.65, 95% CI = 0.39–1.08 for 2.8–7.9 MET-h/wk; HR = 0.59, 95% CI = 0.35–1.01 for 8.0–20.9 MET-h/wk; and HR = 0.51, 95% CI = 0.29–0.89 for ≥ 21.0 MET-h/wk; P = .05) compared to those performing less than 2.8 MET-h/wk in physical activity.[31]
Possible Mechanisms
TAKE HOME POINTS
Previous studies have shown that physical activity decreases the incidence of breast cancer.[32] Insulin and insulin-like growth factor (IGF-1) levels increase at higher BMIs.[19] Irwin et al showed that moderate-intensity aerobic exercise decreased IGF-1 and insulin growth factor–binding protein (IGFBP) levels.[33] Decrease in insulin levels could translate into less recurrence of breast cancer and better prognosis. Another mechanism by which exercise could be beneficial is via lowering of estrogen levels.[34,35] Evidence also suggests that exercise improves quality of life in breast cancer survivors.[36]
Conclusions
Obese patients are more likely to get breast cancer and also have a worse prognosis from the disease. Exercise appears to attenuate the physiologic processes that increase the incidence and mortality from breast cancer. The feasibility of increasing physical activity in patients with breast cancer has been studied, and the results are encouraging. Exercise has also been shown to decrease all-cause mortality in patients with breast cancer. This could be a reflection of the known benefits of exercise in decreasing cardiovascular mortality. With the current obesity epidemic, it is essential that oncologists discuss the beneficial effects of exercise and weight loss in improving overall survival in patients with breast cancer.
References:
References
1. Jemal A, Siegel R, Ward E, et al: Cancer statistics, 2007. CA Cancer J Clin 57:43-66, 2007.
2. Natarajan L, Pu M, Parker BA, et al: Time-varying effects of prognostic factors associated with disease-free survival in breast cancer. Am J Epidemiol 169:1463-1470, 2009.
3. Morimoto LM, White E, Chen Z, et al: Obesity, body size, and risk of postmenopausal breast cancer: The Women’s Health Initiative (United States). Cancer Causes Control 13:741-751, 2002.
4. Nichols HB, Trentham-Dietz A, Egan KM, et al: Body mass index before and after breast cancer diagnosis: Associations with all-cause, breast cancer, and cardiovascular disease mortality. Cancer Epidemiol Biomarkers Prev 18:1403-1409, 2009.
5. Tehard B, Lahmann PH, Riboli E, et al: Anthropometry, breast cancer and menopausal status: Use of repeated measurements over 10 years of follow-up-results of the French E3N Women’s Cohort Study. Int J Cancer 111:264-269, 2004.
6. Kwan ML, Kushi LH, Weltzien E, et al: Epidemiology of breast cancer subtypes in two prospective cohort studies of breast cancer survivors. Breast Cancer Res 11(3):R31, 2009.
7. Vona-Davis L, Rose DP, Hazard H, et al: Triple-negative breast cancer and obesity in a rural Appalachian population. Cancer Epidemiol Biomarkers Prev 17:3319-3324, 2008.
8. Phipps AI, Malone KE, Porter PL, et al: Body size and risk of luminal, HER2-overexpressing, and triple-negative breast cancer in postmenopausal women. Cancer Epidemiol Biomarkers Prev 17:2078-2086, 2008.
9. Chlebowski RT, Aiello E, McTiernan A: Weight loss in breast cancer patient management. J Clin Oncol 20:1128-1143, 2002.
10. Enger SM, Greif JM, Polikoff J, et al: Body weight correlates with mortality in early-stage breast cancer. Arch Surg 139:954-960 (incl discussion), 2004.
11. Berclaz G, Li S, Price KN, et al: Body mass index as a prognostic feature in operable breast cancer: The International Breast Cancer Study Group experience. Ann Oncol 15:875-884, 2004.
12. Litton JK, Gonzalez-Angulo AM, Warneke CL, et al: Relationship between obesity and pathologic response to neoadjuvant chemotherapy among women with operable breast cancer. J Clin Oncol 26:4072-4077, 2008.
13. Dawood S, Broglio K, Gonzalez-Angulo AM, et al: Prognostic value of body mass index in locally advanced breast cancer. Clin Cancer Res 14:1718-1725, 2008.
14. Dignam JJ, Wieand K, Johnson KA, et al: Effects of obesity and race on prognosis in lymph node-negative, estrogen receptor-negative breast cancer. Breast Cancer Res Treat 97:245-254, 2006.
15. Verkasalo PK, Thomas HV, Appleby PN, et al: Circulating levels of sex hormones and their relation to risk factors for breast cancer: A cross-sectional study in 1092 pre- and postmenopausal women (United Kingdom). Cancer Causes Control 12:47-59, 2001.
16. Clemons M, Goss P: Estrogen and the risk of breast cancer. N Engl J Med 344:276-285, 2001.
17. Persson I: Estrogens in the causation of breast, endometrial and ovarian cancers: Evidence and hypotheses from epidemiological findings. J Steroid Biochem Mol Biol 74:357-364, 2000.
18. Snedeker SM, Diaugustine RP: Hormonal and environmental factors affecting cell proliferation and neoplasia in the mammary gland. Prog Clin Biol Res 394:211-253, 1996.
19. Del Giudice ME, Fantus IG, Ezzat S, et al: Insulin and related factors in premenopausal breast cancer risk. Breast Cancer Res Treat 47:111-120, 1998.
20. Goodwin PJ, Ennis M, Pritchard KI, et al: Fasting insulin and outcome in early-stage breast cancer: Results of a prospective cohort study. J Clin Oncol 20:42-51, 2002.
21. Daling JR, Malone KE, Doody DR, et al: Relation of body mass index to tumor markers and survival among young women with invasive ductal breast carcinoma. Cancer 92:720-729, 2001.
22. Schapira DV, Kumar NB, Lyman GH, et al: Obesity and body fat distribution and breast cancer prognosis. Cancer 67:523-528, 1991.
23. Daniell HW: Increased lymph node metastases at mastectomy for breast cancer associated with host obesity, cigarette smoking, age, and large tumor size. Cancer 62:429-435, 1988.
24. Maehle BO, Tretli S, Thorsen T: The associations of obesity, lymph node status and prognosis in breast cancer patients: Dependence on estrogen and progesterone receptor status. APMIS 112:349-357, 2004.
25. Nieto A, Lozano M, Moro MT, et al: Determinants of wound infections after surgery for breast cancer. Zentralbl Gynakol 124:429-433, 2002.
26. Vinton AL, Traverso LW, Jolly PC: Wound complications after modified radical mastectomy compared with tylectomy with axillary lymph node dissection. Am J Surg 161:584-588, 1991.
27. Madarnas Y, Sawka CA, Franssen E, et al: Are medical oncologists biased in their treatment of the large woman with breast cancer? Breast Cancer Res Treat 66:123-133, 2001.
28. Griggs JJ, Sorbero ME, Lyman GH: Undertreatment of obese women receiving breast cancer chemotherapy. Arch Intern Med 165:1267-1273, 2005.
29. Abrahamson PE, Gammon MD, Lund MJ, et al: Recreational physical activity and survival among young women with breast cancer. Cancer 107:1777-1785, 2006.
30. Holmes MD, Chen WY, Feskanich D, et al: Physical activity and survival after breast cancer diagnosis. JAMA 293:2479-2486, 2005.
31. Holick CN, Newcomb PA, Trentham-Dietz A, et al: Physical activity and survival after diagnosis of invasive breast cancer. Cancer Epidemiol Biomarkers Prev 17:379-386, 2008.
32. Bianchini F, Kaaks R, Vainio H: Weight control and physical activity in cancer prevention. Obes Rev 3:5-8, 2002.
33. Irwin ML, Varma K, Alvarez-Reeves M, et al: Randomized controlled trial of aerobic exercise on insulin and insulin-like growth factors in breast cancer survivors: The Yale Exercise and Survivorship study. Cancer Epidemiol Biomarkers Prev 18:306-313, 2009.
34. Holmberg L, Norden T, Lindgren A, et al: Pre-operative oestradiol levels - relation to survival in breast cancer. Eur J Surg Oncol 27:152-156, 2001.
35. Lonning PE, Helle SI, Johannessen DC, et al: Influence of plasma estrogen levels on the length of the disease-free interval in postmenopausal women with breast cancer. Breast Cancer Res Treat 39:335-341, 1996.
36. Mutrie N, Campbell AM, Whyte F, et al: Benefits of supervised group exercise programme for women being treated for early stage breast cancer: Pragmatic randomised controlled trial. BMJ 334:517, 2007.
37. Caan BJ, Kwan ML, Hartzell G, et al: Pre-diagnosis body mass index, post-diagnosis weight change, and prognosis among women with early stage breast cancer. Cancer Causes Control 19:1319-1328, 2008.
38. Tao MH, Shu XO, Ruan ZX, et al: Association of overweight with breast cancer survival. Am J Epidemiol 163:101-107, 2006.