Amivantamab Is Preferred First-Line Pick in EGFR Exon 20 NSCLC
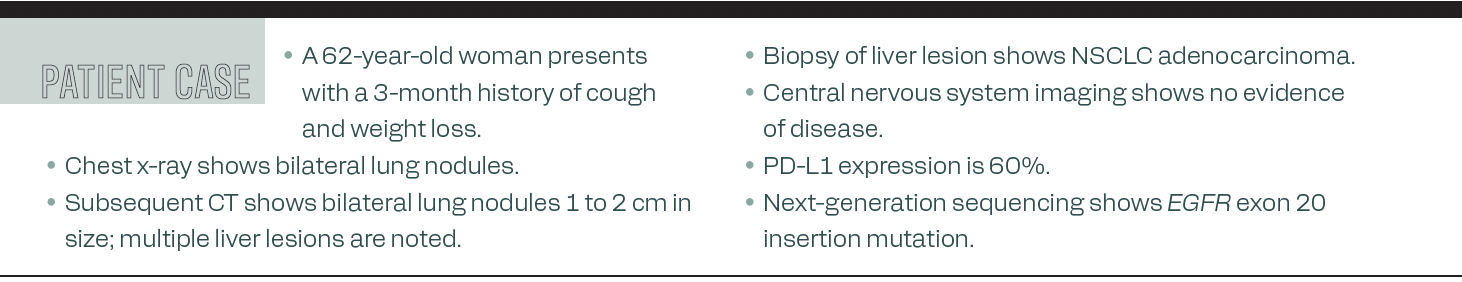
During a Training Academy focused on first-line treatment use in non–small cell lung cancer, panelists discussed a patient case and how they would treat that patient in the setting.
Meet the Experts
During a Training Academy focused on first-line treatment use in non–small cell lung cancer (NSCLC), panelists discussed a patient case and how they would treat that patient in the setting. They also spoke about genetic testing, adverse effect management, and how to educate nurses to best treat patients during infusions.
The patient case
Patel / I’d love to hear how you would handle this scenario in the clinic given some of the recent updates and data.
Spira /I’m typically trying to wait as long as I can. It’s the classic issue we all have as we’re getting the tissue back and we’re testing for the EGFR mutation. I’m waiting for that to come back. To have those results, the [PD-L1] test usually comes back earlier. We typically do a full next-generation sequencing panel on all patients. We’re getting the entire thing with [a PD-L1 test] as well as all the mutations back. It takes on average approximately 2 weeks. I do realize that there is a delay in when the patients come see us. The patients have already been waiting. That delay is tough, but that’s how I generally do it.
Rodriguez /On our end, we do [perform] liquid and tissue testing so at least we get some information early from the liquid biopsy, and most patients can wait 7 days. In other cases where patients already have waited weeks to see us in academic centers, there are sometimes longer waits, and in patients who are sick and need treatment, we have done a cycle of chemotherapy before getting the full genetic information. In the ideal scenario, yes, you will do either concurrent liquid or tissue [testing] so you get all the information you need to make the best decision for the patient.
Bestvina /We also have been sending concurrent testing on almost all patients with a new diagnosis. It allows for faster turnaround times and better comprehensive testing. We’ve seen when patients get concurrent testing, you may pick up some patients with actionable alterations on liquid vs biopsy [testing] vs doing both. It does take a lot to counsel patients on why it’s so important to wait for the results, but as long as the patient isn’t very symptomatic, we will wait for those results to come back prior to starting therapy.
Patel / It’s a great point. This is a great window if you have to use radiation and also if you have to give systemic treatment vs chemotherapy alone, and holding the immunotherapy until you have the molecular information. Given some of the recent advances, what would be your systemic treatment choice?
Bestvina /We saw the phase 3 PAPILLON [NCT04538664] study presented, which looks at frontline amivantamab-vmjw [Rybrevant] plus chemotherapy for patients with EGFR exon 20 mutations.1 This is something that I’ve already adopted in my clinic. We saw an impressive improvement in progression-free survival in the patients who received amivantamab plus chemotherapy, to 11.4 months from 6.7 months with chemotherapy alone. To me, this is a practice-changing study.
Rodriguez /When you have data that show an improvement in progression-free survival for patients and an improvement in how they live with this disease, they can have better responses in the brain. It is imperative for us to start the best treatment up front because we don’t know how things will evolve, so I feel that having this combination will cover all your bases up front, and it’s a little different from when we were using the treatment by itself as a second-line option. We have to learn the new regimen and teach [clinicians] to do that and manage new toxicities.
Spira /[I have very] little to add. I think everybody said this very well. One of the things that we always have to think about—and this has to do not just with this but, as you look at the phase 3 FLAURA2 [NCT04035486] and phase 3 MARIPOSA [NCT04487080] trials—although you have improved outcomes, what’s the trade-off? Especially when you’re adding a third drug, there’s increasing toxicity, and that may weigh on some [patients]. Because patients are already getting chemotherapy, I view that as the hard part. This is just the addition of a targeted therapy. I’m always humbled because I always have to remember that no matter how smart we think we are, only approximately 50% to 60 % of [patients] get to that second line of therapy. If you don’t give them their best option up front, they may not get there. You can wave some of that off if the drug is very toxic or has limited benefit, but I think we all agree that these targeted therapies and amivantamab are no different from any of the other ones and do work very well. For me, I’m going to want to give that to everybody. They’ll probably be the 90-year-old patient who may not be able to do [many] things, but with the current standard of care, I’m giving this to pretty much everybody.
Patel / How do you counsel patients on toxicities, including infusion-related toxicities? Dr Spira, in your clinic, what does counseling look like? Because not all targeted therapies are equal in terms of the toxicity profile.
Spira /That’s daunting for patients who are trying to live normal lives. I’m a little more reactive. If you can be proactive and show that there’s a benefit, I might consider that for certain [patients]. I do talk to them about a rash, skin toxicity, etc. We see our patients back a few weeks after starting. We have a good window to monitor this as well.
Bestvina /In our group, we have taken an approach to using prophylactic doxycycline following the gastrointestinal [adverse effects]. That first visit where you’re talking about therapies is very overwhelming. A lot of that comes with counseling the patient on the scheduling. One of the big things with amivantamab is that it’s given so frequently up front. You start with day 1, day 2, and day 8, and when a patient is newly starting therapy, this can be a little bit overwhelming. As long as the patients are aware that the scheduling frequency is going to go down with time, it’s that up-front cost and that up-front [reaction to] being in therapy. They find it more tolerable knowing that eventually it’s going to be just an every-3-weeks regimen.
Patel / How do you handle counseling between the patient and the caregiver, and how do you educate the nurses?
Rodriguez /We did some in-service to train [the nurses]. This is a little similar to rituximab [Rituxan], in that you are going to see an antibody that may cause an infusion reaction, [so] you will need to premedicate patients with antihistamines, glucocorticoids, and [acetaminophen] because they may get hives and [other] reactions. On the first day, 65% of patients had that type of reaction, different levels. On the second day, they rarely had it. The patient needs to know going into it that there might be a reaction to that first treatment. The nurses need to know that they have seen these types of reactions with other drugs and they know how to [handle] it. They’re prepared to give medications as needed, and they can carry patients through the treatment. Very few patients had to discontinue drugs because of infusion reactions.
[The] messages are that they need to be prepared for it, give the premedications up front, and make sure the patient is aware of this. The nurses need to feel confident that they have managed this and that it is similar to other drugs they have [administered] in the past. With that, we’re able to get patients through it all the time. On the second day, any subsequent treatments are rarely going to see any infusion reaction.
Reference
FDA approves amivantamab-vmjw for EGFR exon 20 insertion-mutated non-small cell lung cancer indications. FDA. March 1, 2024. Accessed May 13, 2024. https://tinyurl.com/msw4u5yk
