ASCO Breast: No Survival Advantage for Mastectomy vs Breast Conservation Therapy
A new study presented at the American Society of Clinical Oncology Breast Cancer Symposium in San Francisco shows that there is no survival difference between having a mastectomy or breast conservation therapy in women under the age of 40.
The decision whether to undergo mastectomy or breast conservation therapy is a complicated one for breast cancer patients, and perhaps most clearly so for younger women. A new study presented at the American Society of Clinical Oncology (ASCO) Breast Cancer Symposium in San Francisco could remove some concerns, though, showing that there is no survival difference between the two therapy options in women under the age of 40.
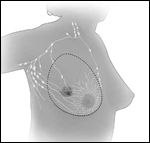
Total (simple) mastectomy
Three decades ago, a series of trials began to show that there was little difference between mastectomy and breast conservation therapy (BCT), but “there has been a reluctance to apply these findings to young women, specifically those less than 40 years old,” said Usama Mahmood, MD, a fellow in radiation oncology at the University of Texas M.D. Anderson Cancer Center in Houston, who led the new study.
That reluctance can be explained by a number of factors, including the fact that those early studies included only small proportions of young women, and that there may be more local recurrences among young women undergoing BCT. “We have seen increases in mastectomy across all ages,” noted Rakesh Patel, MD, director of breast cancer and brachytherapy services at Western Radiation Oncology in Pleasanton, California, during a discussion of the study. “We know it is because of improved [breast] reconstruction options available to women, and use of preoperative MRI has had some influence . . . and all of these factors play a greater role in our younger patients.” Dr. Patel was not involved with the research.
Dr. Mahmood and colleagues analyzed information on 14,764 women in the National Cancer Institute’s Surveillance Epidemiology and End Results (SEER) database. The median age of the study group was 36 years, and patients were followed for a median of 5.7 years; all patients had either stage T1 or T2 breast cancer, and were either N0 or N1 with regard to lymph node involvement.
A total of 6,640 of these patients (45%) underwent BCT, compared with 8,124 who underwent mastectomy. After adjusting for a number of variables, the hazard ratio for overall survival with BCT compared to mastectomy was 0.93, and was not significant (P = .16). Similarly, the HR for cause-specific survival was 0.93, and was also nonsignificant (P = .26).
The group also conducted a matched-pair analysis to confirm these findings. Among 4,644 total patients (2,322 in each group), the 10-year overall survival was 83.5% for BCT and 83.6% for mastectomy (P = .99). The 10-year cause-specific survival was 85.5% in both groups (P = 0.88). Dr. Mahmood noted several limitations to the SEER data, including a lack of information on performance status and genetic predisposition.
“This is the largest data set comparing survival by type of local treatment in young women with early stage breast cancer,” Dr. Mahmood said during a presentation of the study, adding that in spite of these findings there will still be times when mastectomy is the preferred option in younger patients. “Women should be counseled appropriately regarding their treatment options and should not choose a mastectomy based on an assumption of improved survival.”