2022 Genitourinary Cancers Symposium 2-Minute Drill: Experts Review Most Impactful Data
Thought leaders Daniel P. Petrylak, MD; Benjamin H. Lowentritt, MD; Alan H. Bryce, MD; and Tanya Dorff, MD, joined CancerNetwork® following the 2022 Genitourinary Cancers Symposium to discuss highlights of the meeting in a game show–style production.
In February 2022, leaders in the treatment of genitourinary malignancies gathered for the annual American Society of Clinical Oncology (ASCO) Genitourinary (GU) Cancers Symposium for presentations and discussions of the latest practice-changing research.
Closely following the symposium, CancerNetwork® hosted a game show–style production called 2-Minute Drill, where a live, in-studio moderator posed rapid-fire questions about the meeting to key thought leaders to gauge their outlook on high-level topics.
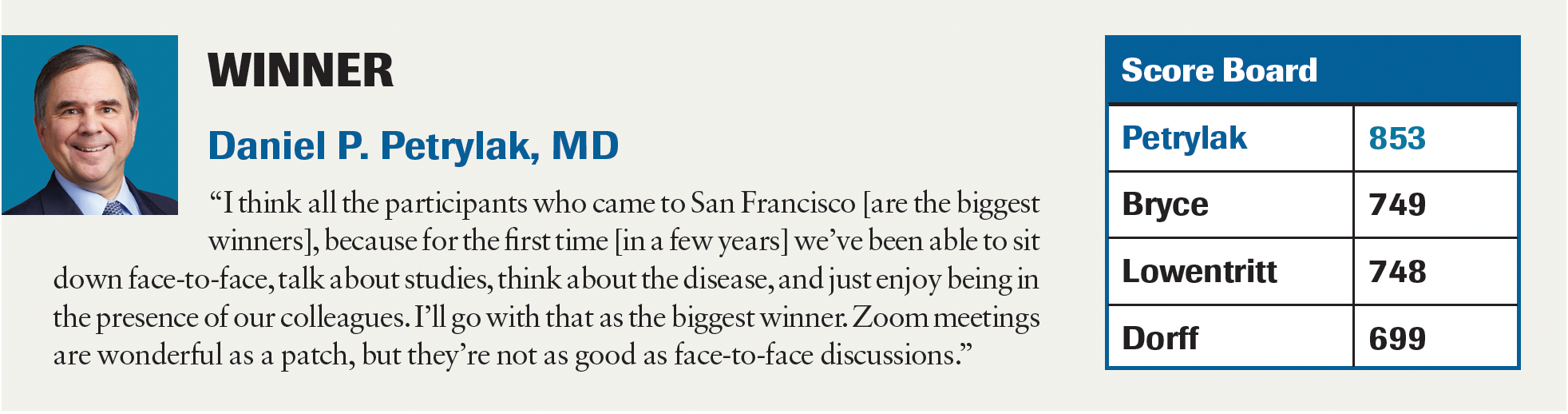
The experts were Alan Haruo Bryce, MD, chair, Division of Hematology/Oncology, Department of Medicine, May Clinic, Phoenix, Arizona; Tanya Dorff, MD, section chief, Genitourinary Disease Program, and associate professor, Department of Medical Oncology & Therapeutics Research, City of Hope, Duarte, California; Benjamin H. Lowentritt, MD, director of Minimally Invasive Surgery and Robotics and the Prostate Cancer Care Program, Chesapeake Urology, Towson, Maryland; and Daniel P. Petrylak, MD, professor of medicine (medical oncology) and urology and coleader of the Cancer Signaling Networks, Yale Cancer Center, New Haven, Connecticut.
The experts agreed that this year’s meeting brought forward a huge number of advancements across all the data presented.

What trial do you think will be the most practice changing?
Dorff on the ARASENS trial (NCT02799602)1
"ARASENS, to me, is immediately practice changing. I’ve been on the fence after the PEACE1 trial (NCT01957436) about whether we need to be adding androgen receptor [AR]–targeted agents on top of up-front docetaxel. But really, the bigger practice change that needs to happen—and this was a call to arms, seeing yet another positive study—[is that] we’ll get the oncology and urology communities energized and motivated to not be doing just castration anymore for [metastatic hormone-sensitive prostate cancer]. I get it—occasionally there’s a very elderly, frail, comorbid patient [who] can just get castration for their first-line therapy. But the majority should be getting doublet therapy, and now there’s a question about triplet therapy. When you looked at some of the real-world data about how many patients are getting intensification up front, there’s been improvement, but we have a long way to go.”
What was the biggest surprise that came out of the 2022 GU Cancers Symposium?
Petrylak on the CYPIDES trial (NCT03436485)2
"The biggest surprise was the activity of ODM-208 in patients with castration-resistant prostate cancer [CRPC]. We’ve all been looking for novel antiandrogens and this is a compound that basically aggregates all steroid synthesis. It was designed to be effective in those patients with AR mutations. I think the biggest surprise was [that] it does hit the target and, in fact, you do see a significant response rate in those patients who have activating mutations—overall about 24%—but you also see responses in those patients who don’t have those mutations. The drug was designed to hit the target, but it’s hitting more than the target. So, to me, that’s the biggest surprise.”
What trial from the symposium will lead to the next FDA approval?
Lowentritt on the MAGNITUDE trial (NCT03748641)3
"When I think of an approval, I think of a drug that we haven’t had access to for prostate cancer. That one new drug will be niraparib [Zejula]. The MAGNITUDE trial will lead to approval for [niraparib]—in the selected patients with HRR [homologous recombination repair] mutations and metastatic CRPC—in combination with abiraterone [Zytiga]. It was powerful study for those patients. Once again, when you have those patients for whom you’re fortunate enough to find an HRR mutation and we want to intensify our treatment, that combination showed a really important difference. I look forward to having the opportunity to use that medication in the appropriate patients. That’s probably our first approval for a new drug.”
What trial requires the most follow-up?
Bryce on the PROpel trial (NCT03732820)4
"We’re going to have to dig into a lot of data very deeply. Some of the data just couldn’t be discussed in the time allowed at ASCO GU, but it came out in the Q&A afterward and in the conversations that many of us had on the sidelines after the fact. There are [remaining] data that we have to see out of PROpel. Overall survival is still pending, and that will be very critical. We really want to know what the survival benefit looks like in the HRR-negative population. We feel pretty good that it will be there in the [HRR-]positive population, but what about for [HRR] negative? A lot of follow-up data [will] come out of that study.”
References
- Smith MR, Hussain MHA, Saad F, et al. Overall survival with darolutamide versus placebo in combination with androgen-deprivation therapy and docetaxel for metastatic hormone-sensitive prostate cancer in the phase 3 ARASENS trial. J Clin Oncol. 2022;40(suppl 6):13. doi:10.1200/JCO.2022.40.6_suppl.013
- Fizazi K, Cook N, Barthélémy P, et al. Phase 1 results of the ODM-208 first-in-human phase 1-2 trial in patients with metastatic castration-resistant prostate cancer (CYPIDES). J Clin Oncol. 2022;40(suppl 6):18. doi:10.1200/JCO.2022.40.6_suppl.018
- Chi KN, Rathkopf DE, Smith MR, et al. Phase 3 MAGNITUDE study: first results of niraparib (NIRA) with abiraterone acetate and prednisone (AAP) as first-line therapy in patients (pts) with metastatic castration- resistant prostate cancer (mCRPC) with and without homologous recombination repair (HRR) gene alterations. J Clin Oncol. 2022;40(suppl 6):12. doi:10.1200/JCO.2022.40.6_suppl.012
- Saad F, Armstrong AJ, Thiery-Vuillemin A, et al. PROpel: phase III trial of olaparib (ola) and abiraterone (abi) versus placebo (pbo) and abi as first-line (1L) therapy for patients (pts) with metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol. 2022;40(suppl 6):11. doi:10.1200/JCO.2022.40.6_suppl.011