Commentary (Witta/Bunn): Second-Line Treatment of Small-Cell Lung Cancer
In this issue of ONCOLOGY, Dr.John Eckhardt provides an excellentreview of the challenge oftherapy for patients with small-celllung cancer (SCLC) who relapse afterfirst-line therapy. Dr. Eckhardt outlinesthe prognostic factors influencingresponse to second-line treatment,survival, and treatment-related toxicity.These prognostic factors includethe response to first-line therapy, theprogression-free interval, and performancestatus. The influence of the chemotherapyregimen and the durationof treatment on symptom palliationand quality of life are also discussed.Dr. Eckhardt provides an excellentsummary of the activity of multipleagents in the second-line setting.
In this issue of ONCOLOGY, Dr. John Eckhardt provides an excellent review of the challenge of therapy for patients with small-cell lung cancer (SCLC) who relapse after first-line therapy. Dr. Eckhardt outlines the prognostic factors influencing response to second-line treatment, survival, and treatment-related toxicity. These prognostic factors include the response to first-line therapy, the progression-free interval, and performance status. The influence of the chemotherapy regimen and the duration of treatment on symptom palliation and quality of life are also discussed. Dr. Eckhardt provides an excellent summary of the activity of multiple agents in the second-line setting.
Survival Benefit?
TABLE 1
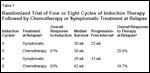
Randomized Trial of Four or Eight Cycles of Induction Therapy Followed by Chemotherapy or Symptomatic Treatment at Relapse
The first question relating to second- line therapy is the issue of whether there is any survival benefit to such therapy. There are few randomized trials that address this issue, but perhaps the most important was conducted by the Cancer Research Campaign in the United Kingdom.[1] This was a four-arm trial that ad-dressed the issue of optimal number of induction therapy cycles as well as therapy at relapse. The results are summarized in Table 1. Patients treated with four cycles of induction therapy who received no therapy at relapse had a significantly worse survival (median: 30 weeks) compared to those who received second-line chemotherapy at the time of relapse (median: 38-42 weeks; P = .04). These data indicate that some therapy should be offered to at least some SCLC patients who relapse after initial therapy.
Patient Selection
Assuming patients are offered additional therapy, the next questions are which patients and which therapy. Currently, there is no accepted standard approach for treating relapsed SCLC. Since there is no evidence that relapsed patients can be cured, the goal in this setting is clearly palliation.
Although most patients relapse at multiple sites, some patients relapse at a solitary site or have severe symptoms referable to a single site in the presence of multiple metastases. Although not discussed in Eckhardt's review, these patients should be offered palliative radiation therapy. In a study from the National Cancer In stitute (NCI), palliative chest radiotherapy led to objective remissions in 52% of extensive SCLC patients with local progression.[2] Higher doses of radiation (60 Gy) may correlate with higher local response rates.[3] Radiotherapy may also palliate symptomatic bone and central nervous system metastases.
The time since initial therapy should be a major factor in the choice of therapy. As indicated in Eckhardt's review, patients who fail to respond to induction therapy or who progress or relapse within 10 to 12 weeks are the least likely to benefit from any known therapy. These patients are also good candidates for clinical trials of novel therapies. Several chemotherapy agents have been studied in these settings. Paclitaxel alone produced a partial response in 7 (29%) of the 21 patients who relapsed within 3 months after being treated with CDE (cyclophosphamide [Cytoxan, Neosar], doxorubicin, etoposide).[4] When paclitaxel was combined with carboplatin (Paraplatin) in patients resistant to CDE, 23 (73%) of 34 patients had a partial response with a median survival of 31 weeks.[5] When carboplatin was combined with vincristine, 8 (36%) of 22 patients who relapsed less than 3 months after the first treatment had a partial response.[6]
Choice of Chemotherapy
Dr. Eckhardt's review notes that many different chemotherapy agents can produce objective responses in 20% or more of SCLC patients who relapse or progress more than 10 to 12 weeks after induction therapy. What is not clear in this review are the choices for patients who relapse more than 6 months after a response to induction therapy.
As early as 1983, the NCI-VA group reported that patients relapsing 2 or more years after induction therapy had an 80% objective response rate to the same induction therapy and that the median duration of response was 10 months.[7] These results, which were confirmed and extended in at least three other studies, are superior to those reported with the new agents in Dr. Eckhardt's review. A report by Postmus et al showed that patients with a progression- free interval lasting more than 34 weeks were more likely to respond to re-treatment with CDE compared to those with a shorter progression- free interval (79% vs 44%, respectively, P < .05).[8]
Similar results were reported by Giaccone et al.[9] In their study, patients who relapsed more than 10 weeks after induction therapy had a response rate of 50% compared to 15% for those who relapsed < 10 weeks after induction therapy when rechallenged with the same therapy. Finally, Vincent et al reported a partial response rate of 67% in patients with SCLC who were rechallenged with chemotherapy similar to their induction treatment. Patients who had a response longer than 8 months were more likely to have a second response of more than 2 months' duration (P = .02).[10]
Other Predictive Factors
Another factor in the choice of second-line therapy is the response to initial therapy. Patients with an initial complete response are more likely to respond to re-treatment with the same regimen than patients with a lesser response. For example, Postmus et al reported that CDE re-treat-ment produced responses in 18 (78%) of 23 patients who had a complete response to CDE compared with only 5 (35%) of 14 patients who had a partial response to initial treatment (P < .01).[8] The Southwest Oncology Group (SWOG) reported similar results.[11]
Two studies suggest that the number of cycles of induction therapy can influence response to second-line therapy. The SWOG reported that fewer initial courses of chemotherapy correlated with more successful salvage therapy.[11] Similar results were reported for the randomized trial by Spiro et al, in which the second- line response was 25.6% among patients receiving four induction cycles vs 19% in those given eight induction cycles.[1]
Although SCLC patients with good performance status are most likely to be treated with a combination, the optimal number of agents is unclear. In the first-line setting, there is no evidence that any three-drug combination is superior to two drug combinations such as etoposide/cisplatin, etoposide/carboplatin, or irinotecan (Camptosar)/cisplatin. There are several phase II studies of threedrug combinations in the second-line setting but no phase III trials.
One randomized phase II trial evaluated the two-drug combination of etoposide/cisplatin (EP) and the threedrug combination of etoposide/cisplatin and carboplatin (EPC) in SCLC patients who progressed after firstline treatment.[12] The response rates were higher in the EPC group (47%) than in the EP group (29%), but the differences were not significant (P = .20). The median survival favored the EPC group (7.6 vs 4.3 months), but the 1-year survival rates were similar (19% vs 18%) and there were no significant differences in overall survival. Thus, there is no evidence for the routine use of any three-drug combination in the second- line setting.
Conclusions
In summary, SCLC patients who relapse or progress after initial therapy should be considered for additional therapy because there is evidence that it can improve survival and alleviate symptoms in such patients. Several factors-including performance status, response to induction therapy, time since induction therapy, and sites of symptoms-should be considered in the selection of therapy.
For patients with an initial complete response and/or 6 months or more of progression-free survival, retreatment with the original therapy can be considered. For patients with a progression-free interval of 3 to 6 months, therapy with a different class of chemotherapeutic agent should be considered. Although two-drug combinations produce higher response rates, there are no randomized trials that prove they are superior to a single agent. Clinical trials should be encouraged in this setting. There are no studies suggesting that three-drug combinations are indicated.
For patients who progress during initial therapy or within 10 to 12 weeks from induction therapy, options include a clinical trial or an established single agent or two-drug combination with a different mechanism of action. Palliative radiation to symptomatic sites should be considered in all patients with disease progression.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Spiro SG, Souhami RL, Geddes DM, et al: Duration of chemotherapy in small cell lung cancer: A Cancer Research Campaign trial. Br J Cancer 59:578-583, 1989.
2. Ihde DC, Bilek FS, Cohen MH, et al: Response to thoracic radiotherapy in patients with small cell carcinoma of the lung after failure of combination chemotherapy. Radiology 132:443-446, 1979.
3. Salazar OM, Yee GJ, Slawson RG, et al: Radiation therapy for chest recurrences following induction chemotherapy in small cell lung cancer. Int J Radiat Oncol Biol Phys 21:645-650, 1991.
4. Smit EF, Fokkema E, Biesma B, et al: A phase II study of paclitaxel in heavily pretreated patients with small-cell lung cancer. Br J Cancer 77:347-351, 1998.
5. Groen HJ, Fokkema E, Biesma B, et al: Paclitaxel and carboplatin in the treatment of small-cell lung cancer patients resistant to cyclophosphamide, doxorubicin, and etoposide: A non-cross-resistant schedule. J Clin Oncol 17:927-932, 1999.
6. Smit EF, Berendsen HH, De Vries EGE, et al: A phase II study of carboplatin and vincristine in previously treated patients with small cell lung cancer. Cancer Chemother Pharmacol 25:202-204, 1989.
7. Batiste G, Ihde DC, Zabell A, et al: Smallcell carcinoma of lung: Reinduction therapy after late relapse. Ann Intern Med 98:472-474, 1983.
8. Postmus PE, Berendsen HH, van Zandwijk N, et al: Retreatment with the induction regimen in small cell lung cancer relapsing after an initial response to short term chemotherapy. Eur J Cancer Clin Oncol 23:1409-1411, 1987.
9. Giaccone G, Dalesio O, McVie GJ, et al: Maintenance chemotherapy in small-cell lung cancer: Long-term results of a randomized trial. European Organization for Research and Treatment of Cancer Lung Cancer Cooperative Group. J Clin Oncol 7:1230-40, 1993.
10. Vincent M, Evans B, Smith I, et al: Firstline chemotherapy rechallenge after relapse in small cell lung cancer. Cancer Chemother Pharmacol 21:45-48, 1988.
11. Albain KS, Crowley JJ, Hutchins L, et al: Predictors of survival following relapse or progression of small cell lung cancer. Southwest Oncology Group Study 8605 report and analysis of recurrent disease data base. Cancer 72:1184-1191, 1993.
12. Schlier JP, Lafitte JJ, Lecomte J, et al: A phase II randomized trial comparing the cisplatin- etoposide combination chemotherapy with or without carboplatin as second-line therapy for small-cell lung cancer. Ann Oncol 13:1454-1459, 2002.