ASH: Early Results of Daratumumab in Multiple Myeloma Show Promise
Data from an on-going early stage phase I/II trial of daratumumab in multiple myeloma continues to show promising activity. The dose-escalation study has shown that higher doses of daratumumab alone can reduce both bone marrow plasma cells as well as paraprotein.
Data from an ongoing early-stage phase I/II trial of daratumumab in multiple myeloma continues to show promising activity. The dose-escalation study has shown that higher doses of daratumumab alone can reduce both bone marrow plasma cells as well as paraprotein, normally produced at abnormally high levels in multiple myeloma patients. Daratumumab, unlike elotuzumab, another antibody currently being investigated for multiple myeloma, has single-agent activity. According to Torben Plesner, MD, of the department of hematology at Vejle Hospital in Vejle, Denmark, and colleagues, “this has not previously been demonstrated with a single-agent monoclonal antibody in multiple myeloma.” These results were presented at the annual American Society of Hematology (ASH) meeting held in Atlanta.
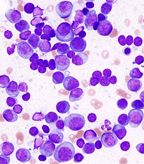
Histopathological image of multiple myeloma; source: KGH, Wikimedia Commons
Daratumumab is a human, monoclonal anti-CD38 antibody that works by mediating the killing of tumor multiple myeloma cells, which tend to overexpress the CD38 cell surface molecule. The antibody is specific for tumor cells as CD38 is not expressed on mature lymphocytes but only myeloid and lymphoid precursor cells.
The most common toxicities reported to date were infusion-related reactions including two grade 3 reactions. Four serious adverse events related to infusion reactions were reported. The trial researchers have since implemented a prednisolone/methylprednisolone steroid regimen prior to all infusions and no serious infusion reactions have been reported since.
The current study, which has accrued 32 patients to date, is the first in-human study of daratumumab in multiple myeloma patients. Two patients have received the highest dose of the antibody, 24 mg/kg. The median age of the patients is 61 and all are heavily pretreated-the median number of prior therapies was 6.3. Patients have received bortezomib, lenalidomide, and thalidomide as prior treatments.
The primary efficacy was based on the best response to paraprotein levels. Patients had reduced levels of paraprotein between 33% and 100% for daratumumab doses of 4mg/kg or greater. Bone marrow plasma cells were reduced by 80% to 100% for patients given daratumumab at all doses of 4 mg/kg or greater. No maximum tolerated dose has yet been found.
Data from the trial on 29 patients presented in June of this year showed that 24% of the patients achieved a partial response, 14% a minimal response, and another 24% had stable disease.
Two phase I/II trials combining daratumumab with either bortezomib and dexamethasone or lenalidomide and dexamethasone for multiple myeloma patients who have received at least two prior therapies are in the works. While Plesner highlights that there are always safety concerns when two therapies are investigated in combination, combination of lenalidomide plus daratumumab appears to be a logical pairing choice. “Daratumumab causes antibody-dependent cellular cytotoxicity-mediated activity and lenalidomide enhances [the activity] of killer T cells.”
“I think there is very good reason to conduct both [combination trials]. Activity and toxicity could differ significantly, and it is not possible to foresee which one will be the best combination,” said Plesner.
Daratumumab is being developed by Genmab along with Janssen Biotech, a wholly owned subsidiary of Johnson & Johnson.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.