Antitumor Activity Seen With Olverembatinib in GIST Subtype
Olverembatinib has shown promising clinical efficacy in SDH-deficient gastrointestinal stromal tumors, says Haibo Qiu, MD.
"Olverembatinib has shown promising clinical efficacy in SDH-deficient GIST," according to Haibo Qiu, MD, of Sun Yat-sen University Cancer Center, in Guangzhou, China.
Antitumor activity in patients with succinate dehydrogenase (SDH)-deficient gastrointestinal stromal tumors (GISTs) and paraganglioma resistant to tyrosine kinase inhibitors (TKIs) was achieved with olverembatinib (HQP1351), according to data from a phase 1 study (NCT03594422) presented at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting.1
In the open-label, multicenter study—defined as the largest global, prospective clinical trial evaluating a TKI for SDH-deficient GISTs completed to date—olverembatinib elicited an overall response rate (ORR) of 23.1% (n = 26), which consisted of 6 partial responses (PRs). The clinical benefit rate was 92.3%, and 24 patients had PR or stable disease for longer than 16 weeks, or 4 cycles. The median duration of treatment for patients was 15.6 months (range, 1.8-42.3).
"Olverembatinib has shown promising clinical efficacy in SDH-deficient GIST," Haibo Qiu, MD, of Sun Yat-sen University Cancer Center, in Guangzhou, China, said in a presentation of the data.
SDH-deficient GIST, a subtype of wild-type GIST, comprises an estimated 10% of GIST diagnoses. This population currently is an unmet medical need, as most studied treatments have limited efficacy in those with SDH-deficient GIST. Furthermore, no novel therapies have shown responses in SDH-deficient GIST, and no preferred treatment regimen in this subgroup exists.
Olverembatinib targets multiple kinases including BCR-ABL, KIT, SRC, FGFR, and PDGFRA. It is currently approved in China for the treatment of patients with TKI-resistant chronic-phase CML and T315I-mutated accelerated phase CML, as well as for the treatment of adult patients with chronic-phase CML resistant to and/or intolerant of first- and second-generation TKIs.2
Preclinical models have shown potent antiproliferative activity with olverembatinib in TKI-resistant GIST cell lines.
At the 2023 ASCO Annual Meeting, Qiu and investigators shared preliminary data investigating olverembatinib in TKI-resistant metastatic SDH-deficient GISTs, resulting in a clinical benefit rate of 93.8% and 5 PRs; the agent was also found to be well tolerated.3,4
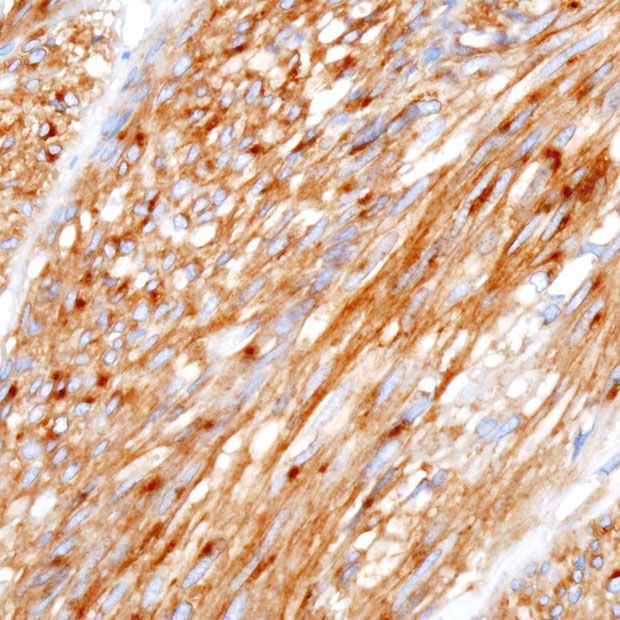
In the phase 1 study, investigators evaluated the safety and efficacy of olverembatinib in patients with advanced or metastatic GIST, as well as other solid tumors, without appropriate treatment.1 Eligibility criteria included those with disease that is primary-resistant to imatinib (Gleevec; progresses within 6 months of first-line imatinib treatment), is SDHB deficient via IHC; an age of 12 years or older, an ECOG performance status of 0 to 2, and adequate hematologic, bone marrow, renal, and liver function.
Exclusion criteria included prior treatment with any anticancer chemotherapy, biological agent, immunotherapy, or radiotherapy within 28 days or 5 times the half-life, before the first dose of olverembatinib; prior use of any TKIs or participation in any clinical trials of other agents within 14 days prior to the first olverembatinib dose; presence of malabsorption syndrome or other diseases affecting oral drug absorption; brain metastasis; and cardiovascular diseases of clinical significance.
Enrolled patients received an oral administration of olverembatinib at doses ranging from 20 mg to 50 mg once every other day in 28-day cycles. The recommended phase 2 dose was defined as 40 mg for adults and adolescents aged 12 to 18 years. Of these patients, 26 were evaluable for the safety population and 26 were evaluable for radiologic response.
The median age of patients enrolled onto the investigation was 30 years (13-56). Most patients were female (73.1%) and had a primary tumor site of the stomach (92.3%), and the median time from initial diagnosis to trial enrollment was 4.7 years (0.2-19.5). Patients either had prior treatment with 0 (3.8%), 1 (30.8%), 2 (15.4%), or at least 3 (50.0%) TKIs; 15.4% of patients previously received’ temozolomide. Notably, patients had germline mutations in SDHB (46.2%), SDHA (3.8%), and/or SDHC (5.8%).
Further results showed a median progression-free survival (PFS) of 27.5 months (95% CI, 12.9–not reached). Qiu noted that, in PFS data collection from real-world studies used for historical control, the median PFS per treatment line is typically 6.0 months (n = 32; 95% CI, 4.0-7.0) in the first-line, 8.0 months (n = 19; 95% CI, 3.0-8.0) in the second, and 5.0 months (n = 11; 95% CI, 1.0-NR) in the third-line setting.
Other reported real-world median PFS data in the presentation included sunitinib (Sutent) at 6.0 months (n = 21; 95% CI, 3.0-7.0) and regorafenib (Stivarga) at 5.5 months (n = 11; 95% CI, 1.0-8.0) months.
Regarding safety, 38.5% of patients experienced grade 3 or higher treatment-emergent adverse events (TEAEs), 7.7% of which were treatment related. Serious AEs were reported in 2.3% of patients, though none were treatment related. No deaths were reported.
The most frequently observed TEAEs included pyrexia (any grade, 73.1%; grades 3-5, 0%), increased aspartate aminotransferase (65.4%; 7.7%), hyperuricemia (61.5%; 0%), increased alanine aminotransferase (57.7%; 7.7%), and anemia (50.0%; 0%). Additional grade 3 to 5 events that were reported included upper abdominal pain in 3.8% of patients and proteinuria in 3.8% of patients.
Steady-state exposure of olverembatinib increased proportionally within the dose range of 30 to 50 mg and no significant accumulation was observed after multiple doses. Furthermore, the maximum plasma concentration of olverembatinib was reached 6 to 8 hours after multiple oral doses, and the terminal elimination half-life was approximately 13 to 18 hours.
In his conclusion, Qui noted that the olverembatinib research has prompted a phase 3 clinical study that will start soon.
Disclosures: Qiu has no relationships to disclose.
References
- Qiu H, Zhou Z, Zhou Y, et al. Updated efficacy results of olverembatinib (HQP1351) in patients with tyrosine kinase inhibitor (TKI)-resistant succinate dehydrogenase (SDH)-deficient gastrointestinal stromal tumors (GIST) and paraganglioma. J Clin Oncol. 2024;42(suppl 16):11502. doi:10.1200/JCO.2024.42.16_suppl.11502
- Ascentage Pharma hosts ceremony marking the launch of olverembatinib in newly approved indication and the dispatch of first batch for the new indication. News release. Ascentage Pharma. November 24, 2023. Accessed January 19, 2024. https://www.biospace.com/article/releases/ascentage-pharma-hosts-ceremony-marking-the-launch-of-olverembatinib-in-newly-approved-indication-and-the-dispatch-of-first-batch-for-the-new-indication/#:~:text=In%20November%202021%2C%20olverembatinib%20was,AP)%20harboring%20the%20T315I%20mutation
- Live from ASCO 2023: updated data of olverembatinib in SDH-deficient GIST including a CBR of 93.8% signals a potential clinical breakthrough. News release. Ascentage Pharma. June 5, 2023. Accessed, June 4, 2024. https://www.ascentage.com/live-from-asco-2023-updated-data-of-olverembatinib-in-sdh-deficient-gist-including-a-cbr-of-93-8-signals-a-potential-clinical-breakthrough/
- Qiu H, Zhou Z, Zhou Y, et al. Antitumor activity of olverembatinib (HQP1351) in patients (pts) with tyrosine kinase inhibitor (TKI)–resistant succinate dehydrogenase (SDH)–deficient gastrointestinal stromal tumor (GIST). J Clin Oncol. 2023;41(suppl 16):11540. doi:10.1200/JCO.2023.41.16_suppl.11540