CTCs May Help Guide Therapy and Predict Poor Prognosis in Lung Cancer Patients
Circulating tumor cells isolated from early stages of lung cancer may be predictive of poor prognosis and could potentially be predictive biomarkers of disease recurrence.
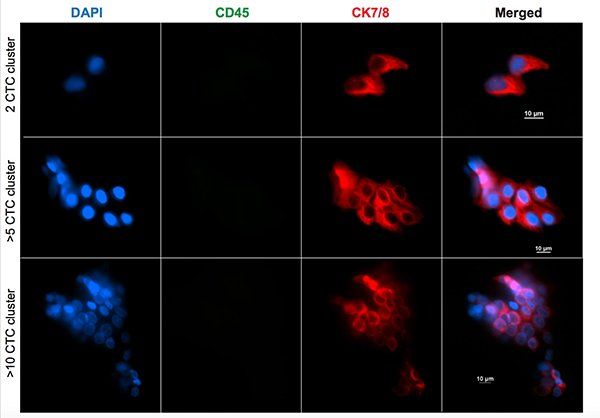
Stained cancer cell clusters. Image © Vasudha Murlidhar
Circulating tumor cells (CTCs) isolated from early stages of lung cancer may be predictive of poor prognosis and could potentially be predictive biomarkers of disease recurrence, according to researchers at the University of Michigan. They report in the journal Cancer Research on analyses revealing enrichment of cell migration and immune-related pathways in CTC clusters, suggesting survival advantage of clusters in circulation. In addition, the researchers report that the clusters display characteristics of therapeutic resistance.
“The most surprising finding is that even in patients with early-stage lung cancer, there are many cells that were present in the pulmonary vein blood,” said study investigator Sunitha Nagrath, professor of chemical engineering at the University of Michigan in Ann Arbor. “Both the frequency and the number of cells were surprising, as was their presence in cluster form. We expected we might find some tumor cells in a few patients, but not to this extent.”
The researchers investigated CTCs in pulmonary vein (PV) blood accessed during surgical resection of tumors. During the perioperative period, PV and peripheral vein (Pe) blood specimens from patients with lung cancer were drawn and assessed for CTC burden. The researchers analyzed 108 blood samples from 36 patients. They found that PV blood had significantly higher numbers of CTCs compared with preoperative Pe and intraoperative Pe blood specimens.
Among the 36 patients, 50% had CTC clusters with large number of CTCs. The researchers discovered that PV often revealed larger clusters. In addition, long-term surveillance suggested that clusters in preoperative Pe blood specimens may predict a poor prognosis. “This study is a step forward to better understanding hematogenous spread,” Nagrath told OncoTherapy Network. “Hopefully soon, researchers can predict in advance who are good candidates for adjuvant therapies based on the CTCs.”
Gene expression analysis showed enrichment of p53 signaling and extracellular matrix involvement in PV and Pe samples. The researchers found Ki67 expression in 62.5% of PV samples and 59.2% of Pe samples. Clusters of two or more tumor cells indicated shorter survival times. Six of the 9 patients whose cancer returned during the 2 to 26 months of follow-up had CTCs appearing in clusters.
While tumor cells from the arm had a median count of around 1.3 per 3 mL, the count in blood from the lung was 7.5 per 3 mL. Among the patients whose lung blood samples revealed hundreds or even thousands of tumor cells, the numbers fell sharply by the time the cells reached the vein in the arm. The researchers hypothesize that the larger clusters are getting stuck in capillaries or that many of these cells can't survive in the bloodstream.