Creating Space for Ide-Cel and Finding Sequencing Options in Multiple Myeloma
Experts debate cutting-edge multiple myeloma treatments, exploring pressing data, the most prominent news, and patient cases.
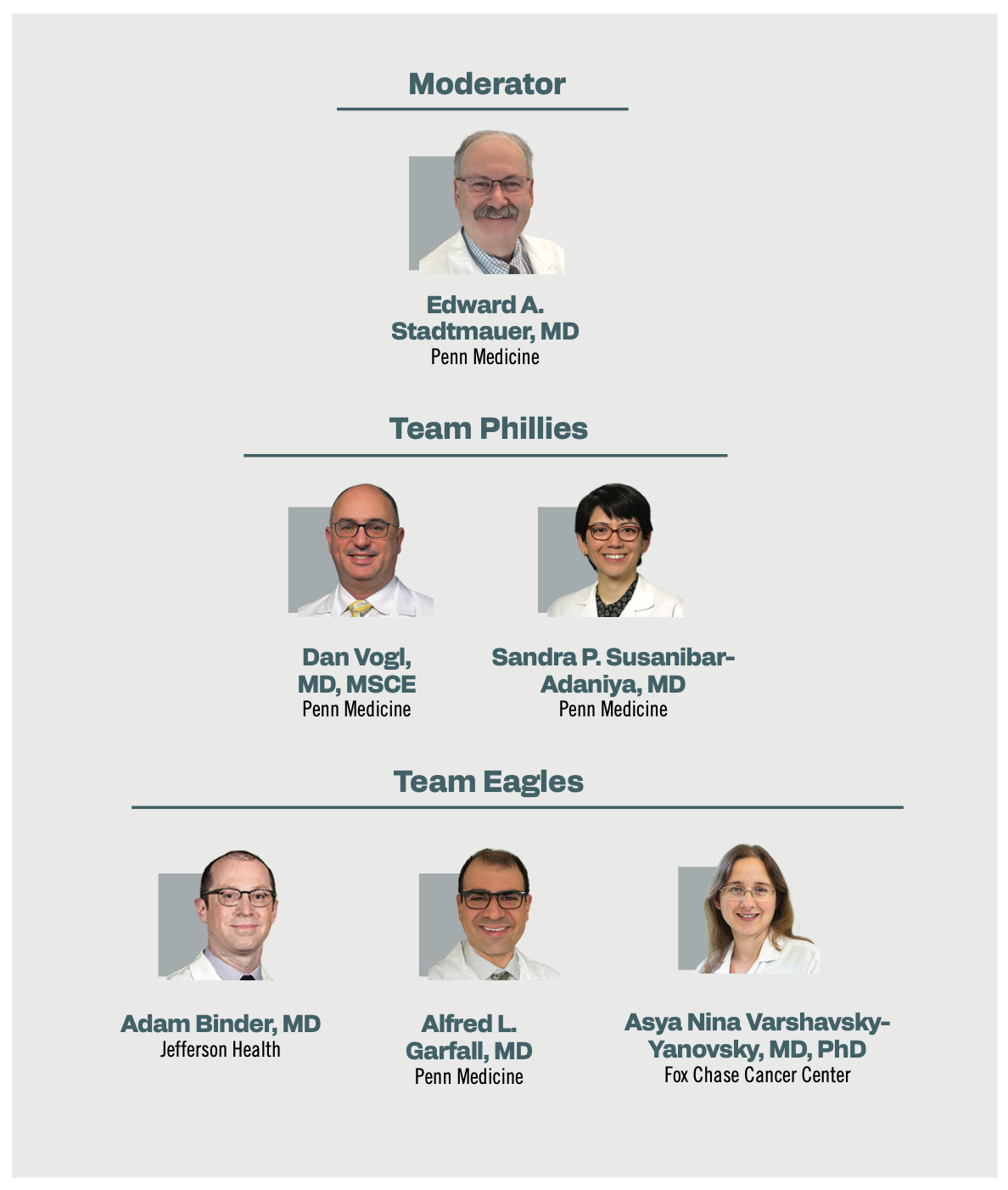
The experts.
On a spring evening in Philadelphia, Pennsylvania, experts in multiple myeloma gathered to debate treatment options in the relapsed/refractory setting. The teams competed in 3 key areas: real-world updates, B-cell maturation antigen (BCMA) or chimeric antigen receptor (CAR) T-cell therapy sequencing, and patient cases.
What is Face-Off? An educational program designed as a competition for teams to present to and against each other.
How does it work? There are 3 rounds: data presentations, topics, and patient cases. During each round, both teams can present and defend their ideas and challenge the other team. The judge determines who is worthy of the top prize.
Round 1: Data Presentation
Team Eagles on Real-World Ide-Cel Results
Presented by Adam Binder, MD
This real-world data set from the Center for International Blood and Marrow Transplant Research (CIBMTR) assessed patients with relapsed/refractory multiple myeloma.1 The data set compared the CIBMTR registry (n = 603) with results from the phase 2 KarMMa trial (NCT03361748; n = 128).2
Between the registry and the trial, the patient characteristics included a median age of 65 years vs 61 years, with 26% vs not available for 70 years or older; 36% vs 26% had penta-refractory disease, and 5% vs 0% had received prior BCMA CAR T-cell therapy. Additionally, 17% vs 39% of patients in the CIBMTR registry and the KarMMa trial had extramedullary disease, 23% vs 35% had high-risk cytogenetics, 16% vs 16% had International Staging System stage III, and the median lines of prior therapy were 7 and 6, respectively.
Efficacy outcomes included a 6-month progression-free survival (PFS) rate of 62% in the CIBMTR registry and a 6-month overall survival (OS) rate of 82%. In the KarMMa trial, the median PFS was 8.6 months, and the median OS was 24.8 months. The overall response rate (ORR) was 71% vs 73%, the very good partial response rate was 53% vs 52%, and the complete response rate or better was 27% vs 33%, respectively.
Notably, cytokine release syndrome (CRS) occurred in 81% of patients in the CIBMTR registry and 84% in the KarMMa trial, with 3% and 5% having grade 3 or higher. Additionally, neurotoxicity was noted in 27% vs 18%, with 4% vs 3% having grade 3 or higher.
A study by Ferreri et al assessed prior BCMA-targeted therapy and idecabtagene vicleucel (ide-cel; Abecma) use.3 For those with prior BCMA therapy, the ORR was 74%, and for those without it, the rate was 88%. Based on the type of prior BCMA therapy, the ORR for those given antibody-drug conjugates (ADCs) was 68%, 86% for those who received bispecifics, and 100% for those who were given CAR T-cell therapy.
Thirty-eight patients received an ADC, mainly belantamab mafodotin-blmf (Blenrep), and 7 patients had not received a prior bispecific antibody.
For those with prior BCMA therapy, the PFS was 3.2 months vs 9.0 months (P = .0002) for those without, and the OS was not reached vs 12.5 months (P = .005). For those given an ADC, the PFS was 3.2 months; those given bispecifics had a PFS of 2.8 months, and prior CAR T-cell therapy had a PFS that was not reached (P = .0004).
Team Phillies on This Evidence
Vogl / I was fascinated by the graph of the different types of prior therapies, because I would have expected the opposite––that patients who had [received] prior ADC with belantamab would probably have a good response to CAR T cells, whereas patients who had [received] a prior bispecific aimed at BCMA would be more likely to have a BCMA-negative relapse and therefore less response to CAR T cells.
Binder / Looking at it initially, it is a little surprising, I agree. The details that aren’t here are how soon after these drug exposures, and did they get their CAR T products? Did it just so happen that they got belantamab right before CAR T, and that maybe would influence response rates? For some reason, there was a longer duration between bispecifics and CAR T therapy because we know the longer you’re off with BCMA-targeted therapy, that’s the predictor of response to CAR T. There wasn’t as much detail here to explain this.
Varshavsky / It’s not surprising [about] the 68% [ORR] in the ADC cohort, but it was striking that this very small number of a total of 12 patients who got T-cell redirecting therapy did incredibly well. They were probably just lucky patients, and 2 received ide-cel, relapsed, received ide-cel again, and responded again. So that’s interesting.
Vogl / If there’s any real takeaway from this real-world study, it’s that those PFS numbers are disappointing. The PFS in the registrational pivotal study was something like close to a year, but in this case, we’re not even seeing more than 9 months. I remember seeing the original ide-cel data from the KarMMa-1 trial, and thinking, “I don’t know if it would beat salvage [therapy]”. It’s just interesting that with BCMA CARs, there’s just such a wide range of responses. It’s different than the CD19 CARs, where there are all these different CD19 CARs out there with different designs and costimulatory domains, and they all work the same. In BCMA, you have some BCMA CARs that went into the clinic and had no responses. There was one…we brought in that had…so-so responses. Then you have ide-cel, which is in the middle, and then you have ciltacabtagene autoleucel [cilta-cel; Carvykti], which is extraordinary. No one has figured out why one works and the other doesn’t.
The Phillies on KarMMa-3 Data
Presented by Dan Vogl, MD, MSCE
Patients with relapsed/refractory multiple myeloma who had received 2 to 4 prior regimens and were treated with either ide-cel or 1 of 5 standard therapies were enrolled in the phase 3 KarMMa-3 trial (NCT03651128).4 Select baseline characteristics included prior treatments, which included either an immunomodulatory agent (88% vs 94%), a proteasome inhibitor (74% vs 72%), or an anti-CD38 monoclonal antibody (95% vs 94%). The median time from diagnosis to screening was 4.1 years in the ide-cel group and 4.0 years in the standard of care group. Additionally, 65% vs 67% of patients had triple-class refractory disease, and 95% vs 93% had disease refractory to daratumumab.
The final PFS analysis highlighted an 18-month PFS rate of 41% in the ide-cel arm vs 19% in the standard-of-care arm. The median PFS was 13.8 months and 4.4 months (HR, 0.49; 95% CI, 0.38-0.63).
In the ide-cel arm, hematologic adverse effects (AEs) of any grade occurred in 90% of patients, grade 3/4 in 93%, and grade 5 in 14%. Any-grade nonhematologic AEs occurred in 58%, grade 3/4 in 24%, and grade 5 in 4%. In the standard regimen arm, any-grade hematologic AEs occurred in 98% of participants, grade 3/4 in 75%, and grade 5 in 6%. Any-grade nonhematologic AEs occurred in 54%, grade 3/4 in 18%, and grade 5 in 2%.
Round 2: Hot Topics
Team Eagles Inspect KarMMa-3 Data
Garfall / What’s interesting to me about KarMMa-3 is that you see a similar pattern with the phase 3 CARTITUDE-4 [NCT04181827] trial. If you look at the responses and duration of response with ide-cel in the third line of therapy and compare it with ide-cel in the sixth line of therapy in KarMMa-1, it looks the same. It doesn’t look like the CAR T cells are working dramatically better when you use them in an earlier line of therapy, which is surprising. All of us anticipated that maybe we would see some cures and plateaus if we use them earlier with healthier T cells, and maybe the cilta-cel to look a little bit better, just like antimyeloma therapy would look a little bit better in the early line of therapy. We’re not seeing that they’re working better when you use them in an earlier line of therapy.
Binder / Keeping that in mind and looking at these curves and thinking about how the landscape of multiple myeloma has changed…, at what point are you thinking about CAR T vs bispecifics and then thinking about some of the newer bispecific data as well, and those PFS curves,…toxicity, and ease of access?
Garfall / This trial also permitted crossover, which we hardly ever see in these types of trials. If you were on the control arm of the study, and you progressed, you could cross over to CAR T cells. Many patients in the control arm received CAR T cells in the next line of therapy. There was no difference in OS, which also informs our thinking about whether we should be rushing to give CAR T cells in the second line of therapy rather than the third or fourth line of therapy. It seems likely that your long-term survival is similar. It just gives you some reassurance that you don’t have to rush to give patients CAR T cells the minute they’re within the label. You can get them a next line of therapy and probably get the same long-term survival as when you’re talking about the risk of CAR T-cell therapy.
Susanibar / You could do the opposite argument, right? Maybe it’s too late because the way we enrolled these patients on the clinical trial, they have to have progressive disease. The disease is growing already on the second to third line. You’re not doing these freezes when the T cells might be the healthiest because they have this growing burden of multiple myeloma that can cause immune dysfunction. There are a lot of benefits in more correlational studies. [The data from] these studies will [enable] us to interpret it and try to choose, right? What’s the fingerprint of the patient who can wait vs the patient who needs this treatment right away?
Varshavsky / It’s a good point. We need to keep in mind that we need 1 more potential salvage, even for bridging, which we all like to look at these days. Also, bringing [us] back to the real-world analysis, you may think they would…do better because these patients didn’t have to wait for confirmed progression [and] didn’t have limitations in bridging therapy, but they did pretty much the same. We still don’t know which subgroup of patients benefits most from each strategy.
Team Eagles on Bispecifics Before CAR T
Presented by Asya Nina Varshavsky-Yanovsky, MD, PhD
Varshavsky / When I may want to do bispecific before CAR T is when a patient is presenting to me as [having] refractory [disease], not second line and not third line. They are coming with an exploding disease. I would love to do CAR T. It will take me 3 weeks to get the patient to gluconeogenesis, and it will take me another 5 weeks to get the patient the actual CAR T product delivered to me. In the meantime, I’m OK with giving selinexor [Xpovio]. In this situation, I am extremely happy that I have those wonderful off-the-shelf products. We are talking about BCMA bispecific. I have 2 wonderful off-the-shelf products [where] I can admit the patients on the same day, see them with their exploding [disease], and start the ramp-up [doses]. The time to first response to these drugs is 1 cycle. The time to best response is around 3 cycles. The toxicity––unlike CAR T, where we are worried about increased toxicities, increased CRS, increased immune effector cell–associated neurotoxicity syndrome, terrible cytopenia, and so on, in patients who have extremely high disease burden––[for the] bispecific does apply, but on a much lesser scale. The toxicities are much more manageable. I can take this patient and this expectation of overall response upwards of 60%. I can get them in a [good], but also deep response. At the end of it, I may keep them on this wonderful drug for as long as they’re responding, which [could] potentially be years. Or I can design a stop date and see [what happens]. This will still not take away my opportunity to do CAR Ts [in the] next line of therapy.
Stadtmauer / Would you ever use a non-BCMA bispecific before doing a CAR T-cell therapy?
Varshavsky / We are all worried about this type of sequencing with potential antigen loss, especially if we are continuing the bispecific through progression as opposed to doing preplanned debulking therapy and moving on to something else. We will not have this concern if we are using a GPRC5D bispecific. In terms of my choice of drug, there are many factors that will affect my choice of BCMA bispecific as opposed to GPRC5D bispecific. If I’m still dead set and getting this patient to BCMA CAR T sooner rather than later, I will offer a GPRC5D bispecific, like talquetamab-tgvs [Talvey]. We’ll plan CAR Ts [in the] next step. It will not take away all my concerns. It will take away my concerns about antigen loss. It will not necessarily take away my concern about T-cell fitness, T-cell exhaustion, or my ability to successfully collect and manufacture the CAR T product. If my goal is to get this very sick patient to CAR T with the hope of giving them this 3-plus years’ PFS from the CAR T, I will favor talquetamab. I will favor debulking and then some treatment holds and some treatment-free period in the hope of getting the T cells to their most functional state, followed by CAR T collection. I may just say, “OK, that’s a great line of therapy. Let’s ride it for as long as it works.” When we get there, we will plan CAR T all over again.
Team Phillies on CAR T Before Bispecifics
Presented by Sandra P. Susanibar-Adaniya, MD
Susanibar / When I treat patients with multiple myeloma, I want to help them live the longest, but with the best quality of life. The [average] patient with multiple myeloma is already in their late 60s, early 70s when they’re diagnosed. What I want for them is the treatment that has a high chance of being effective and can maintain a good quality of life for the longest time. We know that CAR T cell works in [older] patients over the age of 80 with renal failure and has proved to be equally efficacious. If you have a patient who is going to get 1 treatment, and then it’s done, and is 70 and can live the best life ahead of [them] for the next 3 or 4 years and then get a bispecific plus a very good response, why wouldn’t I choose to do that? The risk of infections in CAR T cells is limited, so it’s mostly in the first 3 months, but then it goes down. We have become very good at trying to identify which measures can decrease the infection. It’s that critical period of 3 months that they need more care from us, but then they can go to the community [to receive treatment], and when they go back to the clinic and tell you about their best life, they go on vacation, they’re enjoying the retirement, so they are doing well.
The second thing for me is that you don’t know what’s going to happen later. These 3 years that they haven’t received therapy,…the landscape of multiple myeloma has changed so much in 3 years. You don’t know if they will benefit a lot from this limited- duration bispecific antibody. They get 3 years of treatment, then they get 6 months of bispecific, and then they get maybe…2 more years of treatment. They have this ability to live well.
Then the other thing is the percentage of patients that need treatment because they cannot get to CAR T cells, now that we have the option to do it at second or third line, because it’s approved, it’s reduced. It’s less than 10% [of patients for whom] they did these extraordinary measures that we can do. Maybe we can do just a limited-time bispecific, but for most patients, the treatment that I would prefer is to do CAR T cells and then bispecific, if there are no other CAR T cells that will be approved for patients who have already progressed to CAR T cells.
Binder / For exactly the reasons you said, bispecific before CAR T is perfect. Our goal is to get them to CAR T and maximize their quality of life and durability response. Using a bispecific, like a GPRC5D bispecific, as a holding or bridging phase in which you’re doing it, is an ideal place to use a drug like talquetamab and then get them to CAR T afterward. Because you decrease their disease burden, you minimize that GPRC5D toxicity by just giving a couple of doses. Then you bring them to CAR T afterward. You do bispecific before CAR T. Then, by decreasing their disease burden, you’re minimizing the toxicity that you may experience with CAR T if you try to bring them straight to CAR T without anything beforehand. You may even augment some T-cell activity by doing a bispecific with a different target before a BCMA-targeted CAR T, and then maybe even get a better PFS than you otherwise would have seen with better tolerability and overall better quality of life.
Vogl / What you’re saying is applicable only to patients with incredibly high-risk or high-proliferative disease, where you’re going to be turning to a super-toxic drug like talquetamab for bridging therapy or before going to CAR T cells. For the vast majority of patients, you want to use a treatment that’s going to have the longest PFS, the best data on OS, first, especially because if you go to a CAR T cell first, your likelihood [is] that way down the line, the disease is going to relapse still with the same antigens intact and therefore have better responses to both BCMA, bispecific, GPRC5D, or FCRH5 bispecific whenever it finally gets approved. Those antigens, especially BCMA, are still likely to be there and have to relapse from CAR T, whereas if you go first to a BCMA bispecific, for instance, then you’re possibly leaving yourself without a great option afterwards. It’s only in the highest-risk patients, the patients where you don’t have the option, that you’re going to go to a bispecific first, whether it’s going to a BCMA bispecific because the patient needs something right this second, or using something like talquetamab as a bridging [therapy]. [For] most…patients, you’re going to want to do CAR T cells first.
Round 3: Patient Cases
Team Eagles on Cilta-Cel Use
Presented by Asya Nina Varshavsky-Yanovsky, MD, PhD
• A 70-year-old fit patient with standard-risk, triple-class–exposed relapsed/refractory multiple myeloma, naive to BCMA-targeted therapies, presents for treatment options.
• After progressing on proteasome inhibitors, immunomodulatory drugs, and anti-CD38 monoclonal antibodies, the patient is eligible for cilta-cel therapy.
• This therapy has shown an ORR of 97% and a median PFS of 34.9 months in BCMA-naive populations.
Stadtmauer / I want to know the detailed pathophysiology of the mechanisms and the underlying difference.
Varshavsky / We had a very detailed and heated discussion of whether we want to expose patients when they are planning for BCMA and CAR T to BCMA bispecific, or if we even want to ever do BCMA and CAR T as opposed to BCMA bispecific. That points to prior BCMA exposure decreasing efficacy, including response rates and response duration to BCMA CAR T, and we should also keep in mind that this patient is 70 years old and fit, and potentially maybe less fit and older, if we delay CAR T to the next line of therapy at that time. There is a very strong argument for proceeding with cilta-cel in a patient who is 70 years old and fit, who right now seems to be a good candidate who can handle toxicity and can enjoy the 3 years of PFS as opposed to delaying it.
Stadtmauer / Do we have enough data about the current practice of prior BCMA-targeted exposure?
Garfall / I agree. The data on CAR T cells after prior BCMA-directed therapy are limited. Some of those papers we saw before were talking about [roughly] 7 patients who [received] a prior bispecific and then CAR T cells. The reason is that the more typical patient who [had] a bispecific first, say, on a clinical trial, is still in response. We still have a lot to learn about a typical patient who gets a prior BCMA bispecific, has a good response for a long time, and then progresses [to] what their outcomes are after CAR T-cell therapy. We’ll learn with time. The reason why we feel a lot more comfortable with the opposite sequence is more…that there’s been a much larger volume of reported experience of CAR T cells, and then bispecifics, just the nature of the timing of when these different trials were done. There was just a much larger experience with it so far.
Team Phillies on Ide-Cel Use
Presented by Dan Vogl, MD, MSCE
• A 62-year-old patient with standard-risk, triple-class–exposed relapsed/refractory multiple myeloma presents after 3 prior lines of therapy failed, including proteasome inhibitors, immunomodulatory drugs, and anti-CD38 monoclonal antibodies.
• The patient is fit and eligible for ide-cel therapy, demonstrating improved PFS (13.8 months vs 4.4 months with standard regimens) and a higher ORR (71% vs 42%) in this population.
Vogl / [Regarding] bridging therapy, this is something…we’ve [become] much better at than [what] we used to do on our clinical trials. I don’t even know what the rules were in the ide-cel trials, but in the cilta-cel trials, a lot of times, they had tremendous restrictions on bridging therapy. I guess we’re there to try to make it so that the CAR T cells would not appear better than they were by people getting amazing bridging therapy. We’re seeing that by using good bridging therapy, we can make it easier for people to get through the CAR T cells. We were having a theoretical discussion earlier about whether there is such a thing as too good bridging therapy, where there’s not enough antigen left for the CAR T cells. Maybe we’ll find that out someday, but so far, I don’t think we’ve seen that. Even more than that, in my clinical practice now, [I] treat patients first with something for relapsed/refractory multiple myeloma. Then, as they’re responding to therapy, that’s when I do my apheresis, and then continue the same regimen for bridging. It’s bringing the bridging therapy even before apheresis. That feels like it’s been an effective technique for making the whole process more manageable.
Garfall / In some ways, the big value of having these available earlier has just improved the safety and feasibility. It’s no longer this ranked thing where you’re between scheduling the manufacturing and dealing with relapsed/refractory disease. It just feels very manageable now when you have a good bridging option open. Now that we have readily available manufacturing slots, it’s just a lot easier.
Stadtmauer / We’ve forgotten, a couple of years ago, that we were so limited in the number of cilta-cel slots we had, and basically, we took whatever slot we could get; that was the choice of the product in some ways. Now that has been eliminated as a major barrier. I would say the only somewhat common barrier, and it’s less than 20%, but I would say there are some more manufacturing failures, or at least under specification, for cilta-cel that I’ve seen than ide-cel. Therefore, that…raises the question, if that occurs, do you keep trying to harvest more cells or do another manufacturing, or is that a reason to switch to ide-cel more quickly to get a patient moving along with a BCMA- directed CAR T-cell therapy? But in some ways, that has been my personal practice. The older patients, where I am concerned about the potential toxicity, and then the patients who have some manufacturing difficulty with cilta-cel, are my most common ide-cel uses.
Garfall / The turnaround time for ide-cel is also a little faster than cilta-cel, which is nice. The cilta-cel specifications are very persnickety.
Winner
• Team Eagles with 12 points
• Team Phillies with 8 points
References
- Sidana S, Ahmed N, Akhtar OS, et al. Real world outcomes with idecabtagene vicleucel (ide-cel) CAR-T cell therapy for relapsed/refractory multiple myeloma. Blood. 2023;142(suppl 1):1027. doi:10.1182/blood-2023-181762
- Munshi NC, Anderson LD Jr, Shah N, et al. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N Engl J Med. 2021;384(8):705-716. doi:10.1056/NEJMoa2024850
- Ferreri CJ, Hildebrandt MAT, Hashmi H, et al. Real-world experience of patients with multiple myeloma receiving ide-cel after a prior BCMA-targeted therapy. Blood Cancer J. 2023;13(1):117. doi:10.1038/s41408-023-00886-8
- Rodriguez-Otero P, Ailawadhi S, Arnulf B, et al. Ide-cel or standard regimens in relapsed and refractory multiple myeloma. N Engl J Med. 2023;388(11):1002-1014. doi:10.1056/NEJMoa2213614

Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.
Late Hepatic Recurrence From Granulosa Cell Tumor: A Case Report
Granulosa cell tumors exhibit late recurrence and rare hepatic metastasis, emphasizing the need for lifelong surveillance in affected patients.