Avoiding Errors that Lead to Breast Cancer Litigation
WASHINGTON-When women with breast cancer sue their doctors for malpractice, it is most often because of missed or delayed diagnosis, and the most common reasons are mistakes in the evaluation and workup of breast cancer screening procedures, Vara Samudrala, MD, said at the 100th annual meeting of the American Roentgen Ray Society.
WASHINGTONWhen women with breast cancer sue their doctors for malpractice, it is most often because of missed or delayed diagnosis, and the most common reasons are mistakes in the evaluation and workup of breast cancer screening procedures, Vara Samudrala, MD, said at the 100th annual meeting of the American Roentgen Ray Society.
Other frequently cited problems are clinicians who fail to take seriously what their patients tell them and who fail to notify patients of the need for follow-up testing, said Dr. Samudrala, a fellow in radiology at the Henry Ford Hospital, Detroit. Dr. Samudrala and her colleagues drew their conclusions from their review of 150 cases involving missed or delayed diagnosis of breast cancer.
More and more women are undergoing mammographic screening, with the result that breast cancer litigation is increasing in both the number of cases and the amount of settlement claims, Dr. Samudrala said.
A 1995 Physicians Insurers Association of America study showed an average settlement of $183,000 for breast cancer claims. There is every indication that this number is rising, she said.
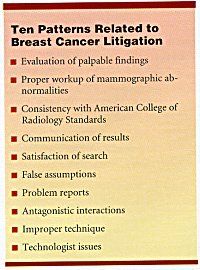
In their survey of claims, the Henry Ford Hospital team found 10 patterns accounting for most of the lawsuits. At the top of the list were clinician mistakes in evaluation of palpable findings, improper workup of mammographic abnormalities, and failure to follow American College of Radiology (ACR) guidelines.
In the majority of such cases, a palpable lesion was present that the patient herself had detected, Dr. Samudrala said. In many cases, the patient was experiencing pain and tenderness in the area in question.
The Michigan team had a number of recommendations to prevent errors leading to litigation.
Mammography alone is not reliable as the only tool to evaluate a massfollow-up with ultrasound may be needed. Do not place a lesion in 6-month follow-up until after proper diagnostic workup, Dr. Samudrala said. Sometimes the lesion looks benign, and a clinician may be tempted simply to use a watch-and-wait approach. However, the Henry Ford teams position is that additional workup is essential for each new mass.
Know the ACR standards for screening and diagnostic mammograms. Follow protocols to avoid mistakes.
Always communicate the results to patients. Dr. Samudrala cited a case in which a woman with a negative screening mammogram was recommended for 6-month follow-up. The patient was not informed of the need for follow-up, and she was diagnosed a year later with breast cancer.
Dont stop searching for abnormalities after the first one has been seen.
Avoid making false assumptions. The team mentioned, in particular, mistaken assumptions about markers such as BBs, used to signal the presence of known lesions. Many times, these are used for benign skin lesions, Dr. Samudrala said, but no one should assume that is what they represent unless it is clearly stated.
Know whats going on in your own institution, she said, warning clinicians to assume nothing, trust no one.
Use standard language (BIRADS) in describing anomalies. Without the standard language, the nature of what the clinician is describing may be unclear, Dr. Samudrala said.
Dont ignore patients complaints. A common theme of the malpractice claims analysis was women with palpable masses who felt they had not been taken seriously. After examination of the mass, the physician may have said its nothing, its a thickening of the breasts, its fibrocystic breasts, Dr. Samudrala said. When we, as radiologists, hear that, bells start ringing.
In a few such cases, she said, the women were in their 20sa factor that may lead a clinician to dismiss an abnormal finding with the assumption that the patient is too young for breast cancer.
The Ford Team also recommends including the patients comments on intake formsbecause they might provide information that will be useful later on.
Use good technique. The researchers gave the example of a patient whose breast increased in size from 1994 to 1996. Ultrasound was performed with poor technique, leading to a mistaken diagnosis of cyst.
Be sure the radiation technologists are property trained. The malpractice claims analysis showed that technologists are not always properly trained and do not always know why the patient is having a mammogram, Dr. Samudrala said.
The Michigan team plans to publish its findings, Dr. Samudrala said, but in the meantime, she hopes that spreading the word will help the breast cancer radiology community do a better job.
Understanding some of the factors that may lead to a malpractice claim can help the radiologist minimize liability exposure, while providing improved care, the team said in a summary of the findings.