Addition of Radiotherapy to Systemic Chemotherapy Improves Survival in ESCC
Although radiotherapy was safe and well tolerated in patients with esophageal squamous cell carcinoma, more research is needed to confirm these results.
Although radiotherapy was safe and well tolerated in patients with esophageal squamous cell carcinoma, more research is needed to confirm these results.
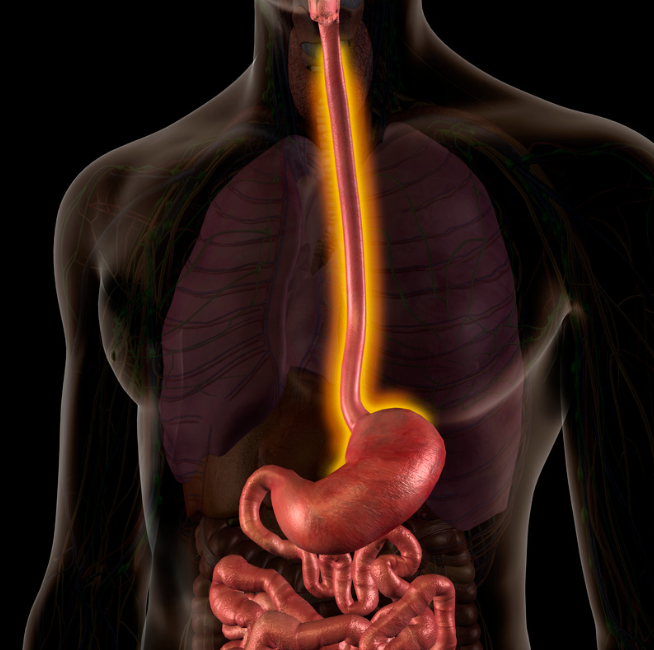
Adding radiotherapy to first-line chemoimmunotherapy significantly improved the survival of Chinese patients with locally advanced or metastatic esophageal squamous cell carcinoma (ESCC) compared with chemoimmunotherapy alone, according to results from the multicenter, retrospective ChinECR trial (NCT06478355) published in Frontiers in Immunology.1
Before propensity score matching (PSM), after a median follow-up of 37.0 months (IQR, 28.3-35.7), patients in the radiation group had significantly longer overall survival (OS; P < .001) and progression-free survival (PFS; P < .001) than in the chemoimmunotherapy alone cohort. Furthermore, OS (P = .015) and PFS (P = .008) remained significantly improved with the radiation group after PSM. The median OS in each respective group was 34 months (95% CI, 27.0-41.0) vs 20 months (95% CI, 17.7-26.3), and the median PFS was 16 months (95% CI, 11.6-20.4) vs 12 months (95% CI, 9.8-14.2).
Additionally, univariate analysis after PSM found factors that particularly affected OS, including age, tumor location, cT, cN, maintenance therapy, and radiotherapy. Furthermore, in the multivariate analysis, independent factors affecting OS and PFS included cN, maintenance therapy, and radiotherapy.
A matched population analysis showed patients could recover from radiotherapy, with a respective OS HR of 0.67 (95% CI, 0.50-0.89; P = .006) and a PFS HR of 0.68 (95% CI, 0.53-0.89; P = .004). Additionally, it showed that immune maintenance therapy was beneficial, with respective OS and PFS HRs of 0.44 (95% CI, 0.30-0.61; P < .001) and 0.72 (95% CI, 0.52-0.99; P = .045).
“According to the research, adding radiotherapy into systemic chemotherapy integrated with immune checkpoint inhibitors significantly improves the prognosis of patients in China who suffer from locally advanced or metastatic esophageal squamous cell carcinoma,” Xinyi Liu, MD, professor in the Department of Radiation Oncology at Hebei Medical University Fourth Hospital in Shijiazhuang, China, wrote in the publication with study coinvestigators.1 “There is a safe combined treatment, and the treatment-related adverse effects are manageable. However, large randomized controlled trials need to be carried out to further confirm those results.”
The retrospective cohort study enrolled patients 18 years or older with stage II to IV ESCC confirmed by bite histopathology across 11 large cancer centers in China who received immunochemotherapy alone (n = 226) or with radiation therapy (n = 438). Both groups of patients underwent platinum-based chemotherapy every 3 weeks for 4 to 6 cycles in the absence of disease progression or unacceptable toxicity based on the investigator’s choice.
Additionally, anti–PD-1 antibodies consisting of sintilimab (Tyvyt), camrelizumab (Airuika), tislelizumab (Tevimbra), or pembrolizumab (Keytruda) were given every 3 weeks until intolerable toxicities, disease progression, or a maximum of 2 years. Immunotherapy received after the sixth cycle was considered immune maintenance therapy.
Radiotherapy was given as x-ray of 6 to 8 MeV employing volumetric modulated arc therapy, intensity-modulated radiotherapy, and tomotherapy. Of 438 patients who underwent radiotherapy, 31 received palliative treatment, receiving 40.0 to 46.9 Gy in 10 to 26 fractions, and 407 received conventional radical treatment at a dose of 50 to 60 Gy in 25 to 33 fractions. The decision to irradiate to distant organ metastases was determined by the attending physician.
Among patients included before PSM in the radiation therapy and control arms, most were male (75.3% vs 75.2%), were younger than 70 years (70.3% vs 67.3%), and had an ECOG performance status of 0 to 1 (88.1% vs 88.1%). In each arm, the most common tumor location was mediastinal (40.9% vs 47.3%), the most common tumor status was T3 to T4 (83.3% vs 82.3%), and the most common node status was N2 (39.7% vs 46.5%). A total of 13.0% vs 20.4%, 2.7% vs 12.4%, 3.7% vs 8.8%, and 1.6% vs 0.4% of each arm had lung, liver, bone, and brain metastases, respectively.
The primary end points included objective response rate and safety.2 Secondary end points included OS, PFS, and disease control rate.
According to the safety analysis, a greater total incidence of esophagitis was observed in the radiation group vs chemoimmunotherapy alone at 22.8% vs 3.6% (P < .001) for any-grade esophagitis and 4.2% vs 0% (P = .015) at grade 3 or 4 severity. For any-grade pneumonia, it was 10.8% vs 3.0% (P = .008), including 1.8% vs 0.6% (P = .623) experiencing it at grade 3 or 4 severity. A total of 5.4% of patients in the radiation group developed esophageal fistula vs none in the control group.
References
- Liu X, Wen J, Zhang Y, et al. Impact of first-line chemoimmunotherapy with or without radiotherapy on the prognosis of patients with locally advanced or metastatic esophageal squamous cell carcinoma: a multicenter, real-world, retrospective cohort study from China (NCT06478355). Front Immunol. Published online July 28, 2025. doi:10.3389/fimmu.2025.1633930
- Immunotherapy combined with chemoradiotherapy for first-line treatment of esophageal squamous cell carcinoma (ChinECR). ClinicalTrials.gov. Updated June 3, 2025. Accessed August 21, 2025. https://tinyurl.com/y2czh7cv