After Lung Cancer Progression, Gefitinib Provides No Benefit
Continuing gefitinib after acquiring resistance to the TKI adds no clinical benefit in patients with EGFR-positive non-small-cell lung cancer, according to trial results presented at the 2014 ESMO Congress.
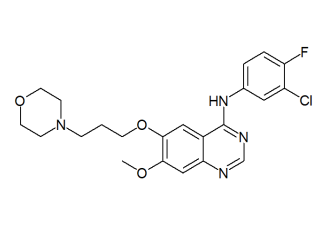
Chemical structure of gefitinib
Continuing therapy with gefitinib after acquiring resistance to the EGFR tyrosine kinase inhibitor adds no clinical benefit in patients with EGFR mutation-positive non–small-cell lung cancer (NSCLC), according to results of a new phase III trial. The results show that chemotherapy doublet therapy alone should be the standard of care in these patients.
“This study was designed to resolve a greatly debated issue: whether tyrosine kinase inhibitors should be continued beyond progression,” said the IMPRESS study’s lead author Tony Mok, MD, of the Chinese University of Hong Kong, in a press release. He said that he and his co-authors “suspected the inhibition of TKI-sensitive cancer cells with continuation of gefitinib and inhibition of resistant cells with chemotherapy would optimize the treatment outcome. However, the study has proved otherwise.”
The IMPRESS trial included 265 patients from 71 centers with locally advanced or metastatic NSCLC with an activating EGFR mutation and prior progression on first-line gefitinib. Patients received cisplatin and pemetrexed chemotherapy with either gefitinib (133 patients) or with placebo (132 patients). Progression-free survival was no different between these groups, at a median of 5.4 months in each group for a hazard ratio (HR) of 0.86 (95% CI, 0.65-1.13; P = .273).
Though overall survival data was immature with 33% of the cohort dying, the results suggested better overall survival with placebo vs gefitinib with an HR of 1.62 (95% CI, 1.05-2.52; P = .029). There were no differences with regard to response rates or disease control rates.
Gefitinib patients experienced more grade 1/2 gastrointestinal toxicities. The most common adverse events were nausea (64% with gefitinib, 61% with placebo) and decreased appetite (49% gefitinib, 34% placebo). Two adverse events with outcome of death were reported in the gefitinib group, compared with one in the placebo group.
Mok concluded that the lack of clinical benefit seen with continued gefitinib establishes doublet chemotherapy as the standard of care for these patients. Marina Garassino, MD, of the National Cancer Institute of Milan in Italy, was the discussant for the session and called the results “very robust and reliable.” She did note that when possible, performing a re-biopsy on patients upon progression could help understand the mechanisms of resistance.
“New generations of agents are now becoming available for specific resistance mutations with very promising results,” she said. “It is therefore possible in the future that we will be able to personalize the further treatments for these patients.”