Asciminib Improves MMR Vs TKIs in Ph+ Chronic Myeloid Leukemia
Treatment with asciminib produces a favorable safety profile among patients with Philadelphia chromosome–positive chronic myeloid leukemia in chronic phase.
"We are very encouraged by these results given that a significant proportion of patients with newly diagnosed CML do not achieve their treatment goals," according to Tim Hughes, MD.
Administering asciminib (Scemblix) led to a meaningful improvement in responses compared with standard Tyrosine kinase inhibitors (TKIs) among patients with newly diagnosed Philadelphia chromosome (Ph)–positive chronic myeloid leukemia in chronic phase (CML-CP), according to a news release on results from the phase 3 ASC4FIRST trial (NCT04971226).
Treatment with asciminib produced statistically significant and clinically meaningful outcomes with respect to both primary end points of major molecular response (MMR) compared with TKIs including imatinib (Gleevec), nilotinib (Tasigna), dasatinib (Sprycel), and bosutinib (Bosulif). Additionally, the experimental agent resulted in fewer adverse effects (AEs) and lower rates of treatment discontinuation compared with standard TKIs while raising no new safety signals.
Investigators plan to have another data readout to assess the key secondary end point of 96-week MMR in addition to other secondary end points. Additionally, other data will be presented at future medical meetings and submitted to regulatory health authorities in 2024.
“We are very encouraged by these results given that a significant proportion of patients with newly diagnosed CML do not achieve their treatment goals,” Tim Hughes, MD, a professor at South Australian Health & Medical Research Institute, said in the news release. “There remains a significant need in first-line therapy of CML for tolerable treatment options, allowing people with CML to balance their treatment alongside their quality of life.”
In the ongoing multi-center, open-label phase 3 ASC4FIRST trial, patients with Ph-positive CML-CP were assigned to receive asciminib orally at 80 mg once a day or investigator-selected TKIs including imatinib at 400 mg once a day, nilotinib 300 mg twice a day, dasatinib at 100 mg once a day, or bosutinib at 400 mg once a day.
The trial’s primary end points are 48-week MMR with asciminib vs investigator-selected TKIs and the experimental agent vs TKIs in a group of patients who received imatinib prior to randomization. Secondary end points include treatment discontinuation following adverse effects, complete hematological response, complete cytogenetic response, duration of MMR, time to treatment failure, event-free survival, progression-free survival, and overall survival.
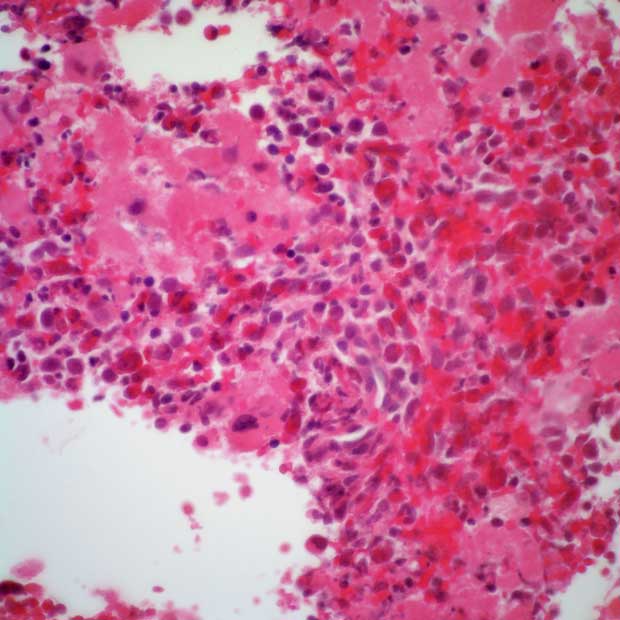
Patients 18 years and older with a diagnosis of CML-CP and cytogenetically confirmed Ph were able to enroll on the trial. Additional eligibility criteria included having less than 15% blasts in peripheral blood and bone marrow, less than 30% blasts and promyelocytes in peripheral blood and bone marrow, less than 20% basophils in peripheral blood, adequate platelet counts, and an ECOG performance status of 0 or 1.
Those with confirmed central nervous system infiltration or impaired cardiac function or cardiac repolarization abnormality were unable to enroll on the trial. Patients were also unsuitable for enrollment if they had a significant congenital or acquired bleeding disorder, major surgery within 4 weeks of study entry, acute pancreatitis within 1 year prior to randomization, or chronic liver disease resulting in severe hepatic impairment.
“Given the chronic nature of their condition, patients often need to be on TKI therapy for many years, so treatment options that are well tolerated and highly efficacious are crucial to support adherence. This study outcome builds on our 20-year legacy in CML innovation as we strive to continue to address the remaining unmet needs for people living with this blood cancer,” Shreeram Aradhye, MD, president of Development and chief medical officer at Novartis, concluded.
Reference
Novartis Scemblix® shows superior major molecular response (MMR) rates vs. standard‐of‐care TKIs in phase III trial for newly diagnosed patients with chronic myeloid leukemia. News release. Novartis. January 8, 2024. Accessed January 8, 2024. https://shorturl.at/nxBR4