Bezuclastinib Demonstrates Improved Symptoms in Systemic Mastocytosis
Median duration on bezuclastinib was 56 weeks vs 40 weeks for placebo in non-advanced systemic mastocytosis, the phase 2 Summit trial reported.
Median duration on bezuclastinib was 56 weeks vs 40 weeks for placebo in non-advanced systemic mastocytosis, the phase 2 Summit trial reported.
Data presented at the 2024 American Society of Hematology Annual Meeting & Exposition (ASH) from the phase 2 Summit trial (NCT05186753) showed that, in patients with non-advanced systemic mastocytosis, a 100 mg dose of bezuclastinib was judged to be safe and demonstrated significant improvement with regard to symptoms and biomarkers for mast cell burden.
The researchers noted that this abstract reported on patients treated with both bezuclastinib formulations in parts 1a or 1b of the trial, which had similar pharmacokinetic exposures. In particular, this presentation focuses on the 24-week outcomes of patients receiving the selected 100-mg dose of bezuclastinib and participating in the open-label extension.
At the 12-week assessment, the median duration on bezuclastinib was 56 weeks (range, 9.3-80.9) for the 18 patients on active treatment. For placebo, the median duration was 40 weeks (range, 30.3-72.1) in 9 patients.
At 12 weeks, with a data cutoff on Dec. 18, 2023, the safety and tolerability profile of bezuclastinib was encouraging, with most treatment-emergent adverse events (TEAEs) considered low grade and reversible without dose modification.
The most common TEAEs reported in patients treated with 100 mg of bezuclastinib included nausea, hair color changes, peripheral edema, diarrhea, taste disorder, GERD, and neutropenia. There were no reports of bleeding or cognitive impairment events.
Of the patients who experienced LFT elevations, 5 resolved without dose modification and remain on the study; 2 patients resolved with dose reduction and remain on study at 72 weeks; and 2 patients with grade 3 events resolved following discontinuation.
Bezuclastinib at 100 mg led to rapid, deep, and sustained reductions in serum tryptase over 24 weeks of treatment. In particular, 89% of patients had at least a 50% decrease in serum tryptase levels by 4 weeks of treatment with 100 mg of bezuclastinib once a day. Of the patients with baseline serum tryptase of at least 20 ng/mL, 95% (20/21) who were treated with 100 mg of bezuclastinib achieved levels less than 20 ng/mL. For patients whose baseline serum tryptase was less than 11.4 ng/mL, 84% (21/25) achieved levels less than 11/4 ng/mL with 100 mg of bezuclastinib.
Patients treated with 100 mg of bezuclastinib reported sustained improvements in symptom severity. Of patients receiving 100 mg active treatment with bezuclastinib for 24 weeks, MS2D2 Total Symptom Score reduced by a mean of 27.6 points. In addition, MS2D2 Total Symptom Score reduced from baseline by a median of 55.8%. Nearly a third of patients (31%) reduced or discontinued their best supportive care medications by 24 weeks.
Of the patients receiving 100 mg active treatment with bezuclastinib for 24 weeks, 88% reached at least a 30% reduction in MS2D2 Total Symptom Score, and 76% of patients reached at least a 50% reduction in MS2D2 Total Symptom Score.
Researchers noted that the patients treated with 100 mg of bezuclastinib demonstrated clinically meaningful changes in symptoms, an effect that deepened with 24 weeks of treatment.
During 24 weeks of treatment with 100 mg of bezuclastinib, health-related quality-of-life improvements deepened in MC-QoL Total Score and across all domains. For example, patients had significant improvements in quality of life with a reduction from “moderate” to “mild” disease. During this 24-week period, MC-QoL Total Score reduced by an average of 25.4 weeks. MC-QoL Total Score reduced from baseline by an average of 48.9%.
Background and Study Design
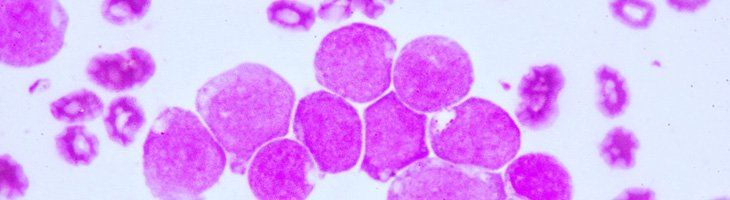
The Summit study is a phase 2, double-blind, placebo-controlled, randomized-controlled study evaluating bezuclastinib in non-advanced systemic mastocytosis. In Part 1 of the study, the primary objective was to determine the recommended dose of bezuclastinib. To do so, researchers enrolled patients with indolent systemic mastocytosis or smoldering systemic mastocytosis based on the 2016 WHO classification, and moderate to severe symptoms on 2 or more anti-mediator therapies.
After screening and enrollment, patients were randomized 1:1:1 to either part 1a (the original formulation; n = 20) or part 1b (the optimized formulation; n = 34). Part 1a consisted of 100 mg of bezuclastinib once a day plus best supportive care; 200 mg of bezuclastinib once a day plus best supportive care; or placebo plus best supportive care. For part 1b, the doses of bezuclastinib were 100 mg and 150 mg once a day. In the open-label extension, the primary objective was to characterize long-term safety and tolerability of bezuclastinib.
Of the patients in part 1 of the Summit study, 19 patients received placebo and 18 received 100 mg of bezuclastinib for 12 weeks.
Regarding patient demographics, 66.7% were female, and the median age was 52 years (range, 36-76). At screening, most patients had an ECOG performance score of 1 (51.9%), followed by 0 (44.4%) and 2 (3.7).
At baseline, patients noted that their most severe symptoms were within the fatigue and skin domains. In addition, at baseline, patients were managing their symptoms of non-advanced mastocytosis with 2 (44.4%), 3 (29.6%), or 4 or more (25.9%) best supportive care medications. Of the 27 patients in the study, 1 received prior avapritinib (Ayvakit).
Regarding baseline mast cell burden, 77.7% of patients were positive for KIT D816V in whole blood. Patients had a median bone marrow mast cell burden of 10% (range, 1-30), and a median serum tryptase at baseline of 37 ng/mL (range, 9.8-275). Six percent of patients had a level less than 20 ng/mL, whereas 21% of patients had levels of 20 ng/mL or greater.
The mean quality of life measures at baseline were 48.3 for MS2D2 (SD, 19.3), 52.7 for MCQoL (SD, 16.1), and 42.3 for MAS (SD, 14.3).
Reference
Rein LAM, DeAngelo DJ, Modena BD, et al. Updated efficacy and safety results of patients receiving selected 100mg bezuclastinib dose and participating in the open-label extension of summit: A randomized, double-blind, placebo controlled phase 2 clinical trial of bezuclastinib in adult patients with nonadvanced systemic mastocytosis. Presented at: 2024 ASH Annual Meeting; December 7-10, 2024; San Diego, California. Abstract 4556.