Building Upon an “Era of Therapeutic Refinement” in Pancreatic Cancer
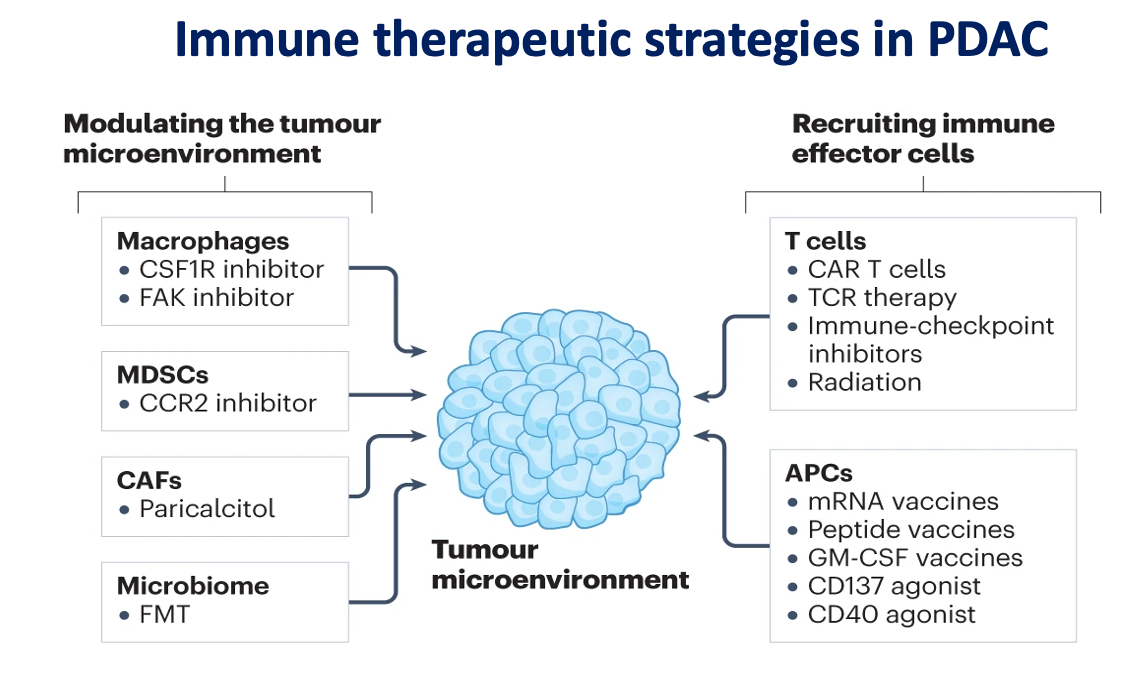
Immunotherapy options like CAR T-cell therapy and antigen-presenting cell-directed agents are currently being evaluated in the pancreatic cancer field.
The pancreatic cancer treatment field has a “very exciting future,” according to Mehmet Sitki Copur, MD, FACP.
Copur, a medical director of Oncology and adjunct professor of Medical Oncology/Hematology at the University of Nebraska Medical Center, a medical oncologist/hematologist at Morrison Cancer Center of Mary Lanning Healthcare, and gastrointestinal editorial advisory board member for the journal ONCOLOGY, spoke with CancerNetwork® during Pancreatic Cancer Awareness Month about potential future directions for pancreatic cancer treatment and research.
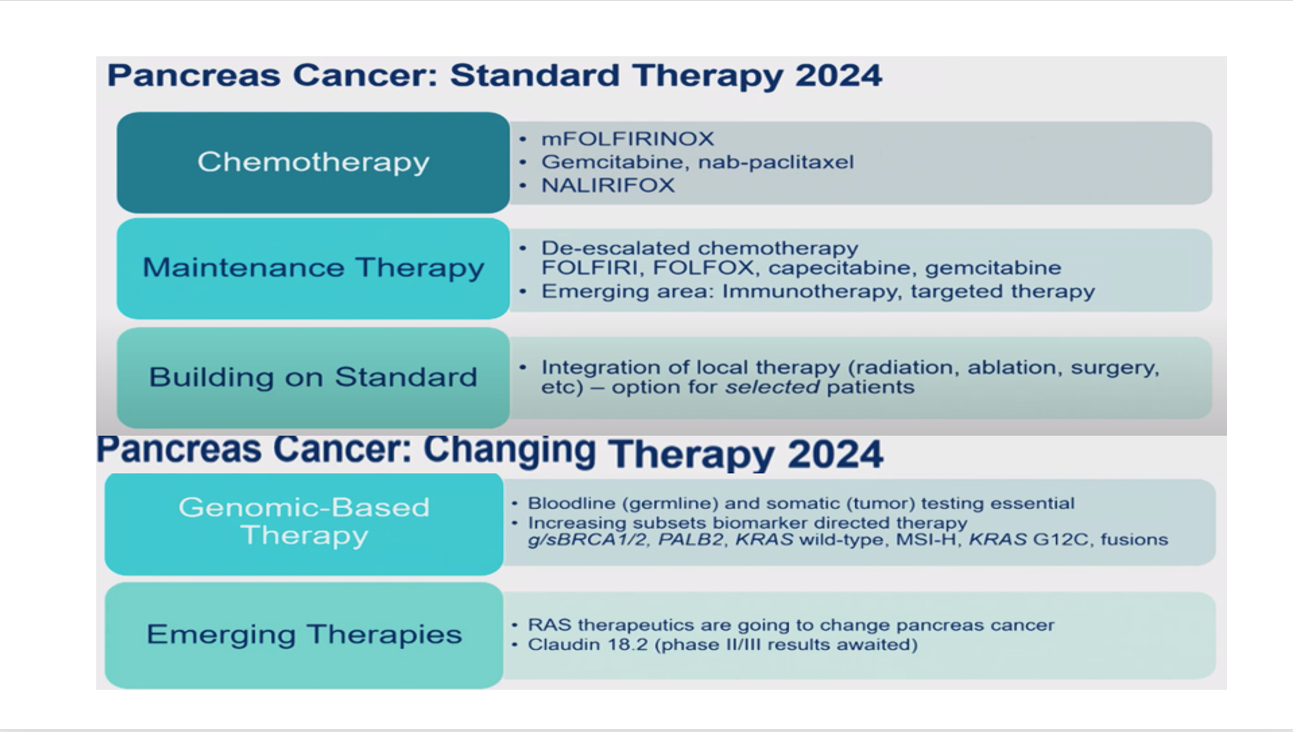
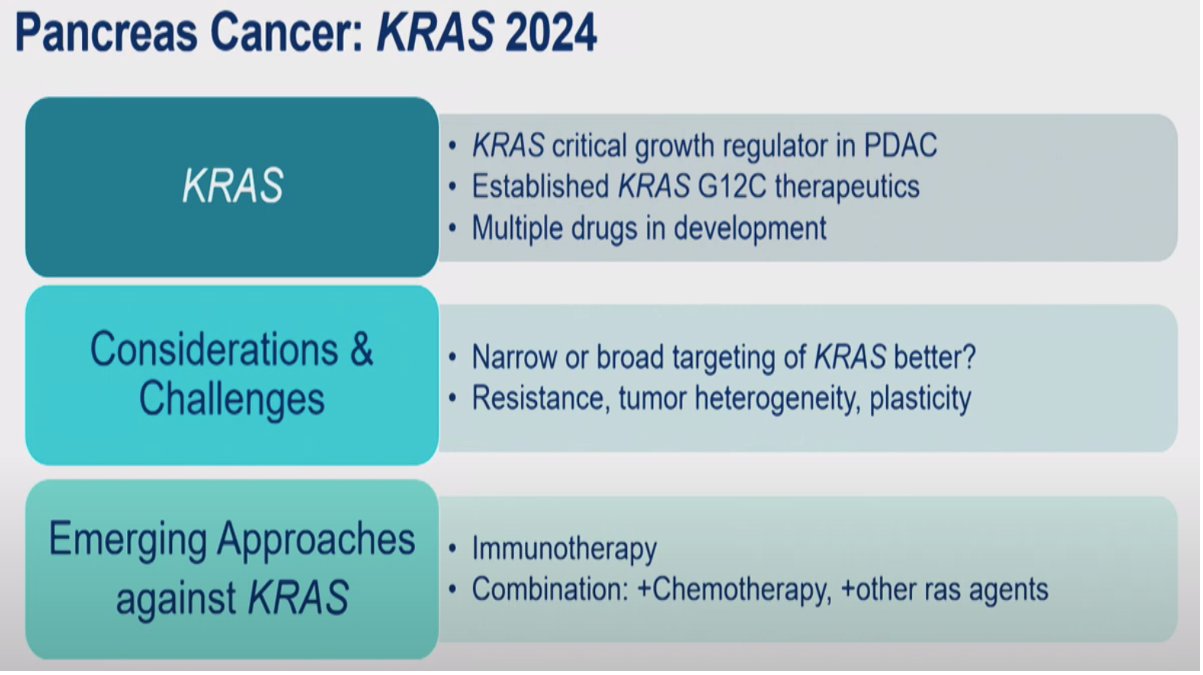
Currently, those in the pancreatic cancer field are navigating an “era of therapeutic refinement and increasing therapeutic complexity” as further research continues to be dedicated to refining potential prognostic biomarkers. As survival rates among patients gradually improve, Copur highlighted the adoption of biomarker-driven selection of cytotoxic chemotherapy, targeted therapies, and immunotherapies to potentially further optimize outcomes. Other novel treatment modalities in the field include cellular therapies, vaccines, and microbiota-directed agents.
Transcript:
As far as the future directions of pancreatic cancer research, as of 2024, we are in the era of therapeutic refinement and increasing therapeutic complexity with biomarker selection for subgroups of patients. There is an ongoing need to improve predictive and prognostic biomarkers.
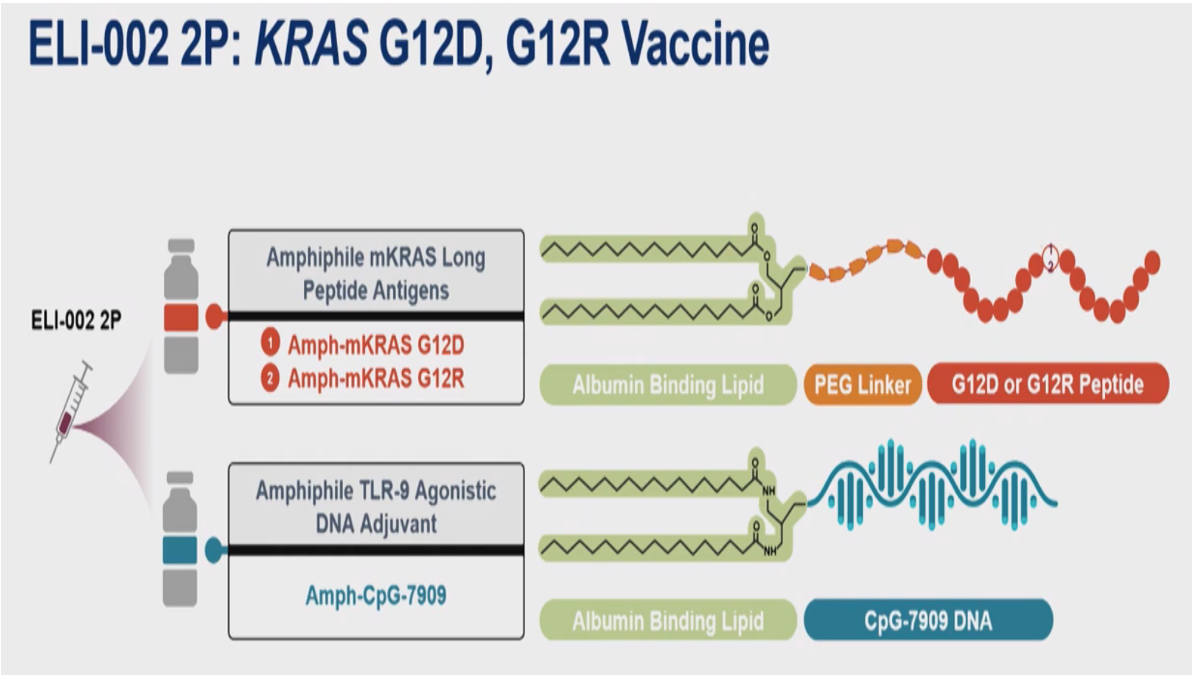
As clinical trials and technology mature over the next decade, outcomes will certainly improve. Already within the past 10 years, we have improved to [a 5-year survival rate of] 12%. [We are also adopting] biomarker-driven selection of cytotoxic chemotherapy and targeted therapies. In immunotherapies, there is a lot going on there, and I have identified some nicely selected targeted therapies. Under immunotherapy, there are antigen-presenting cell-directed [agents]. There are cellular therapies that are T-cell receptor–directed. There are CAR T-cell therapies. Then, there are these vaccines. Interestingly, there are fecal microbiota–directed therapies. Then there is a drug delivery system related to clinical trials.
It’s a very exciting future, and I hope that this will make further progress in our fight against this deadly disease.
Standard and Changing Pancreatic Cancer Therapy in 2024
KRAS mutations in Pancreatic Cancer
KRAS-directed vaccine design in pancreatic cancer
Immune therapeutic strategies in PDAC
All images are posted with the permission of Mehmet Sitki Copur, MD, FACP.