Anito-Cel Shows Early Activity, Safety in R/R Multiple Myeloma
Treatment with anito-cel produces deep, enduring responses in high-risk relapsed/refractory multiple myeloma, says Matthew Frigault, MD.
“I think it’s rather impressive that we can actually see that high response rates are maintained across all high-risk groups, whether we look at it as a composite end point or we look at it as EMD, high-risk cytogenetics, or older patients," according to Matthew Frigault, MD.
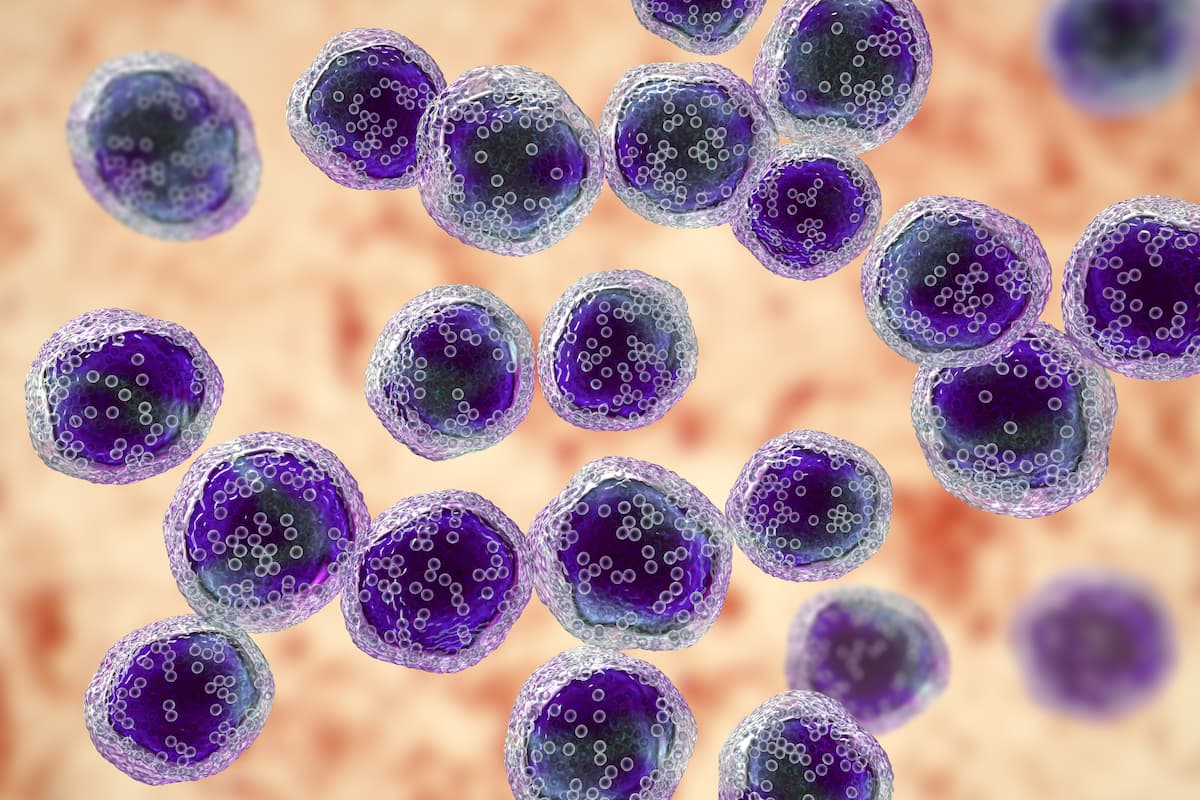
Administering anitocabtagene autoleucel (anito-cel), formerly known as CART-ddBCMA, to patients with relapsed/refractory multiple myeloma produced early activity and manageable safety, even among those with high-risk features, according to findings from a phase 1 study (NCT04155749) presented during the 2023 American Society of Hematology (ASH) Annual Meeting and Exposition.
At a median follow-up of 26.5 months (range, 14-44), the investigator-assessed overall response rate (ORR) was 100% by 2016 International Myeloma Working Group criteria with the autologous BCMA-directed CAR T-cell therapy in the total evaluable population (n = 38); this included a complete response (CR)/stringent complete response (sCR) rate of 76%.
Notably, the CR/sCR rates were greater than 80% in all subgroups assessed. In the high-risk subset (n = 24), defined as having extramedullary disease (EMD), stage III disease per International Staging System (ISS) criteria, and a bone marrow plasma cell (BMPC) percentage of 60% or higher, the CR/sCR rate was 83%. In the subset of patients with EMD (n = 13), the CR/sCR rate was 85%. In those with high-risk cytogenetics (n = 11) and those aged 65 years or older (n = 20), the CR/sCR rates were 82% and 85%, respectively.
In all patients, the median progression-free survival (PFS) had not yet been reached. At a median follow-up of 26.5 months (range, 15-44) in those who achieved a CR/sCR, the median PFS was also not yet reached. The PFS rates at 6, 12, 18, and 24 months were 92.1% (95% CI, 77.5%-97.4%), 75.9% (95% CI, 58.7%-86.6%), 63.7% (95% CI, 45.7%-77.2%), and 56.0% (95% CI, 37.3%-71.1%), respectively. Eighty-nine percent of the total evaluable patients achieved minimal residual disease (MRD) negativity at a minimum of 10-5 sensitivity.
“Our median PFS, duration of response, and overall survival have not been reached with 2 years of follow-up and a median follow-up of 26.5 months, and so it appears that we’re able to have sustained deep and durable responses in a high-risk patient population,” Matthew Frigault, MD, administrative director of Cellular Therapy Service at Massachusetts General Hospital and an assistant professor of medicine at Harvard Medical School in Boston, said in a presentation on the data.
Anito-cel utilizes a D domain, which is a highly stable protein. The small D-domain construct enables high transduction efficiency, CAR positivity, and CAR density on the T-cell surface. Stability at and beyond physiologic conditions is facilitated through quick D-domain folding, lack of disulfide bonds, and a hydrophobic core.
Prior research has indicated that the agent has “very low tonic signaling, which has been shown to be favorable in CAR T-cell constructs, and because of that, …we see a pretty high and uniform expression on the cell surface, with a median transduction efficiency of around 70% with less than 2 average integrations per given cell—so, a very highly stable protein,” Frigault explained. “What we think is happening here is that this multiple kind of binding per cell could potentially be beneficial for overall efficacy.”
The open-label, multicenter, first-in-human, phase 1 trial enrolled patients with relapsed or refractory multiple myeloma who received at least 3 previous lines of systemic treatment, including an immunomodulatory drug, a proteasome inhibitor, and an anti-CD38 monoclonal antibody.2 They were also eligible if they had triple-refractory disease. Other inclusion criteria included an ECOG performance status of 0 or 1 and acceptable organ function.
Study participants received lymphodepleting chemotherapy in the form of fludarabine at 30 mg/m2 and cyclophosphamide at 300 mg/m2 on days –5, –4, and –3 before infusion with anito-cel. The following 2 dose levels were examined in each dose-escalation cohort: 100 ± 20% x 106 CAR+ cells (dose level 1; DL1) or 300 ± 20% x 106 CAR+ cells (dose level 2; DL2).1
“We elected to move forward with an expansion cohort at DL1, with a median cell dose of 115 million cells,” Frigault noted. “…I will say that we were able to manufacture at least 3 doses at DL1 for every single patient that was enrolled on study.”
A total of 40 patients were enrolled on the study and underwent leukaphereses. Anito-cel was successfully manufactured for all patients although 1 patient discontinued prior to receiving lymphodepletion due to infection. An additional patient discontinued after lymphodepletion due to hypoxia or heart failure. As such, a total of 38 patients were dosed with the CAR T-cell therapy; of these patients, 32 received the product at DL1, including in the expansion, and 6 received it at DL2.
The data reported at the meeting were a summary of safety and efficacy in all patients dosed at both DL1 and DL2.
In the 38 patients, the median age was 66 years (range, 44-76) and 61% were male. Most patients had an ECOG performance status of 1 (68%).
Sixty-three percent of patients had high-risk prognostic features, which included BMPC of at least 60% (24%), ISS stage III disease (18%), and EMD (34%). “I’ll point out that this EMD is not what some have called paramedullary disease, but true soft tissue involvement of the liver, lung, parenchyma pleura, as opposed to plasmacytomas that are actually growing out of the bone or near the bone,” Frigault said. He added that these 3 factors “have actually been retrospectively shown in pivotal studies and other real-world series to be detrimental to overall prognosis.” Twenty-nine percent of patients had high-risk cytogenetics.
The median number of prior lines of treatment received was 4, with a range of 3 to 16 lines. All patients had triple-refractory disease and 68% had penta-refractory disease. Additionally, the majority of patients (89%) were refractory to their last line of treatment. Sixty-eight percent of patients received bridging therapy and 76% previously underwent transplant.
“I think the exciting thing here is that we had an 100% ORR in the 38 patients who were infused,” Frigault said. “I think it’s rather impressive that we can actually see that high response rates are maintained across all high-risk groups, whether we look at it as a composite end point or we look at it as EMD, high-risk cytogenetics, or older patients.”
Additional data showed that at a median follow-up of approximately 33 months (range, 14-44) in the subgroup of patients with EMD (n = 13), the median PFS was not yet reached. The PFS rates at 6 and 12 months were 92.3% (95% CI, 56.6%-98.9%) and 67.1% (95% CI, 34.2%-86.2%); at 18 months and 24 months, these rates were 67.1% (95% CI, 34.2%-86.2%) and 57.5% (95% CI, 25.7%-79.9%), respectively. At a median follow-up of approximately 25 months (range, 15-40) in non-EMD patients (n = 25), the median PFS was also not yet reached.
“Notably, at this 33-month time point, we actually haven’t met our median PFS for the EMD cohort, which I think is hopefully promising for improvements in the overall population as time goes on [in terms of] less high-risk patients,” Frigault noted.
In those with high-risk cytogenetics, the Kaplan-Meier estimated PFS rates at 6, 12, 18, and 24 months were 81.8% (95% CI, 44.7%-95.1%), 71.6% (95% CI, 35.0%-89.9%), 71.6% (95% CI, 35.0%-89.9%), and 71.6% (95% CI, 35.0%-89.9%), respectively. In those aged 65 years or older, the Kaplan-Meier estimated PFS rates were 95.0% (95% CI, 69.5%-99.3%), 85.0% (95% CI, 60.4%-94.9%), 74.3% (95% CI, 48.7%-88.4%), and 61.3% (95% CI, 34.9%-79.7%), respectively. In all risk subgroups, the estimated median PFS had not yet been reached at 24 months.
“We’ll continue to have longer follow-up to follow these patients and get more mature data,” Frigault said.
The safety profile of anito-cel, particularly with regard to cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS), aligned with what has previously been presented with the agent.
Of those in DL1, grade 1 or 2 CRS was reported in 94% of patients; no grade 3 CRS was reported in this group. The median onset was 2 days (range, 1-12) and the median duration was 6 days (range, 1-10). In the DL2 cohort, grade 1 or 2 CRS was reported in 83% of patients; 1 patient experienced a grade 3 event. Here, the median onset was 2 days (range, 1-2) and the median duration was 5 days (range, 3-9).
Grade 1 or 2 ICANS occurred in 16% of patients in the DL1 cohort; 1 patient experienced a grade 3 event. The median onset was 4.5 days (range, 3-6) and the median duration was 3.5 days (range, 1-9). In the DL2 cohort, only 1 grade 3 ICANS event occurred. For this patient, the median onset was 7 days, and the median duration was 17 days.
These toxicities were managed by tocilizumab (Actemra) in 84% of those in the DL1 cohort and 83% of those in the DL2 cohort and dexamethasone for 63% and 33% of patients, respectively.
The most common grade 3 or 4 adverse effects (AEs) that occurred in at least 5% of all patients following infusion with anito-cel included decreased neutrophil count (81.6%), anemia (57.9%), thrombocytopenia (42.1%), decreased lymphocyte count (39.5%), decreased white blood cell count (18.4%), febrile neutropenia (13.2%), hypertension (7.9%), increased aspartate aminotransferase (5.3%), cellulitis (5.3%), hypokalemia (5.3%), hyponatremia (5.3%), hypophosphatemia (5.3%), lung infection (5.3%), pain in the extremities (5.3%), and sepsis (5.3%).
“I think notably, and important here, is that we have not seen any delayed movement disorders, Parkinson-like syndrome, or atypical neurotoxicity [in the entire population through the follow-up period],” Frigault said. No Guillain-Barré syndrome or cranial palsies have been observed either.
One grade 5 AE occurred after study treatment, but it was determined to be unrelated; this patient experienced cardiac arrest due to non-study drug overdose.
Frigault concluded by saying that the pivotal phase 2 IMMagine-1 trial (NCT05396885), which will further evaluate the safety and efficacy of anito-cel is currently enrolling patients with relapsed or refractory multiple myeloma.
Editor’s Note: Frigault disclosed that research funding was received by Kite, Novartis, and Arcellx. He also serves in a consultancy role for Bristol Myers Squibb, Novartis, and Covance.
Reference
Frigault MJ, Rosenblatt J, Dhakal B, et al. Phase 1 study of CART-Ddbcma for the treatment of patients with relapsed and/or refractory multiple myeloma: results from at least 1-year follow-up in all patients. Blood. 2023;142(suppl 1):1023. doi:10.1182/blood-2023-189761
Maintenance Tucatinib Combo Yields PFS Extension in Advanced HER2+ Breast Cancer
December 11th 2025“HER2CLIMB-05 has demonstrated that the addition of tucatinib to HP represents an enhanced frontline maintenance therapy option for patients with HER2-positive metastatic breast cancer,” said Erika Hamilton, MD.