Hospital Volume Shown to Predict Breast Cancer Outcome
ASCO-Breast cancer patients receiving care in hospitals that treat fewer than 25 patients a year have substantially lower survival rates than women treated in larger-volume hospitals, according to a study presented at a poster session of the 36th Annual Meeting of the American Society of Clinical Oncology (ASCO), New Orleans.
ASCOBreast cancer patients receiving care in hospitals that treat fewer than 25 patients a year have substantially lower survival rates than women treated in larger-volume hospitals, according to a study presented at a poster session of the 36th Annual Meeting of the American Society of Clinical Oncology (ASCO), New Orleans.
Monica Morrow, MD, reported 5-year survival for breast cancer patients treated with surgery and chemotherapy at 1,238 US hospitals. Although hospital volume has been shown to influence outcome for high-morbidity, complex cancer surgery and chemotherapy, this study population is one that traditionally experiences negligible treatment-related morbidity.
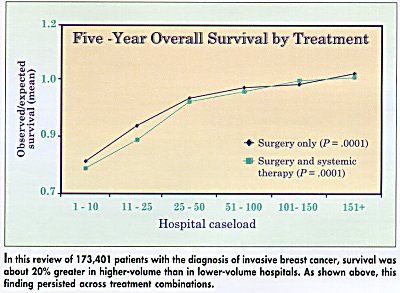
We found that survival in the high-volume hospitals is about 20% greater than in the lower-volume hospitals, said Dr. Morrow, professor of surgery and director of the Lynn Sage Comprehensive Breast Program, Northwestern University Medical School.
This finding persists across all treatment combinations (see Figure), and is not explained by failure of low-volume hospitals to refer patients for systemic therapy. The difference was evident when we looked at patients who were treated with surgery alone or surgery plus systemic therapy, and those who had mastectomy or breast-conserving therapy, Dr. Morrow said.
Data on 173,000 Patients
The investigators analyzed data for 173,401 patients with the diagnosis of invasive breast cancer recorded in the National Cancer Data Base (NCDB) from 1985 to 1991. The NCDB is a joint project of the American College of Surgeons and the American Cancer Society. All the survival data were adjusted for age and stage.
We only studied patients who underwent typical surgical treatment and had a TNM stage, to make sure we were comparing like to like, Dr. Morrow said. Metastatic breast cancer is not included in this study.
The study showed that 35% of hospitals treated fewer than 25 cases per year (8% of total patients). Conversely, only 12% of hospitals treated more than 100 cases per year (35% of total patients). The majority of patients (57%) were treated at hospitals that see 26 to 100 patients annually (53% of hospitals).
No relationship between volume and outcome was seen for patients with ductal carcinoma in situ (DCIS), and differences were observed in patients both over and under age 60, suggesting that these findings are not simply a reflection of differences in comorbidity.
The Message
The message for small hospitals is not dont treat, but learn how to treat better, Dr. Morrow told ONI. She emphasized that the study does not say that doctors in large hospitals are better than doctors in small hospitals. It says that systems of care in large and small hospitals may be different. We must figure out these differences in care and apply what weve learned in larger hospitals to low-volume centers.
Systems of care that may lead to improved outcomes in large-volume hospitals include greater expertise in mammography and pathology, more aggressive use of systemic therapy, and treatment by multidisciplinary teams.
She said that the study serves as a starting point to allow detailed examination of differences in systems of care between small- and large-volume hospitals. Ultimately, she said, we will see if by applying whats been learned in large hospitals to smaller hospitals, we can improve treatment outcomes across the board.