Bortezomib Plus Vorinostat for Multiple Myeloma Results in Small PFS Advantage
Adding vorinostat to bortezomib for the treatment of relapsed multiple myeloma resulted in a statistically significant increase in progression-free survival compared with bortezomib alone, according to results of a new study.
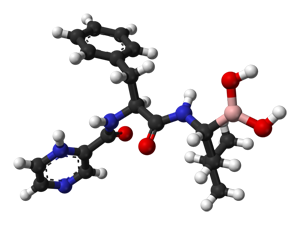
Chemical structure of bortezomib
Adding the histone deacetylase (HDAC) inhibitor vorinostat to bortezomib for the treatment of relapsed multiple myeloma resulted in a statistically significant increase in progression-free survival compared with bortezomib alone, according to the results of a study published recently in the Lancet Oncology.
However, given that the survival difference was only 0.8 months, the responses seen may not be durable and “the clinical relevance of the difference in progression-free survival between the two groups is not clear,” concluded Meletios Dimopoulos, MD, of the University of Athens, Greece, and colleagues.
The phase-III double-blind study included patients with non-refractory multiple myeloma who were randomly assigned to treatment with bortezomib plus vorinostat (n = 317) or bortezomib plus placebo (n = 320). All patients had responded to a prior treatment and patients with resistance to bortezomib were excluded. The median age of patients was 62 years.
Patients assigned vorinostat had a median progression-free survival of 7.63 months compared with a median survival of 6.83 months in those assigned placebo (P = .01).
“We noted significant differences in progression-free survival in favor of the vorinostat group for patients without previous proteasome inhibitor treatment, patients with previous immunomodulatory drug treatment, patients with non-refractory disease, patients younger than 65 years, women, patients with ISS score 1 staging, and those with one previous treatment regimen,” the researchers wrote.
Half of the patients assigned to vorinostat had a dose reduction at least once; whereas, only 25% of patients on placebo required the same. The majority of patients experienced an adverse event. Ninety-eight percent of adverse events in the vorinostat group and 88% in the placebo group were considered to be related to treatment.
“Limitations of our study include the lack of generalizability to myeloma patients in the general population,” the researchers wrote. “Although the median age of our patients was consistent with the age of patients with myeloma who participate in large randomized trials, elderly patients with myeloma are under-represented in most such trials. This discrepancy results in restricted knowledge about the applicability of the trial results in the elderly population.”
In an editorial that accompanied the research, Guy Pratt, MD, of the University of Birmingham, United Kingdom, questioned the use of bortezomib alone as a control arm when the drug is usually assigned in combination with dexamethasone, but pointed out that when the trial began the combination was “less well established.”
“Dimopoulos and colleagues’ study is important in that it affirms the synergy of the combination of vorinostat and bortezomib in the first phase III trial of HDAC inhibitors in multiple myeloma and supports further exploration of HDAC inhibition,” Pratt said. “Future developments in the specialty include continued exploration of HDAC inhibitors, especially for a more targeted approach using selective HDAC inhibitors, finding optimal partners for HDAC inhibitors in combination therapies, and optimizing dose and scheduling.”
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.