Avutometinib Combo Yields Responses in Serous Ovarian Cancer Subgroups
Findings from the phase 2 RAMP 201 trial highlight responses with avutometinib/defactinib in those with KRAS-mutated low-grade serous ovarian cancer and other patient subgroups.
“Notably, tumor regression was observed in the majority of patients, including those with SD or progressive disease with last line of therapy including previous MEK inhibitors,” according to Susana N. Banerjee, MBBS, MA, PhD, FRCP, and her coauthors.
Heavily pretreated patients with low-grade serous ovarian cancer (LGSOC) experienced responses following treatment with avutometinib (previously VS-6766) plus defactinib, according to subgroup analysis findings from part A of the phase 2 ENGOT-ov60/GOG-3052/RAMP 201 trial (NCT04625270) presented at the Society of Gynecologic Oncology (SGO) 2024 Annual Meeting on Women’s Cancer.1
In the study, 45% (n = 13; 95% CI, 26%-46%) of patients (n = 29) achieved a confirmed overall response rate (ORR). Among patients with KRAS mutations (n = 15), the ORR was 60%, whereas in patients with KRAS wild-type disease (n = 14), the ORR was 29%. Additionally, tumor regression was observed in 86% of patients treated with avutometinib plus defactinib.
Notably, confirmed responses occurred in 3 out of 4 patients who had previously received MEK inhibitors. Among the 13 patients with stable disease (SD), 10 achieved tumor shrinkage, with 6 demonstrating at least a 15% reduction in tumor size. The median time from the last line of treatment was 1.84 months.
The last lines of treatment for the 13 patients who achieved SD included chemotherapy (n = 2), bevacizumab (Avastin) plus chemotherapy (n = 2), hormonal therapy (n = 7), MEK inhibitors (n = 1), and everolimus (Afinitor; n = 1).
“Notably, tumor regression was observed in the majority of patients, including those with SD or progressive disease with last line of therapy including previous MEK inhibitors,” Susana N. Banerjee, MBBS, MA, PhD, FRCP, and colleagues wrote in the presentation. Banerjee is a consultant medical oncologist and research lead of the Gynecology Unit at The Royal Marsden NHS Foundation Trust, as well as a professor in women’s cancers at the Institute of Cancer Research in London.
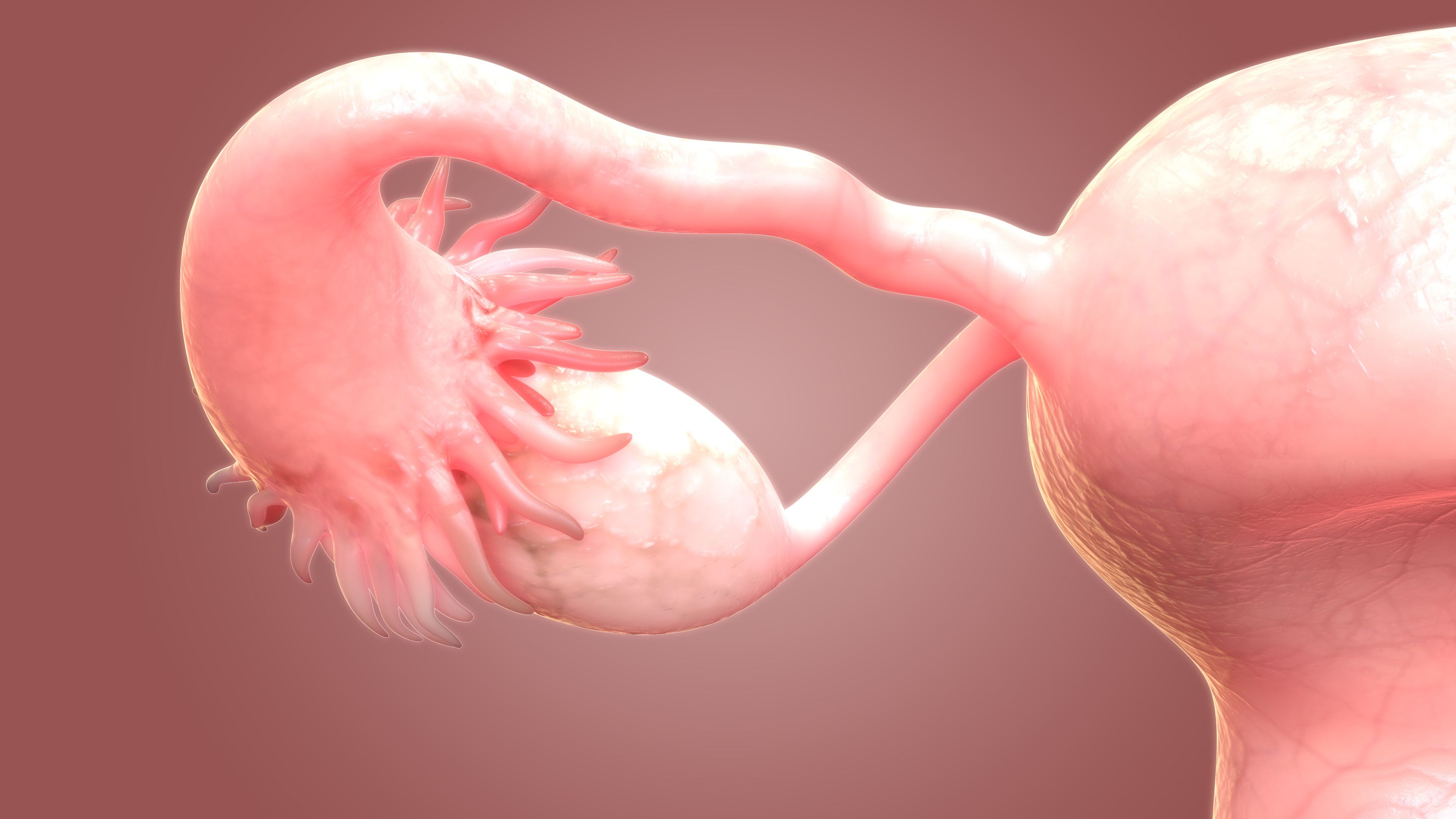
LGSOC is a rare cancer that commonly results from RAS/MAPK pathway alterations and makes up less than 10% of new cases of epithelial ovarian cancer. Notably, existing treatments for this disease have produced objective response rates (ORRs) ranging from 0% to 26%. These unmet needs in LGSOC inspired further research using avutometinib, a novel oral inhibitor of RAF/MEK. This agent targets MEK kinase activity while preventing the compensatory reactivation of MEK by upstream RAF. Similarly, defactinib is an inhibitor of FAK, which is a signaling pathway known to foster resistance to multiple anticancer medications.
The combination of avutometinib and defactinib was previously evaluated in the phase 1 FRAME study (NCT03875820, which supported the regimen’s FDA breakthrough therapy designation in 2021. This paved the way for the RAMP 201 study.2
The current analysis comprised data from patients in the combination arm of RAMP 201, with a data cutoff date of April 6, 2023. In this planned subgroup analysis, patient outcomes were specifically evaluated in the context of lines of prior systemic therapy and best response to the most recent prior treatment in the metastatic/recurrent setting. Notably, results with the combination in patients who experienced SD and those who had previously been treated with a MEK inhibitor were further characterized.
Patients with recurrent LGSOC who received prior treatment of platinum therapy, have measurable disease per RECIST v1.1 criteria, documented KRAS mutation status, and prior MEK inhibitor or bevacizumab treatment were eligible for enrollment onto the study.
The study was split into 4 parts: the selection phase (part A); the expansion phase (part B); the combination expansion phase (part C); and the lower-dose combination expansion (part D). All parts of the study enrolled patients with KRAS-mutant and wild-type disease; parts C and D expanded study enrollment to at least 40 patients and at least 20 to 30 patients, respectively.
Patients treated with avutometinib monotherapy received an oral 4.0 mg twice-weekly dose for 3 out of 4 weeks. Those in the combination group were treated with a biweekly 3.2 mg dose of oral avutometinib plus a twice-daily 200 mg dose of oral defactinib for 3 out of 4 weeks. In part D, the dose of avutometinib was reduced to 1.6 mg biweekly.
The primary end point of the study of the study was ORR by blinded independent review per RECIST v1.1 criteria. Secondary end points included overall survival, PFS, ORR, DOR, disease control rate (DCR), and safety.3
Among the 23 patients in RAMP 201 who experienced poor responses on their last line of therapy in the recurrent or metastatic setting, 43.5% of patients achieved either a complete response (CR) or partial response (PR) with the combination.1 The last line of therapy for these patients included chemotherapy (n = 2), bevacizumab alone or combined with chemotherapy (n = 2), hormonal therapy (n = 4), MEK inhibitors (n = 1), and pembrolizumab (n = 1). The median time since last treatment was 2.7 months. Moreover, 2 of these 23 patients experienced a CR or PR with their most recent prior treatment in the recurrent or metastatic setting. Of the patients with prior MEK inhibitor exposure in part A of RAMP 201, 1 achieved SD and 3 achieved a PR as their best confirmed response with the combination.
Response rates in patients who had previously been treated with 1, 2, or 3 prior lines of therapy were comparable with those in patients who had received 4 or more prior lines. Of the 11 patients treated with 3 or fewer prior lines of therapy, 45.5% of patients achieved a confirmed ORR (95% CI, 17%-77%). Among the 18 patients treated with 4 or more prior lines of therapy, the confirmed ORR was 44.4% (95% CI, 22%-69%).
No patients in either group experienced a CR; PRs occurred in 45.5% and 44.4% of patients with 1 to 3 prior lines vs 4 or more prior lines, respectively. In patients treated with 3 or fewer prior lines of therapy, the rates of SD, PD, and DCR were 45.5%, 9.1%, and 90.9%. These rates were 44.4%, 11.1%, and 88.9%, respectively, in those who received 4 or more lines.
The incidence of grade 3 or greater treatment-emergent adverse effects (TEAEs) in patients treated with the combination approach was consistent between patients with 1 to 3 prior lines of therapy vs at least 4 prior lines of therapy.
Common TEAEs included nausea; diarrhea; blood creatine phosphokinase increase; edema peripheral; vomiting; vision blur; dermatitis acneiform; fatigue; rash; aspartate aminotransferase increase; dry skin; and blood bilirubin increase.
Based on these data the international, confirmatory, phase 3 GOG-3097/ENGOT-ov81/NCRI/RAMP 301 trial (NCT06072781) has been initiated and is enrolling patients to further investigate avutometinib and defactinib vs standard-of-care chemotherapy or hormonal therapy in recurrent LGSOC. The key primary end point of the study is PFS per RECIST v1.1 criteria. Secondary end points included overall survival, PFS, ORR, DOR, disease control rate (DCR), safety, pharmacokinetics, and patient-reported outcomes. In the primary analysis, a hierarchical evaluation will be performed in KRAS mutated LGSOC and all recurrent LGSOC cases.
Disclosures: Banerjee reported honoraria from AstraZeneca, GlaxoSmithKline, Immunogen, Merck Sharpe Dohme, Mersana, Pfizer, Roche, Takeda, Novacure, and Verastem Oncology; being on the advisory board for AstraZeneca, Epsilogen, GlaxoSmithKline, Immunogen, Merck Sharpe Dohme, Mersana, Myriad, Novartis, Oncxerna, Seagen, Shattuck Labs, Regeneron, Verastem Oncology; travel support from AstraZeneca, GlaxoSmithKline, and Verastem Oncology; and stock ownership in Percihealth.
References
- Banerjee SN, Nieuwenhuysen EV, Santin AD, et al. Avutometinib + defactinib in recurrent low-grade serous ovarian cancer (LGSOC): a subgroup analysis of ENGOT-ov60/GOG-3052/RAMP 201 part A. Presented at: 2024 SGO Annual Meeting on Women’s Cancer; March 16-18, 2024; San Diego, CA.
- Verastem Oncology receives breakthrough therapy designation for VS-6766 with defactinib in recurrent low-grade serous ovarian cancer. News release. Verastem, Inc. May 24, 2021. Accessed March 21, 2024. https://investor.verastem.com/news-releases/news-release-details/verastem-oncology-receives-breakthrough-therapy-designation-vs
- A study of avutometinib (VS-6766) v. avutometinib (VS-6766) + defactinib in recurrent low-grade serous ovarian cancer with and without a KRAS mutation (RAMP 201). ClinicalTrials.gov. Updated March 12, 2024. Accessed March 21, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04625270