Current Status of Monoclonal Antibody Therapy for Chronic Lymphocytic Leukemia
Despite many therapeutic options for chronic lymphocytic leukemia(CLL), the disease remains incurable. Since monoclonal antibodiesand recombinant toxins that bind surface antigens expressed on themalignant lymphocytes have been developed, targeted therapy hasbecome a vital option in treating CLL. Rituximab (Rituxan), a chimerichuman-mouse anti-CD20 antibody, and alemtuzumab (Campath), ahumanized anti-CD52 monoclonal antibody, have both shown activityin CLL-as single agents and in combination with conventionalchemotherapy. The possibility of combining antibodies has beenexplored as well, with some efficacy. In this review, we discuss theclinical data on the activity of commercially available antibodies inCLL, both as monotherapy and in combination with other agents.
ABSTRACT: Despite many therapeutic options for chronic lymphocytic leukemia (CLL), the disease remains incurable. Since monoclonal antibodies and recombinant toxins that bind surface antigens expressed on the malignant lymphocytes have been developed, targeted therapy has become a vital option in treating CLL. Rituximab (Rituxan), a chimeric human-mouse anti-CD20 antibody, and alemtuzumab (Campath), a humanized anti-CD52 monoclonal antibody, have both shown activity in CLL-as single agents and in combination with conventional chemotherapy. The possibility of combining antibodies has been explored as well, with some efficacy. In this review, we discuss the clinical data on the activity of commercially available antibodies in CLL, both as monotherapy and in combination with other agents.
Chronic lymphocytic leukemia (CLL) is the most common leukemia in the western hemisphere.[ 1] Early-stage CLL (Rai stage I and II) usually requires no therapy and has a median survival of almost 10 years. However, advanced-stage disease (Rai stage III and IV) has a worse prognosis with a median survival of 18 months.[2] Traditionally, CLL has been treated with alkylating agents, steroids, or fludarabine (Fludara), although there is recent evidence demonstrating that initial fludarabine is associated with im proved response rates and progression- free survival.[3] Once patients fail purine analog-based therapy, other therapeutic options are usually limited as they produce modest efficacy and significant toxicity. This mandates the search for innovative approaches that have activity in this disease and can be administered safely in a heavily pretreated older patient population.
Targeted therapy has become an important paradigm for cancer treatment. The selective cytotoxicity of monoclonal antibodies against malignant cells allows for enhanced efficacy with fewer adverse events. Chronic lymphocytic leukemia is an ideal therapeutic model with the identification of a spectrum of well-char- acterized cell surface antigens. It is anticipated that the introduction of monoclonal antibodies in the treatment of CLL will allow for improved outcome, and would permit combinations of biochemotherapy in an effort to cure this devastating leukemia.
Antigens and Antibodies
Ideally, targeted therapy should be directed against tumor-specific antigens that are expressed on malignant cells and not on normal tissue. However, antigens with a restricted range of expression on normal cells that are not critical for survival are acceptable. It is clear that the nature of the target antigen plays an important role in determining the likelihood of therapeutic success. For instance, having a target antigen present in sufficient concentration is essential.
Monoclonal antibodies that are generated from rodents can be immunogenic, with patients generating a human antimouse antibody response. In CLL, the patient's perturbed immune system often precludes this response. This dilemma, however, has been virtually eliminated by humanizing parts of the monoclonal antibody through genetic engineering. In addition, the efficacy of monoclonal antibodies, when used alone, might be limited by their large size, which could prevent adequate penetration in the case of large bulky adenopathy.
TABLE 1

Barriers to Effective Therapy With Unmodified Monoclonal Antibodies
The theoretical basis for combining monoclonal antibodies with conventional chemotherapeutic agents is based on evidence of in vitro synergy. Animal model data support this observation. Also, the timing of anti- antibody administration can be crucial. When monoclonal antibodies are combined with conventional approaches, maximal activity may be witnessed with pretreatment, simultaneous therapy, or after the reduction of bulky disease. Table 1 summarizes the critical issues contributing to therapeutic efficacy with monoclonal antibodies.
Mechanisms of Action
The mechanisms of action of monoclonal antibodies are not fully understood, but antibody-dependent cellular cytotoxicity (ADCC) and complement-mediated cytotoxicity (CMC) are attractive theories.[4] In fact, the immunoglobulin heavychain isotype may be critical, as it interacts with both human complement and Fc receptors to permit cell lysis.[5] Recently, Cartron and colleagues showed that the FcgR3a receptor polymorphism (158V/F) plays an important role in the therapeutic response to rituximab (Rituxan).[6] The FCGR3A-158V/F genotype was determined in 49 patients who had received rituximab for a previously untreated follicular non-Hodgkin's lymphoma. The clinical response and the disappearance of the BCL2-JH gene rearrangement in both peripheral blood and bone marrow were evaluated at 2 months and at 1 year.
The study population consisted of 20% FCGR3A-158V homozygous patients, 35% FCGR3A-158F homozygous patients, and 45% heterozygous patients (FCGR3A-158F carriers). The objective response rates at 2 months and 1 year were 100% and 90%, respectively, in FCGR3A- 158V homozygous patients, compared with 67% (P = .03) and 51% (P = .03), respectively, in FCGR3A- 158F carriers. A disappearance of the BCL2-JH gene rearrangement in both peripheral blood and marrow was observed at 1 year in 5 of 6 homozygous FCGR3A-158V patients compared with 5 of 17 FCGR3A-158F carriers (P = .03)
The homozygous FCGR3A-158V genotype was confirmed to be the single parameter associated with clinical and molecular responses by multivariate analysis.[6] This study- showed an association between the FCGR3A genotype and clinical and molecular responses to rituximab. In addition, although in vitro complement activation clearly enhances the cytotoxicity of rituximab and alemtuzumab (Campath-1H) against hematologic malignant cell lines, the evidence for complement activation in vivo has been less definitive. This issue was addressed in one investigation where there was no clinical correlation between rituximab activity in lymphoma and the expression of inhibitors of complement activators (CD46, CD55, and CD59).[7]
In addition, emerging evidence suggests a role for antibody-induced apoptosis. Byrd and colleagues studied the mechanisms of action of rituximab in patients with B-cell chronic lymphocytic leukemia (B-CLL) and demonstrated activation of caspase 3 and caspase 9, as well as poly(ADPribose) polymerase cleavage in blood leukemia cells immediately following rituximab infusion.[8] These investigators have also shown that significant downmodulation of antiapoptotic proteins occurs. Other groups have provided complementary evidence that apoptosis is one of the mechanistic pathways for monoclonal antibody cytotoxicity.[4,9] In addition, the mechanism of action may be dictated by the targeted tissue compartment (for example, blood vessels, spleen, lymph nodes).
Rituximab in CLL
Rituximab is a chimeric monoclonal anti-CD20 antibody that consists of the murine variable regions of the parent 2B8 murine ant-CD20 grafted onto a human immunoglobulin G1-constant region.[10] The CD20 antigen is an excellent immunotherapy target as it is expressed only on malignant and mature B cells and not on precursor B cells, and the antigen is not shed, internalized, or modulated to a significant degree once antigen-antibody binding has occurred.[11] It is a 33-kD protein, the gene of which is located on chromosome 11q12-q13 and encodes a 297-amino acid, nonglycosylated, tetraspan molecule with intracellular N and C termini and short loops protruding from the cell membrane.[ 12] The precise function of CD20 is still undetermined, although some have suggested that this protein is involved in regulation of calcium flux[13] and cell signaling that affects B-cell growth and differentiation.[ 14] CD20 is expressed at high density (100,000 molecules/cell) on most malignant mature B cells, although this density is lower in B-CLL (8,000 molecules/cell).[5]
The initial pivotal trial that led to rituximab approval showed 6% complete response and 42% partial response, for an overall response of 48% in patients with relapsed indolent non-Hodgkin's lymphoma (NHL).[15] The median duration of response in this trial was 11.6 months. Of the patients treated on that study, 33 had a diagnosis of small lymphocytic lymphoma (SLL). These patients had remarkably lower responses than those with other histologic diagnoses (13% compared with 58%). It is believed that the lower CD20 antigen density and altered pharmacokinetics cause rapid clearance of the drug that may have accounted for the lower response rate. Since then, rituximab has shown efficacy in bulky indolent NHL, previously untreated patients, and in combination with chemotherapy, as discussed later in this article.[16,17]
Refractory or Relapsed Patients
As the CD20 antigen is also expressed on circulating tumor cells in CLL, several investigators have explored the efficacy of this agent in relapsed or refractory patients. Winkler and colleagues reported on 12 patients with fludarabine-resistant CLL or leukemic variants of other low-grade NHLs that were treated with rituximab at 375 mg/m2 once weekly for 4 weeks.[18] The response rates in the CLL patients were modest. There was one complete response (duration of 9 weeks), one partial response (duration of greater than 22 weeks), seven cases of stable disease, and one case of progressive disease. The authors concluded that there is some efficacy for rituximab in CLL, and that further studies were warranted. Since then, Huhn and colleagues reported minimal activity of rituximab in CLL, showing an overall response rate of 25% in 28 previously treated patients, with all responses being partial.[19]
Some investigators explored in- creasing the frequency or the dose of rituximab in order to overcome the poor pharmacokinetic profile in CLL. To this regard, O'Brien et al recently reported the results of a phase I escalation study of rituximab in CLL patients who failed prior traditional therapies.[20] In this study, eligible patients were treated with rituximab in four weekly infusions with escalated doses ranging from 375 mg/m2 to 2,250 mg/m2. The response rate was 36% among 39 evaluable patients, with a suggestion of better response at higher dose levels. All responses were partial. Adverse events were fever, chills, and hypotension, with more side effects at higher dose levels. The median time to disease progression was 8 months. Although there was a suggestion of good activity of rituximab in CLL at these high dose levels, the cost was substantial, and the authors concluded that a better approach would be combining rituximab with other effective agents.
Byrd et al reported another important study in CLL patients who were treated with thrice-weekly rituximab for a total of 12 doses.[21] To assess toxicity, the first cohort of patients received rituximab at 250 mg/m2 three times weekly for 4 weeks. All other treated patients received a dose of 375 mg/m2. Among 29 patients who were assessable for efficacy, one patient achieved a complete response (3%); the overall response rate was 45%. Of the patients who did not respond to therapy, 11 had stable disease, and 3 had evidence of disease progression. Previously untreated patients had a better response rate (83%) compared to patients who had previously received alkylator therapy (30%) or who were refractory to fludarabine (41%), yet this was not statistically significant. The median duration of response in this study was 10 months.
Treatment-Naive Patients
TABLE 2

Selected Clinical Trials With Rituximab in Chronic Lymphocytic Leukemia
Based on the activity in the refractory and relapsed settings, Hainsworth and colleagues administered rituximab to previously untreated CLL patients.[22] A total of 70 patients (39 with SLL and 31 with CLL) were treated with rituximab (375 mg/m2 weekly for 4 weeks) and then reevaluated at 6 weeks. Those with stable disease or an objective response were treated with maintenance rituximab using a standard 4-week schedule, every 6 months, for a maximum of 4 courses. At the time of the report, 57 patients were evaluable, with 44% having an objective response at 6 weeks (9% complete response), and 44% having stable disease. The median progression- free survival in these patients was 35 months. Table 2 summarizes the data of selected clinical trials using rituximab in CLL.[18-22,64]
Despite the evidence of activity of rituximab in CLL patients, there is a clear discrepancy between the high rate of response in follicular lymphoma patients compared with CLL patients. Several factors might contribute to this difference. Expression of CD20 on CLL cells is dim-only 20% to 30% of the level found in patients with follicular lymphoma. In fact, in a study reported by Nguyen and colleagues, the only responding patient had a higher expression of CD20 compared with the nonresponders.[ 23] In addition, soluble CD20 has been demonstrated in the plasma of patients with CLL.[24] It can act as a sink for the antibody (especially with a higher circulating B-cell count), causing rapid clearance of rituximab and resulting in unfavorable pharmacokinetics.[25] The common finding of splenomegaly in patients with SLL or CLL might affect rituximab pharmacokinetics as well.
Others have attempted treating autoimmune hemolytic anemia in CLL patients with rituximab in combination with cyclophosphamide (Cytoxan, Neosar), and dexamethasone. All patients but one achieved normal hemoglobin levels, with a median duration of response in excess of 12 months.[26] However, in their recent update, the same investigators reported that five of the eight responding patients suffered a relapse at a median of 13 months.[27] Those five patients were re-treated with rituximab (375 mg/m2 on day 1), cyclophosphamide (750 to 1,000 mg/m2 on day 2), and 12 mg of dexamethasone given intravenously on days 1 and 2, and orally on days 3 through 7. Cycles were repeated every 4 weeks until the best achievable response was obtained. All five patients achieved a second remission with a median duration of response of 7+ months at the time of the report.[27]
Tolerability
In general, rituximab has been very well tolerated. Side effects are typically confined to the infusion period, and many investigators have described a "cytokine-release syndrome" characterized by fever, chills, nausea, vomiting, hypotension, and occasionally dyspnea.[15,28] Byrd and colleagues noted that these side effects were increased in older patients, and that these reactions were associated with elevated serum levels of inflammatory cytokines, including interleukin (IL)-6, IL-8, tumor necrosis factor-alpha (TNFalpha), and interferon-gamma.[21] Although it is controversial, some investigators have suggested that because this syndrome occurs more frequently during the initial infusion and the high circulating white cell count contributes significantly to the ele- vated cytokine levels,[18,20] this might explain why some patients have developed tumor lysis syndrome with rituximab.[29]
However, tumor lysis syndrome is rarely seen with classic CLL, and most cases have been associated with the leukemic phase of mantle cell lymphoma or prolymphocytic leukemia. Premedicating with steroids during the first cycle or beginning with a 2-day infusion (100 mg of rituximab on day 1 and the remainder on the following day) may minimize this problem. After completion of therapy with rituximab, long-term complications are unusual, with the most common adverse effect being B-cell depletion, lasting 6 to 9 months.[30]
From a practical point of view, the majority of patients receive rituximab at an infusion rate starting at 50 mg/h, and are premedicated with acetaminophen and diphenhydramine. In the absence of symptoms, the infusion rate is increased gradually until completion of therapy. If symptoms are witnessed, the infusion should be stopped and the symptoms managed. Unless it is contraindicated, the antibody should then be given again at a slower rate.
Alemtuzumab in CLL
The original monoclonal antibody Campath-1M was a rat immunoglobulin (IgM), and although it demonstrated in vitro cytotoxicity, there was no evidence of clinical efficacy.[31] Subsequently, a rat IgG2a anti-CD52 monoclonal antibody was produced, and from this a class-switch IgG2b variant was derived (these antibodies differed in their constant region genes). The IgG2b monoclonal antibody (Campath-1G) was capable of eliciting antibody-dependent cellular cytotoxicity by binding human Fc receptors or effector cells and by mediating complement lysis.[32,33] Campath-1G can deplete tumor cells from blood, marrow, spleen, and skin, although it was less effective against lymph nodes or extranodal masses.[ 34] The introduction of genetic manipulation of Ig genes allowed a series of human CD52 antibodies to be produced.[33] The human IgG1 version (alemtuzumab) was chosen for initial trials because it showed optimal activation of cellular and complement-mediated effector mechanisms, making alemtuzumab the first completely humanized monoclonal antibody.[33]
The CD52 protein (21-28 Kd glycosylated glycoprotein)-the function of which is still undefined-is composed of only 12 amino acids attached indirectly to the cell membrane through a glycosylphosphatidylinositol anchor. It is expressed at high density at approximately 5 * 105 molecules/ cell.[35] It is usually present on most normal and malignant mature lymphocytes of T-and B-cell lineages as well as monocytes, is not expressed on hematopoeitic stem cells, and does not modulate in vitro or in vivo.[32,36]
Initial studies with alemtuzumab were performed in patients with NHL, with modest response rates (15% to 20%).[37,38] However, it was hypothesized that CLL could potentially be a better target for this antibody, as alemtuzumab demonstrated tumor regression in the bone marrow and peripheral blood, but not in bulky adenopathy.[37] Based on the preliminary phase I dose-escalation studies, it was recommended that alemtuzumab should be administered at 30 mg three times a week for 4 to 12 weeks. Subsequently, phase II studies were conducted in patients with refractory and relapsed CLL as well as in patients with T-cell prolymphocytic leukemia (PLL).[40]
Osterborg and colleagues investigated alemtuzumab in 29 refractory CLL patients showing a 38% partial response and 4% complete response, for an overall response rate of 42%, and a median duration of response of 12 months.[41] Two recently reported abstracts have confirmed significant activity for alemtuzumab in CLL patients. The first was reported by Keating and colleagues, involving 93 CLL patients who failed fludarabine.[ 42] In this pivotal study, the overall intent-to-treat response rate was 33%, with 2% complete response, 31% partial response, and 59% stable disease. The projected median time to progression is about 9 months.
Kennedy and colleagues reported on 29 patients with refractory CLL who were treated with alemtuzumab, with 59% responding (34% complete response).[43] Peripheral stem cell mobilization and collection did not appear to be affected by alemtuzumab. Nine responding patients pro- ceeded to peripheral blood stem-cell transplantation, with eight of those still alive at a median of 14 months. At the 2001 American Society of Hematology meeting, Rai et al reported on the largest number of patients who received alemtuzumab on a compassionate basis showing 7% complete response in 136 treated patients who had failed prior therapies.[44] The progression-free survival was 7.3 months in responding patients, with an overall response of 40%.
TABLE 3

Alemtuzumab in the Treatment of Chronic Lymphocytic Leukemia and Prolymphocytic Leukemia
Alemtuzumab has also been studied in previously untreated patients with impressive results. Osterborg and colleagues showed an overall response of 89% in a small group of patients, with response duration ranging from 8 to 24 months.[45] Followup bone marrow examination is critical in patients receiving alemtuzumab, as peripheral blood remissions will often precede marrow clearing by several weeks. Table 3 summarizes pivotal studies with alemtuzumab in CLL.[40-44,46]
Studies in PLL
Pawson and colleagues studied the efficacy of alemtuzumab in 15 patients with T-cell PLL.[39] Eleven patients (73%) had a major response, with nine (60%) achieving complete response. Re-treatment was feasible in three relapsed patients who achieved a complete response again, and two of those patients underwent autologous peripheral stem cell transplant. Dearden and colleagues recently showed that patients with refractory PLL have an excellent response to alemtuzumab.[40] Although this response is usually not sustained, patients who undergo consolidative high-dose chemotherapy with autologous or allogeneic bone marrow transplantation appear to have longer disease-free intervals.[40]
Side Effects
Intravenous administration of alemtuzumab is almost always associated with "first dose" reactions characterized by fever, rigors, and nausea due to cytokine release (TNF and IL-6).[41,45] Such reactions are not seen with subcutaneous administration, although local injection site reactions may occur.[ 41,46] Antiglobulin responses have not been observed with alemtuzumab. The major side effect is prolonged lymphopenia (both T and B cells) and profound immunosuppression, resulting in an increased risk of opportunistic infections, especially in heavily pretreated patients.[37,41,47] Lymphopenia mandates instituting prophylactic antibiotics once alemtuzumab therapy is initiated.
Antimicrobial prophylaxis is recommended for a minimum of 2 months following the last dose of alemtuzumab or until CD4+ counts are above 200 cells/mL. The median time to recovery of CD4+ counts to that level was 2 months; however, full recovery (to baseline) of CD4+ and CD8+ counts may take more than 12 months. Hematologic toxicity (neutropenia and thrombocytopenia) has been witnessed in all alemtuzumab phase II studies, and rare cases of severe fatal marrow aplasia have also been reported.[39,41,37]
Recently, several reports of cytomegalovirus (CMV) reactivation have been documented in patients treated with alemtuzumab. Thai and colleagues studied the incidence of such an infection in 34 patients with PLL or CLL who were treated with alemtuzumab between 1998 and 2001 at Stanford University.[48] Although all patients received prophylactic antibiotics and antivirals, five patients (15%) developed CMV viremia at a median of 28 days after the first alemtuzumab infusion. All affected patients had a fever above 38.5°C, but otherwise normal chest radiographs and normal chemistries with nega- tive bacterial blood cultures. All patients responded to ganciclovir (Cytovene) with resolution of their fever and viremia. The authors were not able to identify specific risk factors for developing CMV viremia, although a trend toward statistical significance was almost reached in patients with prior rituximab exposure (P = .07). Although the incidence of CMV viremia is not high, it is important to consider the diagnosis in any febrile patient who is undergoing alemtuzumab therapy.
Rituximab in Combination Therapy in CLL
Although many chemotherapeutic agents have been used with success in CLL, none has been proven curative. Fludarabine has shown better activity than alkylating agents in chemotherapy- naive patients, although the overall survival in randomized trials was not statistically different.[ 3,49] Because rituximab has shown activity without significant toxicity in CLL, as discussed above, investigators have attempted to combine conventional therapies with the antibody-based approach. Byrd and colleagues reported preliminary results of a Cancer and Leukemia Group B trial (CALGB-9712) conducted as a randomized phase II study comparing concurrent rituximab and fludarabine with the same agents given sequentially.[50]
Patients on the concurrent arm received fludarabine at 25 mg/m2/d (days 1-5, cycles 1-6), and rituximab at 375 mg/m2 (days 1 and 4 of cycle 1, and day 1 of cycles 2-6). Patients on the sequential arm received fludarabine as in the concurrent regimen followed by a 2-month therapy hiatus, then rituximab at 375 mg/m2/wk for 4 weeks. Both arms included previously untreated patients. Preliminary results suggest better response in the concurrent arm (90% vs 77% overall response), and a complete response rate that reached statistical significance (47% compared with 28%, P = .04).
Others have reported similar efficacy with this combination. Schulz and colleagues treated CLL patients who were anthracycline- and fludarabinenaive with overlapping cycles of fludarabine (25 mg/m2/d, days 1-5, cycles 1-4) and rituximab (375 mg/m2 on day 1 of cycles 3-6). The overall response rate in 29 evaluable patients was 90%, with 34% achieving a complete response.[51] Although this combination is showing promising results, its superiority to single-agent fludarabine or other traditional therapies requires confirmation in phase III randomized studies.
FCR Protocol
Since fludarabine has shown in vitro and in vivo synergy with alkylating agents,[52] specifically cyclophosphamide,[ 53] investigators have attempted a triple regimen combination with fludarabine, cyclophosphamide, and rituximab (FCR) in an effort to improve response rates in refractory patients and those who were previously untreated. Garcia- Manero and colleagues treated relapsed CLL patients with FCR (rituximab at 375 mg/m2 on day 1 of cycle 1 and 500 mg/m2 on day 1 of cycles 2-6, fludarabine at 25 mg/m2 on days 2-4 of cycle 1 and days 1-3 of cycles 2-6, and cyclophosphamide at 250 mg/m2 on days 2-4 of cycle 1 and days 1-3 of cycles 2-6).[54] To date, 136 patients are evaluable for response, 28 (21%) of whom achieved a complete response, and 68 (50%) of whom obtained a partial response, for an overall response rate of 71%. Complete molecular remission was observed in 5 of the 14 complete response patients (36%) using polymerase chain reaction (PCR) technology on bone marrows from these patients. The same regimen was tested in previously untreated patients, yielding higher response rates.
TABLE 4
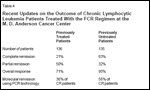
Recent Updates on the Outcome of Chronic Lymphocytic Leukemia Patients Treated With the FCR Regimen at the M.D. Anderson Cancer Center
Wierda and colleagues reported on 135 evaluable patients treated with the same FCR protocol mentioned above. Eighty-five patients (63%) had a complete response, with a molecular remission demonstrated in the bone marrow of 56% of complete response patients (as detected by PCR assay).[55] At a median follow-up of 12 months, median time to treatment failure has not been reached (Table 4). In both studies, the combination therapy was well tolerated without increased toxicity compared to historical controls. Nausea was observed in 20% of patients, while fatigue, vomiting, and diarrhea were noted in 11%, 6%, and 2%, respectively. Although the incidence of grade 4 neutropenia was observed with higher frequency than in patients treated with fludarabine and cyclophosphamide alone, there was no increase in the incidence of major infections (sepsis or pneumonia).
The current FCR regimen shows excellent activity and compares favorably with all prior regimens for CLL. The activity and superiority of this regimen, however, requires validation in a larger randomized multiinstitutional study before being advocated as a new standard of care.
Rituximab and Pentostatin
A phase II multicenter trial to evaluate the safety and efficacy of pentostatin (Nipent) in combination with rituximab in patients with low-grade NHL and CLL is under way.[56] Patients in this study receive rituximab on day 1 at 375 mg/m2 followed by both agents on days 8, 15, and 22. Pentostatin is given at a dose of 4 mg/m2. Cycles are repeated after 1 week of rest. The outcome of this ongoing trial is not yet available, but the interest in adding antibodies to conventional agents proves a shift toward a more targeted approach in CLL. As discussed previously, others have attempted treating autoimmune hemolytic anemia in CLL patients with rituximab, cyclophosphamide, and dexamethasone with promising results.
Alemtuzumab in Combination Therapy in CLL
Few reports have been published on alemtuzumab in combination with conventional therapies. The immunosuppression observed with alemtuzumab mandates exercising caution when adding this antibody to other agents; administering prophylactic antibiotics is warranted until patients are no longer at increased risk for opportunistic infections. Kennedy and colleagues treated five patients who were extremely refractory to traditional therapies with a combination of alemtuzumab and fludarabine.[57] In this study, all patients were refractory to fludarabine alone and to alemtuzumab alone. Patients received alemtuzumab for 8 to 16 weeks at a dose of 30 mg three times per week intravenously, with fludarabine at 25 mg/m2 for 3 to 5 days every 4 weeks during alemtuzumab therapy. Four of the five patients responded, with two achieving a complete response and two obtaining a partial response.
In all four responding patients, bone marrow examination showed no evidence of CLL, and molecular studies failed to demonstrate evidence of minimal residual disease. Despite the theoretical concern that patients receiving such a combination are at increased risk of opportunistic infections, none of these five patients had serious infections. Patients on this study, however, received prophylactic antifungals, and were monitored frequently for possible CMV reactivation. In a recently published update, these investigators confirmed their results and reported on a total of six patients. Of the five patients that responded, three had no morphologic evidence of CLL in their bone marrow.[58]
Currently, large randomized studies are being conducted in untreated CLL patients using either the combination of fludarabine and alemtuzumab or a sequential regimen of both agents. Theoretically, the combined arm would have more toxicity than the sequential arm. Results of these ongoing trials are not yet published, but it is anticipated that the standard approach to CLL will change in the near future, and that monoclonal antibodies will make their way into frontline therapy and into combination regimens.
Antibody Combinations
TABLE 5

Phase I Study of Alemtuzumab/Rituximab in Relapsed or Refractory CLL: Study Schema
In light of the fact that monoclonal antibody-based therapy is well tolerated and produces minimal side effects, we have initiated at Northwestern University a phase I study combining alemtuzumab with rituximab in patients with refractory and/or relapsed CLL.[59] Eligible patients must have a confirmed diagnosis of CLL or small lymphocytic lymphoma (SLL) in the leukemic phase. Patients must have expressed both CD20 and CD52, and have had adequate bone marrow reserve unless cytopenia is related to extensive bone marrow involvement. Patients must have failed traditional therapies. Prior exposure to alemtuzumab is not allowed, but prior exposure to rituximab is permitted if the last infusion was administered more than 6 months prior to initiating the current regimen. Patients have received therapy as outlined in the study schema in Table 5.
All patients receive premedication with diphenhydramine and acetaminophen. Fever and rigors are treated with hydrocortisone at 100 mg and/or meperidine at 25 mg, both given intravenously. Blood cultures are obtained where clinically indicated. Other infusion-related side effects (dyspnea, hypoxemia, and hypotension) are managed by temporary cessation of the infusion, hydration, and the appropriate medical intervention. Once these side effects are resolved, the infusion can be restarted at half the previous infusion rate. Because alemtuzumab produces major infectious complications, all patients are placed on trimethoprim and sulfamethoxazole DS three times weekly, fluconazole (Diflucan) daily, and acyclovir twice daily. These prophylactic antibiotics are continued until 2 months after completion of therapy or until recovery of CD4+ counts. Neutropenic patients are started on ciprofloxacin (Cipro), and the use of growth factor is allowed but not required.
At the time of our report, nine patients had already been enrolled, one of whom obtained a partial response by National Cancer Institute criteria, and a decline in absolute lymphocyte count had been noted in eight patients.[ 60] It should be noted that in this study, the combination has been well tolerated, without opportunistic infections, and that the infusionrelated toxicity is similar to what is usually reported with each antibody as monotherapy. We are currently expanding this study to administer alemtuzumab for a total of 8 to 12 weeks. Once the feasibility of this combination is achieved, a phase II study of the same regimen will be initiated. It is foreseeable that incorporating highdose rituximab in this regimen might produce a better response, but confirmatory trials are required.
In a similar study, Faderl and colleagues treated patients who expressed CD20 and CD52 with alemtuzumab and rituximab. Patients received rituximab at the standard dose for 4 weeks, and alemtuzumab at 3, 10, and 30 mg on days 3, 4, and 5 of week 1, and at 30 mg intravenously on days 3 and 5 weekly during weeks 2 through 4.[61] One patient obtained a complete response; the overall response rate was 43%. The combination was well tolerated without significant toxicity. Having established the feasibility of combining alemtuzumab and rituximab in this patient population will allow the addition of conven- tional chemotherapeutic agents to such a combination. Others have combined rituximab with epratuzumab (anti- CD22, LymphoCide) in relapsed or refractory NHL, and have concluded that this combination is safe and well tolerated, but that its efficacy remains to be determined.[62]
Other Antibodies
Several antibodies have been generated that recognize CLL antigens; these are currently under investigation. Link and colleagues reported preliminary results of a phase II study utilizing apolizumab (Hu1D10, Remitogen), a monoclonal antibody generated against HLA-DR expressed on normal and malignant B cells. Patients received the antibody at 0.5 or 1.5 mg/kg once weekly for 4 consecutive weeks.[63] At the time of the report 21 patients were treated, five of whom had small lymphocytic histology. Although response data were not available, the authors commented on the feasibility of administration and on the limited side effects that were essentially related to infusion- related symptoms. An anti-CD23 agent is currently under development as well.
Conclusions
As we enter the new millennium, targeted therapy with monoclonal antibodies has revolutionized the approach to select malignant disorders. These antibodies are, in general, better tolerated than conventional chemotherapy, and can be combined together and with other agents. The ability of administering these antibodies to older patients who are heavily pretreated will hopefully allow for improved outcomes in treating challenging entities such as refractory CLL. Although CLL generally remains an incurable disease, these new therapeutic options reflect the dawn of a new era and the potential for more effective control of this devastating disease.
References:
1.
Greenlee RT, Murray T, Bolden S, et al:Cancer statistics, 2000. CA Cancer J Clin 50:7-33, 2000.
2.
Rai KR, Sawitsky A, Cronkite EP, et al:Clinical staging of chronic lymphocytic leukemia.Blood 46:219-234, 1975.
3.
Rai KR, Peterson BL, Appelbaum FR, etal: Fludarabine compared with chlorambucil asprimary therapy for chronic lymphocytic leukemia.N Engl J Med 343:1750-1757, 2000.
4.
Larson S, Divgi C, Sgouros G, et al: Monoclonalantibodies: Basic principles, radioisotopeconjugates, in Rosenberg SA (ed):Principles and Practice of the Biologic Therapyof Cancer, pp 396-412. Philadelphia, LippincottWilliams &Wilkins, 2000.
5.
Dyer M, Osterborg A: The use of therapeuticmonoclonal antibodies in chronic lymphocyticleukemia, in Cheson B (ed): ChronicLymphocytic Leukemias, pp 335-352. NewYork, Marcel Dekker, 2001.
6.
Cartron G, Dacheux L, Salles G, et al:Therapeutic activity of humanized anti-CD20monoclonal antibody and polymorphism in IgGFc receptor FcgRIIIa gene. Blood 99:754-758,2002.
7.
Weng WK, Levy R: Expression of complementinhibitors CD46, CD55, and CD59 ontumor cells does not predict clinical outcomeafter rituximab treatment in follicular non-Hodgkin lymphoma. Blood 98:1352-1357,2001.
8.
Byrd JC, Kitada S, Flinn IW, et al: Themechanism of tumor cell clearance by rituximabin vivo in patients with B-cell chroniclymphocytic leukemia: Evidence of caspaseactivation and apoptosis induction. Blood99:1038-1043, 2002.
9.
Shan D, Ledbetter JA, Press OW: Apoptosisof malignant human B cells by ligation ofCD20 with monoclonal antibodies. Blood91:1644-1652, 1998.
10.
Reff ME, Carner K, Chambers KS, et al:Depletion of B cells in vivo by a chimericmouse human monoclonal antibody to CD20.Blood 83:435-445, 1994.
11.
Anderson KC, Bates MP, SlaughenhouptBL, et al: Expression of human B cell-associatedantigens on leukemias and lymphomas: Amodel of human B cell differentiation. Blood63:1424-1433, 1984.
12.
Tedder TF, Disteche CM, Louie E, et al:The gene that encodes the human CD20 (B1)differentiation antigen is located on chromosome11 near the t(11;14)(q13;q32) translocationsite. J Immunol 142:2555-2559, 1989.
13.
Tedder TF, Streuli M, Schlossman SF, etal: Isolation and structure of a cDNA encodingthe B1 (CD20) cell-surface antigen of humanB lymphocytes. Proc Natl Acad Sci U S A85:208-212, 1988.
14.
O’Keefe TL, Williams GT, Davies SL, etal: Mice carrying a CD20 gene disruption. Immunogenetics48:125-132, 1998.
15.
McLaughlin P, Grillo-Lopez AJ, LinkBK, et al: Rituximab chimeric anti-CD20 monoclonalantibody therapy for relapsed indolentlymphoma: Half of patients respond to a fourdosetreatment program. J Clin Oncol 16:2825-2833, 1998.
16.
Davis TA, White CA, Grillo-Lopez AJ,et al: Single-agent monoclonal antibody efficacyin bulky non-Hodgkin’s lymphoma: Resultsof a phase II trial of rituximab. J Clin Oncol17:1851-1857, 1999.
17.
Gutheil J, Finucane D, Rodriguez R, etal: Phase II study of Rituximab (Rituxan) inpatients with previously untreated low-gradeor follicular non-Hodgkin’s lymphoma (abstract79). Proc Am Soc Clin Oncol 19:22a, 2000.
18.
Winkler U, Schulz H, Jensen M, et al:Toxicity and efficacy of the anti-CD20 antibodyrituximab (Rituxan) in patients with Bcellchronic lymphocytic leukemia: A phase I/II study (abstract 1396). Blood 94:312a, 1999.
19.
Huhn D, von Schilling C, Wilhelm M, etal: Rituximab therapy of patients with B-cellchronic lymphocytic leukemia. Blood 98:1326-1331, 2001.
20.
O’Brien SM, Kantarjian H, Thomas DA,et al: Rituximab dose-escalation trial in chroniclymphocytic leukemia. J Clin Oncol 19:2165-2170, 2001
.
21.
Byrd JC, Murphy T, Howard RS, et al:Rituximab using a thrice weekly dosing schedulein B-cell chronic lymphocytic leukemia andsmall lymphocytic lymphoma demonstratesclinical activity and acceptable toxicity. J ClinOncol 19:2153-2164, 2001.
22.
Hainsworth J, Litchy S, Burris H, et al:Rituximab as first-line and maintenance therapyfor patients with small lymphocytic lymphoma(SLL) and chronic lymphocyticleukemia (CLL) (abstract 1530). J Clin Oncol20:4261-4267, 2002.
23.
Nguyen DT, Amess JA, Doughty H, etal: IDEC-C2B8 anti-CD20 (rituximab) immunotherapyin patients with low-grade non-Hodgkin’s lymphoma and lymphoproliferativedisorders: evaluation of response on 48 patients.Eur J Haematol 62:76-82, 1999.
24.
Manshouri T, Saffer H, Keating M: Clinicalrelevance of circulating CD 20 (cCD 20) inpatients with chronic lymphocytic leukemia(CLL) (abstract 1595). Blood 96:369a, 2000.
25.
Petryk M, Grossbard M: Rituximab therapyof B-cell neoplasms. Clin Lymphoma 1:186-194, 2000.
26.
Rai K, Gupta N, Janson D, et al: Rituximab/cyclophosphomide/dexamethasone combinationhighly effective in autoimmunehemolytic anemia associated with chronic lymphocyticleukemia (abstract 3264). Blood96:754a, 2000.
27.
Gupta N, Patel D, Kavuru S, et al: Retreatmentwith a rituximab based therapy ishighly effective in autoimmune hemolytic anemia(AIHA) associated with chronic lymphocyticleukemia (CLL) (abstract 1529). Blood98:363a, 2001.
28.
Byrd JC, Waselenko JK, Maneatis TJ, etal: Rituximab therapy in hematologic malignancypatients with circulating blood tumorcells: Association with increased infusion-relatedside effects and rapid blood tumor clearance.J Clin Oncol 17:791-795, 1999.