Anemia Decreases Survival in Women With HIV Infection
ORLANDO-A multicenter, prospective study has shown that anemia is an independent risk factor predicting decreased survival in HIV-infected women and that highly active antiretroviral therapy (HAART) helps resolve anemia in this population group.
ORLANDOA multicenter, prospective study has shown that anemia is an independent risk factor predicting decreased survival in HIV-infected women and that highly active antiretroviral therapy (HAART) helps resolve anemia in this population group.
Alexandra M. Levine, MD, chief, Division of Hematology, and medical director, USC/Norris Cancer Hospital, reported the results at a poster session of the 43rd Annual Meeting of the American Society of Hematology (abstract 2091).
Independent Risk Factor
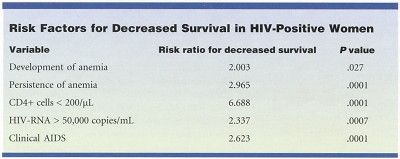
"When you look at all the known risk factors for decreased survivalsuch as low CD4 cell counts, high HIV RNA levels, or history of clinical AIDSthen add anemia into that mix, it turns out that anemia as an independent risk factor is equally important," Dr. Levine said (see Table).
Study participants included 2,054 HIV-positive women and 568 HIV-negative controls in the National Institutes of Health-sponsored Women’s Interagency HIV Study. Anemia was defined as a hemoglobin level of less than 12
g/dL. Patients were followed for 4 years, from 1994 to 1998.
More than half (56%) of the HIV-positive subjects were black. Overall, in the United States, more black women than white women are HIV positive.
Dr. Levine noted that HIV-infected women are statistically more likely to be anemic than HIV-infected men and that regardless of HIV status, black women are more likely than white women to suffer from anemia. The new study found that HIV-positive women are significantly more likely than HIV-negative women to be anemic (P < .001). On multivariate analysis, factors associated with anemia in HIV-infected women in this study were self-reported history of clinical AIDS condition, CD4+ cell counts less than 200/µL, serum HIV-RNA counts greater than 50,000 copies/mL, current use of zidovudine (AZT, Retrovir), mean corpuscular volume (MCV) less than 80 fL, and African-American ethnicity.
In the HIV-positive women who were not anemic at baseline, use of zidovudine was associated with the development of anemia over time, Dr. Levine said. Other factors linked to the development of anemia in these women werea decline in CD4+ cells from more than 200 to less than 200/µL, an increase in plasma HIV-RNA levels from less than to more than 50,000 copies/mL, a decrease in MCV to less than 80 fL, and a clinical diagnosis of AIDS.
HAART was the only factor independently associated with increased survival. In HIV-positive women anemic at the start of the study, use of HAART for 12 months or more aided in its resolution. The drug regimen also protected against the development of anemia in HIV-positive women with normal hemoglobin levels at baseline when used for 18 months or more.
Future Research
"Our findings indicate that use of HAART is associated with improvement in anemia," Dr. Levine said. "By treating the underlying HIV disease, one can correct the anemia."
Dr. Levine’s plans for future research in this area include a review of how individual physicians differed in their treatment of the women’s anemia and how other hematologic parameters, such as low platelet count and low white blood cell count, influence the patient’s prognosis.