CAD Equivalent to Double-Read Mammogram Screening
CHICAGO-Two studies presented at the 87th Scientific Assembly and Annual Meeting of the Radiological Society of North America (RSNA) indicate that computer-aided detection (CAD) of lesions on conventional mammography studies is comparable to double-read mammograms, and it produces fewer false-negative results.
CHICAGOTwo studies presented at the 87th Scientific Assembly and Annual Meeting of the Radiological Society of North America (RSNA) indicate that computer-aided detection (CAD) of lesions on conventional mammography studies is comparable to double-read mammograms, and it produces fewer false-negative results.
Robert A. Schmidt, MD, associate professor of radiology, New York University Medical School, assessed the ability of CAD to find lesions radiologists commonly overlook. In this study (abstract 1001), radiologists participating in a continuing medical education program as well as three expert readers were asked to interpret copies of 100 screening mammograms.
The films contained 50 biopsy-proven cancers in 45 patients and 55 benign or normal cases. Only 49 original mammograms were available. Both those 49 original films and the 100 copies were digitized and analyzed by version 2.2 of the ImageChecker (R2 Technology, Los Altos, California).
Radiologists were told to grade mammograms as normal or abnormal, then characterize every abnormal lesion that was BI-RADS 3 or higher. A mark by a radiologist was labeled correct if it was within a distance of no more than one third of the breast dimension from the actual location of a lesion.
"We were much more stringent on the computer marks," Dr. Schmidt said. A mark by the CAD system that was within 1 lesion width or less of an abnormality was considered to be positive, and CAD had to mark the correct lesion type (mass or calcification).
There was wide variability among the radiologists in the accuracy of their interpretations. "Some radiologists were relatively low in performance, and some beginners were better than experts," Dr. Schmidt observed.
Overall, the general radiologists detected 70% of the cancers, and the experts detected 81%. The CAD system marked 80% of the cancers in both original and copy films, Dr. Schmidt said.
The researchers looked specifically at the 14 lesions missed by more than 50% of the radiologists. These included one calcification and 13 masses, distortions, or asymmetries. Only 36% of the radiologists found these 14 abnormalities. CAD correctly detected 64% of them.
Seven lesions were seen on only one view, a common reason why radiologists overlook mammographic abnormalities. Radiologists in the study, on average, detected these lesions only 40% of the time; the experts found them 60% of the time; and CAD identified them 70% of the time. Four of the 14 lesions missed by more than 50% of the radiologists were seen on only one view. CAD detected all four of these lesions, but it only marked the cancer and nothing else. "There were no false positives," Dr. Schmidt said.
The researchers estimated the theoretical improvement in sensitivity from use of CAD in the identification of the 14 lesions that were missed by more than 50% of radiologists. Dr. Schmidt said there was "a potential maximum improvement of about 11% for all 100 radiologists, and about 7% for the experts, which is similar to what we see in double-reading studies." If all 50 cancers are analyzed, the potential maximum improvement becomes 28% for all 100 radiologists and 17% for the experts.
An analysis of CAD in a double-read screening mammography center in Rochester, NY, found that CAD can decrease the number of false-negative interpretations by about 71%, said Stamatia V. Destounis, MD, assistant clinical professor, Elizabeth Wende Breast Clinic (abstract 998).
Physicians at the clinic see more than 60,000 patients a year; 15,000 undergo diagnostic mammography and 45,000 have mammographic screening. More than 94% of patients return for screening mammograms, so most women with false-negative results return for follow-up, she said.
All Mammograms Double-Read
All mammograms are double-read by two different radiologists. Studies are interpreted online independently, but the second reader typically knows the results of the interpretation made by the first reader.
During 2000, 519 biopsy-proven cancers were detected by the double-read mammography program at the clinic; 328 were found during diagnostic mammography and 191 during screening.
All five mammogram readers in the clinic reviewed prior films from every year 2000 case of cancer, with agreement by three of the five required for a case to be considered a false negative. In 2000, 52 (10%) of the 519 cancers were judged to be detectable in a previous film.
Mammograms from all 52 of these cases were subjected to CAD using the R2 Technology ImageChecker. CAD was considered to be accurate if the system marked the proper location of a lesion and distinguished whether it was a mass or a microcalcification.
Of 43 false-negative screening examinations showing a mass or microcalcification, CAD marked 30 in the previous year and 35 in the current year. "It marked 70% of the cancers a year before we found them, and 81% of the cancers the year that we found them," Dr. Destounis said. CAD identified in prior films 7 of 8 microcalcifications, 19 of 29 masses, 7 of 9 architectural distortions, and 4 of 6 masses with microcalcification.
An Example
Radiologists at the clinic detected a spiculated mass in one patient in the year 2000. CAD not only marked the lesion in the 2000 films but also flagged a mass density in 1999. The radiologists missed the spiculated mass, which was more subtle in 1999 mammograms (see Figure below).
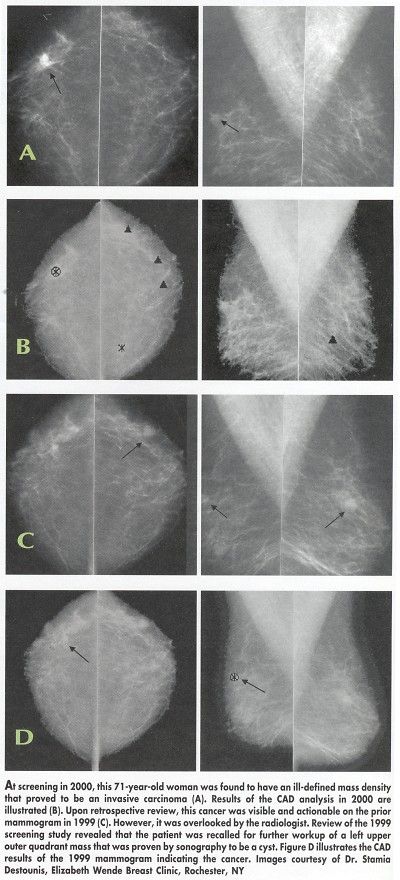
"We were busy concentrating on a smooth outlined mass that turned out to be a cyst, but missed the cancer," Dr. Destounis said. CAD, however, ignored the cyst and marked only the cancer.
Targeted Therapy First Strategy Reduces Need for Chemotherapy in Newly Diagnosed LBCL
December 7th 2025Lenalidomide, tafasitamab, rituximab, and acalabrutinib alone may allow 57% of patients with newly diagnosed LBCL to receive less than the standard number of chemotherapy cycles without compromising curative potential.