ASCO Breast: Mammography in Younger Women, Palpation, Account for Many Diagnoses in Michigan Study
Though there is still disagreement, a new study presented at the ASCO Breast Cancer Symposium in San Francisco suggests that annual mammography and palpation of breast masses remain critical tools in early breast cancer diagnosis.
Controversy has swirled around breast cancer screening since the United States Preventive Services Task Force (USPSTF) changed its guidelines regarding mammography and breast exams in 2009. Though there is still disagreement, a new study presented at the American Society of Clinical Oncology (ASCO) Breast Cancer Symposium in San Francisco suggests that annual mammography and palpation of breast masses remain critical tools in early breast cancer diagnosis.
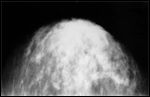
Shown is a mammogram showing subtle cancer
The USPSTF now recommends biennial mammography-rather than annual, as before-for all women beginning only at age 50, with those aged 40 to 49 excluded from such screening. They also say that evidence is insufficient to determine the utility of both mammography in women older than 75 years of age, and of clinical breast exams in women aged 40 and older; the guidelines recommend against teaching women breast self-examination.
“We certainly know that younger women often have denser breast tissue, which can impact or reduce the sensitivity of mammography as compared to in older women, but certainly it doesn’t negate the utility of mammography as a screening test,” said Andrew Seidman, MD, an oncologist at Memorial Sloan-Kettering Cancer Center in New York, during a press event before the symposium.
In the new study that authors stress does not represent a screening population but a group who did present with a diagnosis of breast cancer, the majority of the 5,903-patient cohort was diagnosed prior to the change in screening guidelines. A few, however, were recruited in November and December of 2009. The cohort was a part of the Michigan Breast Oncology Quality Initiative (MiBOQI).
Daniel Smith, a physician’s assistant student at Grand Valley State University who presented the study, said that 3,869 of the patients (65.5%) were diagnosed with mammography, and 1,759 were diagnosed using palpation (29.8%); 90.2% of the latter were through a breast self-examination. A further 275 patients’ cancer was detected with “other” methods, including axillary mass and breast pain, but these were excluded from the primary analyses.
The average age at diagnosis was 59.4 years. “Although the most frequently diagnosed group was between 50 and 69, which was 51% of the sample . . . 26% were diagnosed under the age of 50,” Smith said. Patients diagnosed with mammography were older than those with palpable presentation (61.2 years vs. 55.8 years, P = .001).
Those cancers detected by mammography were also more likely to be early stage, with 25.1% and 52.5% at stages 0 and I, respectively. For palpation, 29.2% and 50% were found at stage I and II, respectively. This may partially explain why palpation patients were more likely to undergo mastectomy than mammography patients (45.8% vs. 27.1%, P = .0001). Palpation patients also received chemotherapy more often than mammography patients (22.7% vs. 15.7%, P = .0001).
Dr. Seidman, who was not involved with this research, noted that the use of screening in younger women has led to lower rates of mastectomy and of chemotherapy because of earlier detection. “This is a very important gain, independent of any potential survival benefits,” he said. “Having less disfiguring surgery and the ability to deliver less chemotherapy based on the stage at diagnosis, for me, is a step forward.”
It is difficult to say exactly how the changes in screening guidelines would have affected this cohort, but Smith did point out that 42.4% of the total sample was diagnosed either through a palpable presentation or mammography conducted in women under the age of 50.
“Women who have breast cancer continue to present with palpable masses even in this contemporary cohort of patients,” said study co-author Jamie Caughran, MD, of Saint Mary’s Lacks Cancer Center in Grand Rapids, Michigan, during the press event. “We conclude that annual screening mammograms and evaluations of palpable breast masses are important tools in breast cancer detection.”