Age Threshold for Hereditary Mutation Testing in Kidney Cancer
Individuals diagnosed with kidney cancer at age 46 or younger are more likely to have hereditary disease, according to a new study.
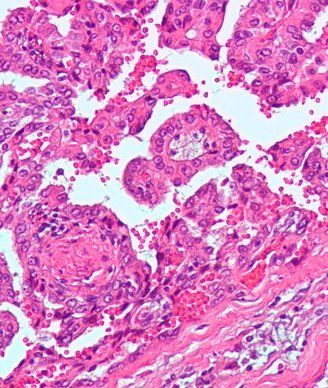
Micrograph of papillary renal cell carcinoma. Copyright 2009 Nephron.
Individuals diagnosed with kidney cancer at a relatively young age are more likely to have hereditary renal cell carcinoma (RCC). According to a new study published in the Journal of Clinical Oncology, any patient who is diagnosed with kidney cancer at age 46 or younger should consider genetic counseling and germline mutation testing.
There are currently no age-specific cutoffs for selecting individuals who should consider germline mutation testing for kidney cancer or guidelines to identify those who should be tested as there are for breast and colon cancers-cancers associated with specific germline mutations that confer individuals with a higher risk of developing these cancers.
In the current study, records of individuals diagnosed with sporadic and hereditary RCC using the SEER-17 program and the researchers institutional hereditary kidney cancer population were analyzed. The authors found that the median age of presentation for hereditary RCC is 27 years younger than that observed in the general population.
These new results suggest that diagnosis at the age of 46 could be a useful cut-off point for the establishment of genetic testing guidelines, according to the authors. This 10th percentile threshold maximized sensitivity and specificity while minimizing the number needed to test.
Genome-wide studies over the past 2 decades have shown that genetic predisposition to specific cancers may be more prevalent than was previously supposed, particularly combinations of loci that together confer an increased risk for a specific cancer. Mutations that confer risk of developing colon and breast cancers as well as more rare cancers such as retinoblastoma have been well defined and have guidelines in place.
But, as W. Marston Linehan, MD, of the urologic oncology branch at the National Cancer Institute and colleagues describe, as many as 5% to 8% of the 55,000 renal cell carcinomas diagnosed in the United States every year are estimated to be hereditary, and this may be an underestimation as many patients do not undergo genetic testing.
There are several hereditary RCC syndromes including von Hippel-Lindau syndrome and hereditary papillary renal cell carcinoma that are associated with germline mutations, but patients may be diagnosed with RCC without being assessed for an underlying syndrome as such diagnosis can be challenging.
According to the authors, the factors known to be associated with hereditary RCC include a family history of RCC, renal masses that are bilateral or multifocal, clinical signs of RCC hereditary syndromes, and specific renal tumor histologies.
In the current study, the median age of patients in the SEER database was 64 years (mean of 63.4 years). The mean age of men and women at diagnosis were 62.9 years and 64.3 years, respectively (P < .001). Estimates of the 25th, 10th, and 2.5th percentiles were 54, 46, and 36 years, respectively. White and Asian patients had a slightly older age at onset of disease (63.9 and 62.6 years, respectively) compared with black and Native American patients (age 60.7 and 60.3 years, respectively; (P < .001). Although the age of onset varied by sex, race, and histology, these factors were not considered to be clinically relevant for the genetic guidelines since these did not alter the age percentiles.
Among the 608 patients in the hereditary RCC group, the median age of onset was 37 (mean age of 39.2).
Current genetic testing is moving to gene panel testing and whole-exome sequencing. However, authors emphasize, that this type of testing may be difficult to interpret, particularly understanding which mutations are disease-associated and which are genetic variants. All patients who may have hereditary RCC should seek out an experienced genetic counseling team to advise patients.
“When clinicians encounter individuals with early-onset kidney cancer (age 46 years or younger), they should strongly consider referral for genetic counseling/germline mutation testing,” conclude the authors.
Prospective studies of age-based screening to validate the age-cut off identified in the current study are currently ongoing.