Confocal Laser Endomicroscopy Can Facilitate the Diagnosis of Both Esophageal and Gastric Cancers
Confocal laser endomicroscopy, a new technology that permits high-resolution subsurface microscopic imaging of living tissue during routine endoscopy, can facilitate the diagnosis of esophageal and gastric cancers, according to a recent report. "Endomicroscopy allows you to make an in vivo histology during ongoing endoscopy," Ralf Kiesslich, MD, PhD, said at the 2006 Gastrointestinal Cancers Symposium (General Session I).
SAN FRANCISCO-Confocal laser endomicroscopy, a new technology that permits high-resolution subsurface microscopic imaging of living tissue during routine endoscopy, can facilitate the diagnosis of esophageal and gastric cancers, according to a recent report. "Endomicroscopy allows you to make an in vivo histology during ongoing endoscopy," Ralf Kiesslich, MD, PhD, said at the 2006 Gastrointestinal Cancers Symposium (General Session I).
The device used is a conventional endoscope that has a confocal microscope integrated into its distal tip, and buttons on the endpiece that control the depth of the imaging plane, explained Dr. Kiesslich, head of the Endoscopic Unit at the University of Mainz, Germany. "Handling of the endoscope is very similar to a conventional endoscope," he added.
Conventional video endoscopy is always performed first. "Inspection of the surface architecture is mandatory prior to endomicroscopy because you have to choose an area of interest where you would like to perform endomicroscopy," Dr. Kiesslich explained. Once an area of interest has been selected, the endoscope is placed in contact with the mucosa, a blue laser light is emitted, and optical sections are obtained, moving from the surface to deeper layers. The field of view is 500 μm X 500 μm, the optical sections are about 7 μm thick, and imaging is possible to a depth of up to 250 μm below the mucosal surface.
Two contrast agents are commonly used during endomicroscopy to enhance mucosal surface and subsurface structures, Dr. Kiesslich said. One is acriflavine, which is applied topically for imaging in the stomach and colon, and the other is fluorescein, which is given intravenously for imaging in the esophagus, stomach, and colon. The images obtained are usually displayed in gray-scale, but color can be added to simulate the normal mucosal appearance.
The learning curve for confocal laser endomicroscopy ranges from 1 week for the imaging of normal tissue to 3 months for the imaging of pathologic tissue, he said. The new technology adds only 10 to 20 minutes to the conventional endoscopy procedure. Although it permits immediate diagnosis at the bedside in some cases, a pathologist is still needed for definitive diagnosis, he emphasized.
Esophageal Applications
In the esophagus, one application of confocal laser endomicroscopy is the diagnosis of Barrett esophagus and associated neoplasia, Dr. Kiesslich said. The new technology permits detailed visualization of the specialized columnar Barrett epithelium, including the glands and individual goblet cells. It can also reveal areas within this epithelium where goblet cells are depleted and where neoplastic epithelial cells have crossed the basement membrane and invaded the lamina propria, both indicators of dysplasia. With the added information from endomicroscopy, he noted, "targeted biopsies can be limited to suspected areas."
In a blinded study (Kiesslich et al, Digestive Disease Week, 2005), confocal laser endomicroscopy was found to have a sensitivity of 98%, a specificity of 94%, and an accuracy of 97% for identifying Barrett epithelium, Dr. Kiesslich said. The technology performed similarly well-with sensitivity of 93%, specificity of 98%, and accuracy of 97%-for identifying Barrett-associated neoplasia.
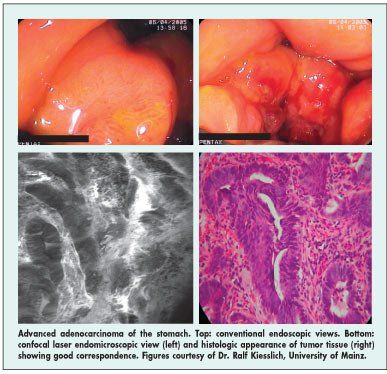
In the stomach, endomicroscopy provides valuable additional information about lesions such as erosive gastritis, intestinal metaplasia, signet ring cell carcinoma, and amyloidosis. It can also facilitate the evaluation of suspected adenocarcinomas seen on conventional endoscopy, with the views obtained in vivo by endomicroscopy showing good correspondence with the ex vivo histology, Dr. Kiesslich said (see Figure).
Gastric Cancer Study
Although data on its performance for identifying gastric cancer are still limited, he noted, a prospective blinded study (Yeoh et al, Digestive Disease Week, 2005) found that confocal laser endomicroscopy had a sensitivity of 84%, a specificity of 95%, and an accuracy of 80% for the identification of gastric cancer. The technology has even been used to make the in vivo diagnosis of Helicobacter pylori infection in the stomach, he said, by enabling visualization not only of accumulations of microbes within gastric glands but also of individual microbes on the mucosal surface, with their distinctive flagella.
Molecular Imaging
Dr. Kiesslich offered some speculation about potential future applications of confocal laser endomicros-copy using molecular imaging. "The goal is risk stratification, via tissue analysis with molecular markers, to identify patients at high risk for the development of cancer and then to optimize therapy," he commented.
In preliminary testing, he said, the new technology has been used to perform in vivo analysis of the liver; to image individual islets within the pancreas using fluorescein-labeled octreotate; to identify aberrant crypt foci in the colon using fluorescein-tagged anti-CD44 antibodies; and in ulcerative colitis, to identify epidermal growth factor receptor (EGFR)-expressing colonic epithelium.
"Endomicroscopy will help to facilitate the early diagnosis of gastric cancer and esophageal cancer," Dr. Kiesslich concluded. "It is a young method, and more studies are warranted. Molecular imaging becomes possible [with this technology] and will shortly open the door for new indications in gastrointestinal endoscopy."