Care of the Pregnant Patient With Cancer
A diagnosis of cancer and its subsequent treatment can be a very frightening and confusing experience for the pregnant patient, and are challenging for the physician and nurse. As women delay childbirth until later in life, the incidence of pregnancy associated with cancer is expected to increase. Currently, approximately 1 in 1,000 pregnancies is complicated by cancer.[1–5]
An estimated 1 in 1,000 pregnancies is complicated by cancer, and the incidence of cancer during pregnancy is expected to increase as women delay childbirth until their later years. A diagnosis of cancer and the cancer treatment process can be particularly difficult for the pregnant patient, and are challenging for the physician and nurse. This article provides an overview of cancer treatment during pregnancy, discusses current practice guidelines and the oncology nursing role in caring for this unique patient population, and highlights resources for clinicians and patients.
A diagnosis of cancer and its subsequent treatment can be a very frightening and confusing experience for the pregnant patient, and are challenging for the physician and nurse. As women delay childbirth until later in life, the incidence of pregnancy associated with cancer is expected to increase. Currently, approximately 1 in 1,000 pregnancies is complicated by cancer.[1–5]
The tumors most commonly seen in women of childbearing age include cervical cancer, breast cancer, melanoma, lymphoma, and acute leukemia.[2–5] Today, many patients with these diagnoses choose to continue their pregnancies. Some patients may delay beginning treatment until after delivery, while others start treatment immediately. This decision depends on their diagnoses, stage of disease, and gestational age. Patients diagnosed late in their pregnancy may choose to deliver their babies early and then begin treatment immediately following delivery.
Patients treated while pregnant pose special challenges. When a cancer patient is pregnant, treatment decisions must take into account the welfare of the patient and the unborn baby. There is an obligation to do “good” for both mother and fetus.[1,6] This article provides an overview of cancer treatment during pregnancy and discusses current practice guidelines developed at our comprehensive cancer center, including the oncology nurse’s role in the care of these patients.
At our cancer center, to ensure continuity of care, a nurse from the Department of Gynecologic Oncology functions as a “nurse liaison” to assist our pregnant patients and their physicians. We have followed 89 pregnancies to date (4 women had 2 pregnancies since their cancer diagnosis). Figure 1 shows the distribution of disease types in a pregnant population at our cancer center between 2003 and April 2008. Figure 2 shows the outcome of pregnancies of patients who were
enrolled and followed in our data-collection study.
Anatomical and Physiological Changes During Pregnancy
Caring for a pregnant patient with cancer must take into account both anatomical and physiological changes occurring during pregnancy and risks associated with cancer diagnosis and treatment.
Maternal blood volume increases by about 40%–50% during pregnancy. Other hemodynamic changes include increases in cardiac output, systemic blood pressure, pulmonary vascular resistance, heart rate, and blood flow distribution. Coagulation properties change during pregnancy, resulting in an increased risk of pulmonary embolus and deep venous thrombosis.[7–9]
As the gravid uterus grows, anatomical changes occur. The diaphragm and abdominal organs are pushed upward. The heart changes in position, appearance, and function, and the heart rate increases and peaks in the third trimester. Respiratory and gastric functions may be altered.[7,8,10] Positioning the patient on her left side during the late stages of pregnancy ensures good circulation. When the mother is supine for long periods of time, the gravid uterus can compress the inferior vena cava and compromise circulation.[7–9]
Pregnancy Assessment in the Newly Diagnosed Patient
It is important to ask any female patient of childbearing age the date of her last menstrual period, before administering chemotherapy or performing any test with radiation. This provides an opportune moment to teach the patient the importance of contraception during cancer treatment. If pregnancy is suspected, but not certain, a serum pregnancy test should be done. In a normal pregnancy, the level of beta HCG (human chorionic gonadotropin) increases by 66% every 48 hours beginning at the time of implantation of the fertilized ovum. The first trimester is a period of organogenesis. Fetal exposure to chemotherapy agents in the first trimester may cause spontaneous abortion or congenital malformation.[2]
It is important to ask the patient about her desires for the pregnancy. If she is not certain and/or needs counseling, she may be referred to a gynecologist for consultation. The physician can review the impact of cancer treatment relative to gestational age and address questions or concerns. Some patients are quite clear as to what they want to do. For others, the decision is more difficult and more information is needed.
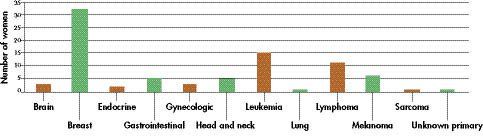
Figure 1: Cancer During Pregnancy-Distribution of disease types in the pregnant population at M.D. Anderson Cancer Center between 2003 and 2007. Data represent 89 pregnancies in 85 women.
As with any cancer patient, early diagnosis and treatment offer the best prognosis. Regardless of cancer stage at diagnosis, pregnant patients with cancer do not appear to have a more aggressive clinical course, and the biological behavior of the cancer appears not to be influenced by the pregnancy.[3] Outcomes are similar in pregnant vs nonpregnant women with cancer.[2]
Diagnositic Testing
In some cases, a cancer diagnosis is delayed because the woman may attribute her symptoms to physiological changes that occur during pregnancy. In addition, the suspicion of cancer during pregnancy is low and there are perceived difficulties and dangers in investigating symptoms.[2] Patients with breast cancer are more likely to present with an advanced stage of disease; this is because small lumps are less easily detected due to the natural changes
occurring in the breast during pregnancy.[5]
Mammography has a high false-negative rate during pregnancy. Loibl et al state, however, that “mammography is the most intensively studied imaging procedure during pregnancy and the only one to rule out extensive microcalcifications and should therefore be used if it is necessary. With adequate abdominal shielding, mammography presents little risk to the fetus.”[11]
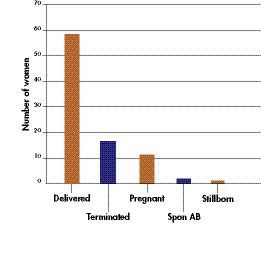
Figure 2: Outcomes of Pregnancies-A total of 85 pregnant patients with cancer were followed in M.D. Anderson data collection study. (Four women have had two pregnancies since their cancer diagnosis.) Of these 89 pregnancies, 58 patients (65%) have given birth, 17 (19%) terminated their pregnancy, 11 (12%) are currently pregnant, 2 (3%) had a spontaneous abortion, and 1 (1%) had a stillborn birth.
When cancer is suspected, biopsy or needle aspiration should be performed for diagnosis and should not be postponed until after delivery. While pregnancy-associated breast cancer typically occurs at a later stage and is often estrogen receptor–negative, breast cancers diagnosed during pregnancy have a prognosis similar to breast cancer in the nonpregnant patient when matched for stage and age.[12]
Many diagnostic tests can be done during the first trimester. Moran et al state that “diagnostic and staging investigations during pregnancy should be limited to essential tests with the lowest exposure to ionizing radiation possible.” If possible, abdominal and pelvic CT (computed tomography) scans and barium enemas should be avoided.[2] Routine CT scans and bone scans are not recommended during pregnancy because of the amount of radiation exposure to the fetus.[12] Ultrasound testing can be performed safely during pregnancy, and can differentiate between cystic and solid lesions. Chest x-rays are also safe, provided that the abdomen is shielded.[7]
Magnetic resonance imaging (MRI) is increasingly used, although there are some concerns regarding the safety of both enhanced and nonenhanced MRI scans during the first trimester.[2] MRI with contrast is not recommended because of concerns about the safe use of gadolinium and the difficulty in positioning a gravid patient in a prone position.[7,11] If necessary, an MRI may be done without contrast to rule out a bone metastasis.
A lead shield should be placed over the abdomen to reduce the amount of radiation to the fetus.[2,7,13] Radiologic diagnostic tests that deliver less than 5cGy to the fetus do not increase the risk of growth retardation and spontaneous abortion, and they are not believed to cause birth defects, even during the first trimester.[7,13]
Timing of Treamtment During Gestation
The first trimester of pregnancy, from conception to the end of the 12th week, is the period of organogenesis, when most treatment is contraindicated. The second trimester is from week 13 to the end of week 26, and the third trimester is from the 27th week until delivery. A full-term pregnancy is 40 weeks in duration.
Implantation occurs in the first 2 weeks following conception. If chemotherapy is given at this time, a spontaneous abortion is likely to occur. All major organs and organ systems are formed during the second to eighth week of gestation. The developing embryo is most susceptible to teratogenic effects of antineoplastic agents at this time.[14]
The ideal time for treatment is during the second trimester and early part of the third trimester, during which time the fetus is formed and continues to mature. A fetus is usually considered viable at 24 weeks.[1,2] At this time, survival is possible with neonatal intensive care. Each time the patient is seen, it is important to always document the last menstrual period, the expected date of delivery, and the gestational age, as it is essential to know when the fetus is viable.
It is also important to document the name and contact information of the patient’s obstetrician and/or maternal fetal medicine (MFM) specialist, and the hospital that will be used for delivery, so that the information is readily available in case of an emergency. If a patient is hospitalized between 24–40 weeks’ gestation in a facility with no obstetric or neonatal services, then there must be a plan of action in case the patient shows any signs of premature labor. If the patient is suspected to be in labor, steps should be taken to immediately transport her to a facility equipped with obstetrical care and a neonatal intensive care unit. At our center, we notify the gynecologist on call to assess the patient. If she is in labor, the gynecologist then contacts the nurse manager who coordinates patient transfer.
Figure 3: Management Protocol-Care of pregnant cancer patients at M.D. Anderson Cancer Center. EMR = electronic medical record; MD = medical doctor; MFM = maternal fetal medicine specialist; OB = obstetric; US = ultrasound.
Timing of delivery is crucial for patients receiving chemotherapy during pregnancy, and is based on response to chemotherapy. The last dose should be given before week 34–36, to allow sufficient time for the patient’s blood counts to recover prior to delivery. In spite of this timing, the newborn may also have pantocytopenia at birth, owing to the inability of the immature liver and kidneys to metabolize and eliminate the cytotoxic agents.[14] When early delivery is chosen, the mother receives steroid injections to increase fetal lung functions and limit intracranial bleeds.[15]
For the melanoma patient, it is recommended that the placenta be sent to pathology at the time of delivery, as melanoma can cross the placental barrier.
Breastfeeding is contraindicated if chemotherapy or hormonal therapy are given postpartum, as cytotoxic agents can be excreted in breast milk.[11,15] Post delivery, the nurse can assist the patient in obtaining follow-up appointments with her oncologists to resume therapy.
Radiation and Chemotherapy
Radiation
Radiation therapy is contraindicated during pregnancy because of its potential for fetal injury. Radiation doses used in cancer therapy are typically
40 to 70 Gy, about 104 to 105 times higher than diagnostic radiation levels. Teratogenic effects
(abnormal fetal development) can result from exposure to radiation in the first 12 weeks of pregnancy, when the embryo is undergoing organogenesis.
Carcinogenic effects may result from exposure to radiation in the second and third trimesters of pregnancy, and these effects are manifested in the first decade of life. National Comprehensive Cancer Network (NCCN) guidelines state that radiotherapy is contraindicated at all stages of pregnancy.
Chemotherapy
Chemotherapy for the pregnant cancer patient is undertaken using a multidisciplinary approach. Patients should visit an MFM specialist before chemotherapy is initiated, so that the growth and well-being of the fetus and the status of the mother can be monitored. Chemotherapy is contraindicated during the first trimester. Chemotherapy agents inhibit cell division through various mechanisms that may directly or indirectly alter DNA, RNA, and protein synthesis, or microtubule function, leading to induction of apoptosis and cell death.[7,14,16] Cytotoxic agents predominantly affect rapidly dividing cells.[2]
Adverse fetal effects of receiving chemotherapy during the first trimester are spontaneous abortion, congenital malformations, and premature birth. Leslie et al state that “there is virtually no information about long-term effects such as learning or behavior problems that may result from the chronic prenatal exposure to chemotherapy.”[15] In a 2006 report, researchers concluded that breast cancer can be treated with FAC (5-fluorouracil, doxorubicin, cyclophosphamide) in the adjuvant (n = 32) or neoadjuvant (n = 25) setting during the second and third trimesters of pregnancy without significant short-term complications for the majority of children exposed to chemotherapy in utero, but cautioned that longer follow-up of the children is required to evaluate possible late effects of FAC on cardiac function and fertility. [17]
Nurses and health care workers strive to make pregnant patients as comfortable as possible during their treatment without harming the fetus, bearing in mind that placental transport of drugs from mother to fetus must be considered beginning with the fifth week of gestation. Patients may experience symptoms common to both pregnancy and chemotherapy (eg, nausea, vomiting, anemia, pain, deep venous thrombosis [DVT], and fatigue); they should be encouraged to practice good self-care, with plenty of rest, proper nutrition, prenatal vitamins, and adequate fluid intake.[7,18]
Nausea and vomiting can be treated with ondansetron (Zofran).[7,19] Ondansetron is reasonably safe to use during the second and third trimesters.[7,20] Recombinant human erythropoietin (epoetin alfa; Epogen, Procrit) is indicated for chemotherapy-induced anemia. It is always important to check blood pressure during pregnancy. Pregnant patients are given the low-molecular-weight heparin enaxaparin (Lovenox) for treatment of DVT.
Treatment of infection and cutaneous, pulmonary, cardiac, and renal complications resulting from cancer therapy should be a collaborative effort between the oncologist and the MFM specialist, to adequately treat the patient while reducing the risk to the fetus.
Surgery
The goal is to provide safe surgical treatment and anesthesia to the mother while minimizing the risk of preterm labor or fetal demise.[7,10] The greatest risk of spontaneous abortion is before the 12th week of gestation.[11] When possible, surgery should be postponed until after the first trimester.[8,21] The ideal time for a patient to undergo surgery is during the second trimester.
Premature labor is more likely to occur during the third trimester. This is a very important risk to consider when deciding when to schedule a surgery. If surgery is being performed after the 24th week, the surgeon and hospital must be prepared to deliver a viable fetus. It is recommended that major surgeries, performed on patients with a viable pregnancy, be undertaken at a hospital with obstetrical and neonatal services.
A multidisciplinary approach is important in surgical planning, and should include the oncologist, surgeon, anesthesiologist, MFM specialist, and the patient. Patients are strongly advised to consult with the MFM specialist prior to surgery. General recommendations of the MFM regarding surgery are:
• Assess fetal heart tones both preoperatively and postoperatively. This is done by one of the gynecologists at our cancer center. Monitoring of the fetus during surgery usually is not necessary.
• Aspirin and nonsteroidal analgesics are contraindicated during pregnancy.
• Anesthesia and analgesia can be used as in the nonpregnant state as long as precautions are taken. Pregnant patients are at a greater risk for aspiration with general anesthesia and more apt to have oxygen desaturation.
• Intraoperative mapping using isosulfan blue dye
has not been approved for use in pregnant patients and is contraindicated because anaphylaxis can occur with its use.
It is important to understand the anatomic and physiologic changes during pregnancy. Adequate uteroplacental blood flow, blood pressure, and oxygenation must be maintained. The mother must be positioned correctly during surgery to avoid aortocaval compression, especially in advanced gestation.[7,10,21]
NCCN Guidelines for Breast and Cervical Cancer in Pregnancy
Breast Cancer
In March 2006, the NCCN issued its first breast cancer guidelines for treatment of early, localized breast cancer during pregnancy.[22] The guidelines are classifed by the NCCN as being based on Level 2A evidence (unanimous consensus on best level of care, rather than Level 1A, based on evidence from clincal trials).
The guidelines suggest that, if the patient is in her first trimester of pregnancy, the doctor and patient should discuss possible termination of the pregnancy so that chemotherapy can be initiated. If the patient in her first trimester chooses to continue the pregnancy, she is then scheduled for a mastectomy with axillary lymph node dissection. After surgery, the treatment guidelines suggest beginning adjuvant chemotherapy in the second trimester.
For cancer discovered during the second trimester or early in the third trimester, the NCCN guidelines suggest that the patient undergo either a mastectomy or lumpectomy, with lymph node dissection. She can also begin chemotherapy as well as undergoing surgery.
In all cases of breast cancer treatment during pregnancy, the NCCN guidelines state that radiation therapy and endocrine therapy (eg, with tamoxifen) must be delayed until after delivery. During pregnancy, patients have usually been treated with FAC combinations, however the NCCN guidelines do not indicate dosing of these drugs during pregnancy.
Cervical Cancer
For the pregnant patient with cervical cancer, NCCN guidelines include the following recommendations and comments regarding colposcopy and follow-up care (Level 2A evidence)[23]:
•Endocervical curettage (ECC) is contraindicated.
•Cervical biopsy or colposcopically directed brush cytology is safe. Consultation with, or referral to, a colposcopist with experience in colposcopy during pregnancy is recommended. A limited excisional procedure is recommended only when invasion is suspected.
•Treatment of (any grade) cervical intraepithelial neoplasia (CIN) should be delayed until after delivery. The guidelines state that women treated using LEEP (loop electrosurgical excision procedure) are at increased risk of premature rupture of membranes or preterm delivery in subsequent pregnancies. While the NCCN notes that women have been treated with chemotherapy for cervical cancer during pregnancy, they advise postponing chemotherapy until after the first trimester, to avoid major congenital malformations.
Experience and Current Practice
Nurse Liaison Role
At our cancer center, physicians refer their pregnant patients to the Department of Gynecologic Oncology. The nurse liaison meets with the patient as soon as possible after the referral is made, explains his or her role as an advocate, and discusses the option of seeking a consult visit with an MFM physician.
Basic information is documented in the medical record regarding the pregnancy. The patient is provided with a copy of an education booklet, “Pregnancy and Cancer.” The nurse also discusses our data collection study and offers the patient an opportunity to participate. The goal of this study is to collect data on patients who are or were pregnant and diagnosed with cancer. (See section in this article, “Databases on Pregnant Patients With Cancer,” page 20.)
Our leukemia and lymphoma patients are often hospitalized either for chemotherapy or for possible side effects such as neutropenia or fever. If they are hospitalized after 24 weeks’ gestation, we request that an MFM physician make an inpatient consultation visit. The recommendations are noted in the patient’s electronic medical record, along with the contact information for the MFM specialist.
Collaboration with MFM Specialists
As we became more aware of the growing number of pregnant patients at our cancer center, it was clear that a more unified and cohesive approach was needed for us to care for these patients. Our cancer center is committed to providing optimal care to patients with special needs. Since many pregnant patients may deliver their babies while undergoing cancer treatment, it is important to identify an obstetrician who specializes in high-risk pregnancies and to facilitate exchange of patient information, to ensure a safe pregnancy and delivery.
There are no obstetricians at our center, so a formal collaboration with the division of Maternal Fetal Medicine at a nearby health science center was established to treat our pregnant patients on an as-needed basis (see Figure 3, page 16). The Society for Maternal Fetal Medicine defines an MFM specialist as “an obstetrician/gynecologist who has completed 2 to 3 years of additional training and formal education and clinical experience. MFM specialists have advanced knowledge of the obstetric, medical, genetic, and surgical complications of pregnancy and their effects on both the mother and the fetus.”
For institutions with obstetrical and neonatal services available, it is recommended to have a policy defining specific guidelines for signs and symptoms of labor or other complications of pregnancy, and outlining what to do should a pregnant patient present in labor.
Patient Resources
Patient education is an important aspect of nursing care of these rare patients. Because patients may have symptoms related both to pregnancy and to cancer and its treatment (eg, nausea, fatigue, anemia, gingivitis), it is important to counsel the patient on good self-care. Naturally, patients also will be seeking information and reassurance about treatment of their cancer while pregnant, and may need counseling regarding specific psychosocial concerns.
Internet resources for pregnant patients with cancer seeking information and support include websites of the National Cancer Institute ([NCI] eg, www.cancer.gov/cancertopics/pdq/treatment/breast-cancer-and-pregnancy/patient); the American Cancer Society (www.cancer.org); the American Society of Clinical Oncology website Cancer.Net (formerly People Living With Cancer); Fertile Hope (www.fertilehope.org), which addresses fertility issues arising from cancer treatment before, during, and after pregnancy; and the Pregnant With Cancer Network (PWCN; www.pregnantwithcancer.org), a national nonprofit organization for women diagnosed with cancer during pregnancy. The Motherisk Program (www.motherisk.org) of the Hospital for Sick Children, University of Toronto, Ontario, Canada, also offers counseling and information for pregnant women with cancer.
A patient education booklet, “Pregnancy and Cancer,” was developed to answer frequently asked questions and provide a list of resources.[24] Naturally, many patients may also need emotional support, as the emotional challenges that are prevalent during normal pregnancies are overlaid with concerns and fears about management and outcome of the patient’s cancer.
Patient Counseling
At our cancer center, when the nurse liaison initially meets with the patient, she gathers information about the patient’s desires regarding the pregnancy. This enables the patient to proceed with scheduling appointments to see either the MFM physician or the gynecologist. Some patients may be under the misconception that they must terminate the pregnancy. Our role is to give them information they need to make the best decision.
A multidisciplinary approach is important. The oncologist will discuss the disease, treatment options, and prognosis with the patient and family. The MFM specialist will review the proposed treatment plan with the patient, and its effects on the pregnancy. If the patient is undecided about whether to continue or terminate the pregnancy, she is offered a consultation appointment with our gynecologist. Often, the oncologists and MFMs communicate together about type and timing of treatment during pregnancy, as well as timing of delivery.
Patients sometimes ask if there are others with a similar diagnosis and history who can contact them. A number of our patients who were treated for cancer during pregnancy have offered to talk with newly diagnosed pregnant cancer patients. This provides emotional support. We also have a chaplain service and psychologists on staff, and can schedule appointments for patients with emotional needs.
Pregnancy and cancer can put a financial strain on patients and their families. In an effort to alleviate this burden, the nurse liaison has assisted patients in obtaining Medicaid coverage. In Texas, most patients are eligible for Medicaid, if they are not otherwise covered by an insurance company, during pregnancy.
Databases on Pregnant Patients with CancerRegistry Study
Researchers at our cancer center have developed a data collection study through their Cancer and Pregnancy Registry. The research database is maintained by the nurse liaison. The goal of the study is to document the types of cancer occurring during pregnancy, the types of treatment these patients receive, and the outcome of their pregnancies, as well as the special needs of these patients. Patients who enroll are given an accession number and information is entered into a password-protected database.
Cancer and Childbirth Registry, Philadelphia
The Cancer and Childbirth Registry, Philadelphia, Pennsylvania, was initiated in 1996 by Elyce Cardonick, MD. Dr. Cardonick, an advisory board member of the Pregnant With Cancer Network, is an associate professor, Robert Wood Johnson Medical School, University of Medicine and Dentistry of New Jersey, Camden. She is investigating the interaction of pregnancy and the natural history of certain types of cancer. Information collected is strictly confidential and concerns diagnosis and treatment of cancer in pregnant women. Currently, about 200 women are included in the registry, mostly patients with breast cancer or Hodgkin’s lymphoma. (For more information, visit www.cancerandpregnancy.com.)
The Motherisk Program at the University of Toronto maintains an international registry of pregnant cancer patients. Gideon Koren, MD, directs the program, which also offers an online Cancer in Pregnancy Forum to which health care professionals can submit questions or describe experiences with patients.
The University of Oklahoma maintains a federal Registry of Pregnancies Exposed to Chemotherapeutic Agents; established at the NCI, it moved to the University of Oklahoma in 1998 and is overseen by John J. Mulvihill, MD. Since 1984, data have been collected on chemotherapy-exposed pregnancies described in the literature or submitted by medical professionals. The more than 600 cases are mainly from published reports on women exposed to chemotherapeutic agents while pregnant.
Conclusion
Cancer treatment presents special challenges during pregnancy. Often choices are made based on the gestational age of the pregnancy at the time of cancer diagnosis. Many diagnostic tests can be performed during the first trimester. Most treatment can be offered safely during the second trimester and in the early part of the third trimester. Good documentation and communication between all health care workers involved are essential.
A multidisciplinary approach is crucial to insure good care of the patient and her unborn baby. At our cancer center, we developed a plan of care that incorporates this multidisciplinary approach. A registered nurse serves as the liaison between the pregnant patient and professionals from the various disciplines involved in her care. The identification of one individual to facilitate care and referral for these patients is important in promoting continuity of care for each patient.
The role of the nurse includes patient advocacy, to ensure that the patient receives proper prenatal care, and the communication of critical health care information to all health care providers. The oncology nurse can assist in communication, continuity of care, and advocacy for the patient and her unborn child.
A written policy with specific guidelines, appropriate for each facility, is recommended in caring for this unique population.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Chervenak FA, McCullough LB, Knapp RC, et al: A clinically comprehensive ethical framework for offering and recommending cancer treatment before and during pregnancy. Cancer 100(2):215–222, 2004.
2. Moran BJ, Yano H, Al Zahir N, et al: Conflicting priorities in surgical intervention for cancer in pregnancy. Lancet Oncol 8(6):536–544, 2007.
3. Jacobs IA, Chang CK, Salti GI: Coexistence of pregnancy and cancer. Am Surg 70(11):1025–1029, 2004.
4. Weisz B, Meirow D, Schiff E, et al: Impact and treatment of cancer during pregnancy. Expert Rev Anticancer Ther 4(5)889–902, 2004.
5. Pavlidis NA: Coexistence of pregnancy and malignancy. Oncologist 7(4):279–287, 2002.
6. Theriault R, Hahn K: Management of breast cancer in pregnancy. Curr Oncol Rep 9(1):17–21,2007.
7. Rimes S, Gano J, Hahn K, et al: Caring for pregnant patients with breast cancer. Oncol Nurs Forum 33(6):1065–1069, 2006.
8. Shaver SM, Shaver DC: Perioperative assessment of the obstetric patient undergoing abdominal surgery. J Perianesth Nurs 20(3):160–166, 2005.
9. Torgersen KL, Curran CA: A systematic approach to the physiologic adaptations of pregnancy. Crit Care Nurs Q 29(1):2–19, 2006.
10. Ni Mhuireachtaigh R, O’Gorman DA: Anesthesia in pregnant patients for nonobstetric surgery. J Clin Anesth 18(1):60–66, 2006.
11. Loibl S, von Minckwitz G, Gwyn K, et al: Breast carcinoma during pregnancy. International recommendations from an expert meeting. Cancer 106(2):237–246, 2006.
12. Woo JC, Yu T, Hurd TC: Breast cancer in pregnancy:
A literature review. Arch Surg 138(1):91–98, 2003.
13. Challoner K, Incerpi M: Nontraumatic abdominal surgical emergencies in the pregnant patient. Emerg Med Clin North Am 21(4):971–985, 2003.
14. Williams SF, Schilsky RL: Antineoplastic drugs administered during pregnancy. Semin Oncol 27(6):618–622, 2000.
15. Leslie KK, Koil C, Rayburn WF: Chemotherapeutic drugs in pregnancy. Obstet Gynecol Clin North Am 32(4):627–640, 2005.
16. Gemignani ML, Petrek JA: Pregnancy-associated breast cancer: Diagnosis and treatment. Breast J 6(1):68–73, 2000.
17. Hahn KM, Johnson PH, Gordon N, et al: Treatment of pregnant breast cancer patients and outcomes of
children exposed to chemotherapy in utero. Cancer 107(6):1219–1226, 2006.
18. MacDougall MK, LeGrand SB, Walsh D: Symptom control in the pregnant cancer patient. Semin Oncol 27(6):
704–711, 2000.
19. Berry DL, Theriault RL, Holmes FA, et al: Management of breast cancer during pregnancy using a standardized protocol. J Clin Oncol 17(3):855–861, 1999.
20. Peters BG, Bray JJ, Masidonski P, et al: Issues surrounding adjuvant chemotherapy for breast cancer during pregnancy. Oncol Nurs Forum 28(4):639–642, 2001.
21. Kuczkowski KM: Nonobstetric surgery in the parturient: Anesthetic considerations. J Clin Anesth 18(1):5–7, 2006.
22. National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology. Breast Cancer. V.2.2008. Available at: www.nccn.org/professionals/physician_gls/PDF/breast.pdf
23. National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology. Cervical Cancer. V.1.2008. Available at: www.nccn.org/professionals/physician_gls/PDF/cervical.pdf
24. M.D. Anderson Cancer Center. Pregnancy and Cancer patient education booklet. Available at: www.mdanderson.org. Linked to the breast cancer and cervical cancer pages.