ASH: Triple Immunotherapy Shows Activity in Lymphoma Metastasized to the Central Nervous System
Researchers presented a late-breaking abstract reporting activity in a metastatic lymphoma mouse model of two monoclonal antibodies combined with CpG, a short synthetic oligonucleotide agonist of TLR9, that mimic bacterial and viral DNA and facilitates a pro-inflammatory immune response.
In a late-breaking abstract session, Aurlien Marabelle, MD, MSc, reported activity in a metastatic lymphoma mouse model of two monoclonal antibodies combined with CpG, a short synthetic oligonucleotide agonist of TLR9, that mimic bacterial and viral DNA and facilitates a pro-inflammatory immune response (ASH 2011 LBA-2-Local Treg Immunomodulation Cures Metastatic Lymphoma Including CNS Sites).
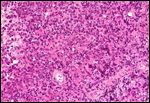
High magnification micrograph of a primary central nervous system (CNS) lymphoma in a human; source: Nephron, Wikimedia Commons
Marabelle is a post-doctoral research fellow in the laboratory of Dr. Ronald Levy in the division of oncology at the Stanford School of Medicine. Dr. Levy helped develop rituximab for the treatment of lymphoma, the first FDA-approved antibody against cancer.
The work from the Levy lab presented by Marabelle showed that together the triple combination breaks the tumor tolerance of the immune system, allowing the immune system to elicit a response and eradicate both local and distant tumors.
By injecting the combination therapy into subcutaneous tumors of immunocompetent mice, Marabelle and colleagues saw eradication of both local and distant tumors, curing mice of established metastatic lymphoma, even with spinal cord metastases. All three components, CpG, anti–CTLA-4, and anti-OX40 antibodies are required for the response.
“This technique could be a paradigm shift in cancer therapy,” said Marabelle during the introduction of his research. An anti–CTLA-4 has been recently approved by the FDA to treat metastatic melanoma patients, and an anti-OX40 is in early stage clinical trials for cancer. The research suggests that this combination can be tested in patients that have injectable sites of lymphoma even with prevalent CNS metastases.
“These results are not limited to lymphoma and in fact we have similar results in solid tumor models not presented today,” stated Dr. Levy in a correspondence with CancerNetwork. “We have also generated exciting data with a breast carcinoma model. This should be part of the story of our upcoming paper on this strategy,” added Marabelle.
Commenting on the feasibility of injecting patient tumors, Dr. Levy pointed out that the results show intratumoral injection of CpG is necessary and that the antibodies “can go either intratumoral or systemic,” but that the advantage of the local injection is lower toxicity. “I think it may be worth going with intratumoral injections if the results are better,” he added.
According to Dr. Levy, a clinical trial in lymphoma with CpG and an anti-PD1 antibody is in the works. “Our results show that the OX40 antibody is required but immediate availability of antibodies against CTLA-4 and another check point target, PD1, for human testing make it worthwhile to try them now.” The rationale, according to Marabelle, is to design human trials with the antibodies that are currently available in order to move forward and learn about the toxicities of these combinations for better patient treatment.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.