Current Treatments in Mantle Cell Lymphoma
Avyakta Kallam, MBBS and Julie Vose MD, MBA, review available treatment options for patients with mantle cell lymphoma.
Introduction
Mantle cell lymphoma (MCL) is a disease of older patients with a median age of 65 years. It accounts for 5% to 7% of all non-Hodgkin lymphoma (NHL) cases in North America.1-5Approximately 4000 cases are diagnosed every year, with disease prevalence estimated to be 20,000 cases. The initial studies among patients with MCL showed poor outcomes after standard chemotherapy, with a median survival of 3 years. Over the past 2 decades, significant progress has been made in the risk stratification and treatment of MCL.
MCL has varied presentations, and most patients present with palpable lymphadenopathy, with or without systemic presentations.6-8 More than 80% of patients present with stage III/ IV disease at the time of diagnosis, with bone marrow involvement,9 and approximately 30% of patients present with generalized symptoms, such as fever, night sweats, and weight loss. Central nervous system involvement at the time of diagnosis is unusual and associated with poor outcomes.
Patients sometimes present with peripheral lymphocytosis, without lymphadenopathy and systemic symptoms, often mimicking chronic lymphocytic leukemia. This presentation is often associated with an indolent course, with a good prognosis. Such patients are often managed by surveillance alone. Another unusual presentation of MCL is lymphomatous polyposis of the gastrointestinal (GI) tract, with the polyps involving any part of the GI tract and detected incidentally on a colonoscopy.
Current Standards of Diagnosis
A diagnosis of MCL requires a histopathological examination of a lymph node or lymph tissue. A peripheral flow cytometry test and a bone marrow biopsy can also be diagnostic in patients who present with peripheral lymphocytosis.
Historically, MCL was referred to as intermediate lymphocytic lymphoma or centrocytic lymphoma, based on the histologic observation that some of the cells had indented nuclei (as seen in small cleaved-cell lymphoma) and some cells had well-rounded nuclei (similar to small lymphocytic lymphoma). In the 1990s, with a better understanding of the molecular aberrations and the immunophenotype associated with the disease, the term MCL was coined.10 A typical histological appearance, with a distinct immunophenotype and molecular aberrations, is required to make a diagnosis of MCL.
Histologically, neoplastic cells in MCL are small-to medium-sized lymphocytes with scant cytoplasm, clumped chromatin, and inconspicuous nucleoli. The cytological subtypes include classical MCL, blastoid MCL, and pleomorphic MCL.11-13 MCL can exhibit different growth patterns, including diffuse, in situ mantle cell neoplasia; MCL with expanded mantle zones; and nodular MCL. In nodular MCL, nodules consist of follicles with reactive germinal centers surrounded by mantles of neoplastic lymphocytes. This is also referred to as mantle zone pattern. As the disease progresses, there is an obliteration of the interfollicular/nodular pattern, resulting in a diffuse MCL growth pattern. In some cases, referred to as the blastic variant, the neoplastic cells are larger than the nodular variant, and the nuclei have finely dispersed chromatin, with a high mitotic rate. The pleomorphic variant has large cells with irregular nuclear contours and prominent nucleoli; its morphological appearance is like that of diffuse large B-cell lymphoma. The blastic and the pleomorphic variants are associated with a more aggressive clinical course and are frequently associated with more complex cytogenetic findings.
The immunophenotype of MCL is characterized by the expression of B-cell antigens: CD20 positive, CD19 positive, and CD22 positive, with monotypic immunoglobulins.14λ Light chains are more commonly seen than κ light chains. Cells are CD5 positive and have nuclear expression of cyclin D1. The cells are CD10 negative, BCL6 negative, and typically CD23 negative. Cytogenetic assessment for karyotype or fluorescence in situ hybridization showing t(11;14)(q13, q32) is a diagnostic feature and is seen in 90% to 95% of MCL cases. Ki-67 serves as a prognostic marker.
Molecular Mutations Of Significance
The Table shows common MCL molecular aberrations, all of which have been shown to play a role not only in prognostication, but also in predicting responses to conventional therapies.19
Molecular Mutations Detected in MCL, With Roles in Tumorigenesis and Clinical Significance15-23
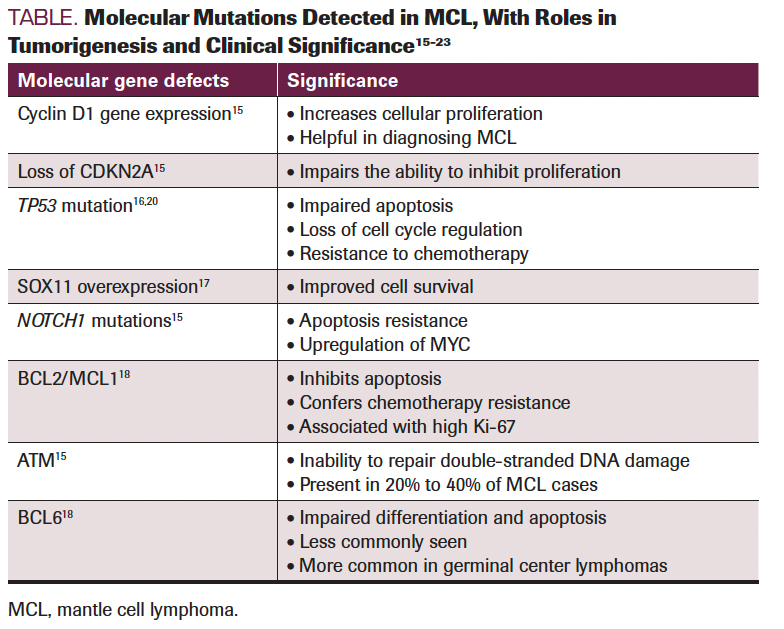
Common Molecular Aberrations in MCL
Cyclin D1 overexpression: Chromosomal translocation t(11:14) (q13;q32) is detected in the majority of MCL cases. This translocation results in the transposition of the cyclin D1 gene, CCND1, on chromosome 11 (11q13) to a site downstream of the immunoglobulin heavy chain gene promoter on chromosome 14 (14q32).20-22 The t(11;14) results in constitutive upregulation and increased cyclin D1 expression. Overexpression of cyclin D1 results in activation of CDK4/6, which in turn promotes the transition of a cell from G1 to the S phase.
CDKN2A deletions: The CDKN2A gene encodes p16, a CDK inhibitor that inhibits CDK4/6. Deletion of CDKN2A results in uncontrolled cell proliferation. Seen in 25% of MCL cases, deletion is associated with aggressive histology.15
TP53 mutations: TP53 is a tumor suppressor gene located at 17p13.1. TP53 mutations or deletions can result in cell cycle upregulation, higher proliferation, and inhibition of apoptosis.TP53 mutations predict an aggressive disease course and poor response to cytotoxic chemotherapy, and they are associated with inferior outcomes.16,23 TP53 mutations appear in approximately 11% of MCL cases, whereas 17p deletions are seen in up to 16% of all MCL cases.22
SOX11 overexpression: SOX11 is a transcription factor encoded by the SOX11 gene located on chromosome 2p25. SOX11 overexpression results in augmented B-cell antigen receptor signaling and activation of PAX-5. In turn, this results in inhibition of differentiation, promotion of angiogenesis, and upregulation of CXCR4, with the consequence of promoting invasiveness of the cells. Certain other mutations such as BIRC3, CARD11, KMT2D, MAP2K 14, and MYC, have also been reported.17,24
Stratification For Treatment Selection
As advances are made in molecular biology, MCL prognostic factors continue to evolve.25 The Mantle Cell Lymphoma International Prognostic Index (MIPI) and a simplified MIPI are commonly used for predicting outcomes.25,26 The simplified MIPI score takes into consideration age, lactate dehydrogenase levels, performance status, and white blood cell count, dividing patients into low-, intermediate-, and high-risk categories,26 for which the 5-year overall survival (OS) rates are 81%, 63%, and 35%, respectively.27 A Ki-67 index greater than 30% is associated with poor prognosis; this has been added to the MIPI risk score for a biologic MIPI score. A higher MIPI score is often an indication of a need for intensive therapy. Aggressive histology, such as blastoid and pleomorphic variants, are associated with poor prognoses.28 Additionally, TP53 mutations, 13q deletion, NOTCH1, CDKN2A deletion, and complex cytogenetics are associated with poor prognoses. Multivariate analysis showed that the patients harboring vs not harboring a TP53 mutation had progression-free survival (PFS) of 1 year vs 12.7 years, respectively. Patients with TP53 mutations do poorly with cytotoxic chemotherapy.23 Absence of SOX11 expression is associated with a favorable prognosis.25
Therapy Selection
Treatment options for a patient with MCL should be tailored based on their functional age, clinical risk factors, and lymphoma biology (Figure).
Current Approach to a Patient With Newly Diagnosed MCL
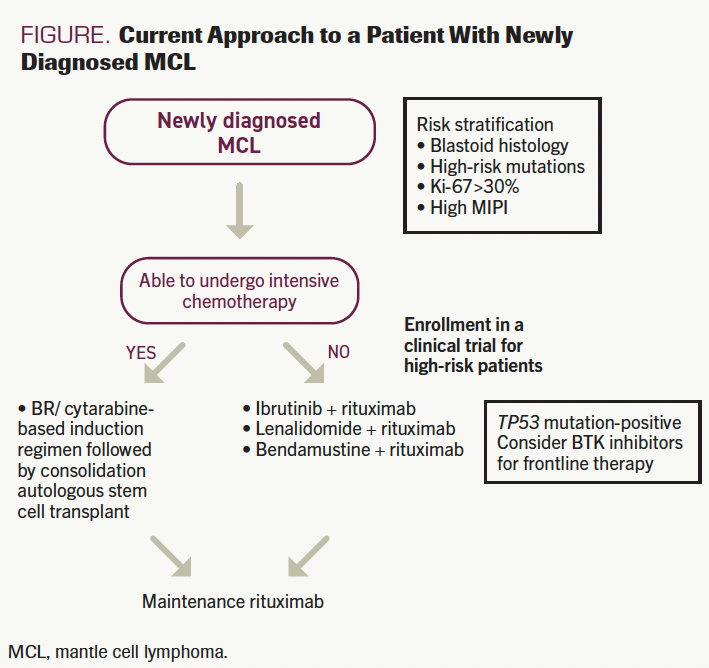
Indolent MCL
Approximately 20% to 30% of patients with MCL have an asymptomatic presentation; they often present with leukocytosis, asymptomatic splenomegaly or low tumor volume, and without bulky lymphadenopathy. These patients often have a low biological MIPI score and can often be observed, without therapy.
Patients who require therapy for MCL are classified into 2 groups: those who can receive intensive chemotherapy and those who are considered unfit to receive intensive chemotherapy and autologous stem cell transplant (ASCT).
Rituximab (R)-based chemoimmunotherapies with or without consolidative ASCT, with maintenance rituximab, is the current standard of care in patients who are physically fit.29 The choice of initial chemotherapy regimens varies widely among various institutions.28 The Nordic regimen treated 160 patients with R-Maxi CHOP (cyclophosphamide 1200 mg/m2, doxorubicin
75mg/m2, vincristine 2 mg, prednisone) and high-dose cytarabine.30 Patients who had a response to chemotherapy underwent ASCT. At a median follow-up of 11.4 years, the overall response rate (ORR) was 96%.
The phase 3 BRIGHT trial (NCT03180840) enrolled 447 patients with indolent lymphomas, including MCL, and compared outcomes between bendamustine and rituximab (BR) for 6 cycles vs R-CHOP (rituximab, cyclophosphamide 750mg/m2, doxorubicin 50mg/m2, vincristine 1.4mg/m2)
for 6 cycles.31 Among the 134 evaluable patients with MCL in this study, the completed response rates were higher in the BR arm when compared with the R-CHOP arm (50% vs 27%, respectively). The median OS at 5 years was 82% with BR vs 85% with R-CHOP. This may reflect subsequent lines of chemotherapy, which included BR for patients in both the R-CHOP and rituximab, cyclophosphamide, vincristine, and prednisolone (R-CVP) arms.
The phase 3 StiL trial (NCT00991211) compared BR with R-CHOP among 514 patients with newly diagnosed indolent lymphomas.32 In this study, 46 patients with MCL received BR and 48 patients with MCL received R-CHOP; BR gave rise to a superior PFS (69.5 months), compared with R-CHOP (PFS, 31 months).32 There was no difference in median OS. BR was associated with lower rates of paresthesias and higher rates of secondary skin malignancies compared with R-CHOP.
The European Mantle Cell Lymphoma Network conducted a large phase 3 study evaluating 497 patients with MCL. Patients were randomly assigned to receive either 6 cycles of R-CHOP or 6 cycles of R-CHOP alternating with rituximab, dexamethasone, cytarabine, and cisplatin (R-DHAP).33 Patients in both arms received consolidative ASCT. Median PFS for patients who received R-CHOP/R-DHAP was 9.1 years vs 4.3 years in the R-CHOP arm, but the difference in OS did not reach statistical significance. There was a significant difference in the OS, favoring the R-CHOP/R-DHAP arm, when adjusted for the MIPI. However, the R-CHOP/R-DHAP arm was associated with higher rates of hematological and renal toxicity, so this regimen is not routinely used, given the toxicity concerns.
Another study combined (rituximab, cyclophosphamide, vincristine, doxorubicin, dexamethasone), alternating with high-dose methotrexate and cytarabine(R-HyperCVAD)34 Ninety-seven patients with MCL received 6 cycles of R-HyperCVAD. Patients did not receive consolidation ASCT. The complete response (CR) rate was 87%. However, the toxicity rates with this regimen were high, with 29% of patients unable to complete therapy due to toxicities. The incidence of grade 3/4 hematological toxicities was 40% to 50%. The incidence of secondary hematological malignancies was 6.4%. Median OS in patients younger than 65 years was 13 years, but median OS among patients older than 65 years was much lower, at 5 years. This regimen, when used in clinical practice, has been associated with a high incidence of hematological toxicity and secondary infections.
At the University of Nebraska Medical Center, we prefer to use BR for induction, due to high response rates and good tolerability. We consider using a cytarabine-based regimen in young patients presenting with high Ki-67 and blastoid variants.
A 2021 study randomly assigned 122 patients with MCL who had achieved a CR or a partial response (PR) to a CHOP-based induction therapy to receive either consolidative ASCT or maintenance therapy with interferon.35 Results showed that 3-year PFS was significantly longer in patients who received ASCT than those in the maintenance arm. Several retrospective studies showed a benefit in PFS and OS with ASCT.36
The 3-arm, randomized, phase 3 TRIANGLE trial (NCT02858258) assigned untreated patients with stage II or higher MCL to induction chemoimmunotherapy and ASCT (arm A); induction chemoimmunotherapy with ibrutinib and ASCT, followed by 2 years of ibrutinib maintenance (arm B); or induction chemoimmunotherapy with 2 years of ibrutinib maintenance alone (arm C). Patients in all 3 arms received maintenance rituximab. The addition of ibrutinib to ASCT showed a superior failure-free survival rate over ASCT alone. At a median follow-up of 31 months, the ibrutinib arm showed a 3-year failure-free survival rate of 88% vs 72% with ASCT alone. The 3-year OS was 86% in arm A, 91% in arm B, and 92% in arm C. The patients in arm A did not have a superior outcome when compared with patients in arm C, raising the question of whether ASCT can be replaced by Bruton tyrosine kinase (BTK) inhibitors. Although further data are necessary—including stratification of patients, as per TP53 mutation status, and blastoid pleomorphic variants—the preliminary data do suggest that the addition of BTK inhibitors to ASCT does improve outcomes.
A phase 3 study, evaluating the role of maintenance rituximab in the post-ASCT setting, enrolled 299 patients younger than 65 years; they were randomly assigned 1:1 to receive rituximab given every other month for 3 years or observation following consolidative ASCT.37 This study showed an improved 4-year PFS (83% vs 64%) and OS (89% vs 80%) with rituximab when compared with the observation arm, respectively. Based on these studies, induction chemotherapy followed by consolidation with ASCT and maintenance rituximab has become the current standard of care in patients who are physically fit.38 For patients who are older and physically unfit, BR followed by maintenance rituximab is the preferred treatment approach. Certain non–chemotherapy-based approaches, such as lenalidomide/rituximab and ibrutinib/rituximab, have also been used with good response rates.
Novel Treatment Strategies of MCL
Improvement in understanding MCL’s molecular pathogenesis has led to the development of several targeted agents that are currently being used in relapsed/refractory disease and are being studied in the first-line setting. These include BTK inhibitors, BCL-2 inhibitors, immunomodulatory drugs (IMiDs), proteasome inhibitors, mTOR inhibitors, and
PI3K inhibitors.
BTK Inhibitors
Ibrutinib, acalabrutinib, and zanubrutinib are currently approved in the United States for patients with relapsed MCL.
Ibrutinib, an irreversible BTK inhibitor, demonstrated a CR rate of 58% in patients with relapsed MCL when used in combination with rituximab.39 At a 4-year follow-up, median PFS was 43 months and median OS was not reached. Grade 3 or higher adverse events (AEs) included neutropenia (16%), thrombocytopenia (11%), atrial fibrillation (6%), and bleeding (5%). Several studies have explored the use of ibrutinib in combination with other novel agents, with promising results. The phase 2 PHILEMON study (NCT02460276) evaluated the combination of ibrutinib, rituximab, and lenalidomide in 50 patients with relapsed/refractory MCL and reported an ORR of 76% at a median follow-up of 40 months.40 Ibrutinib has also been used in combination with venetoclax in patients with relapsed disease, with promising results. In the phase 2 AIM study (NCT02471391), 23 patients with relapsed disease (less than 2 lines of therapy) received venetoclax plus ibrutinib, resulting in an ORR of 72% and a CR rate of 62%.41 Notably, 50% of the patients had a TP53 mutation and 75% had a high MIPI score, which are disease features that are usually associated with poor prognoses. Ibrutinib has also been combined with venetoclax and obinutuzumab, with a 2-year PFS of 69.5%.42
Acalabrutinib, a second-generation irreversible BTK inhibitor, has better selectivity and minimal off-target effects (due to fewer cardiovascular complications) when compared with ibrutinib. The phase 2 ACE-LY-004 study (NCT02213926) enrolled 124 patients with relapsed/refractory disease (more than 2 lines of therapy) and reported an ORR of 81% and a CR rate of 48% with acalabrutinib. The incidence of atrial fibrillation (2.4%) was significantly lower when compared with ibrutinib.43 The responses were consistent in high-risk groups as well.
Zanubrutinib is also a selective, irreversible BTK inhibitor, with studies demonstrating an ORR of 84% and a CR rate of 68% in patients with relapsed/refractory MCL (more than 2 prior lines of therapy).44 Incidence of atrial fibrillation (0.89%) with zanubrutinib was lower than with acalabrutinib and ibrutinib.
Pirtobrutinib, a reversible BTK inhibitor, has shown activity in patients who are refractory to irreversible BTK inhibitors. In the phase 1/2 BRUIN trial (NCT03740529), 134 patients with relapsed/refractory disease—90% of whom were exposed to a prior BTK inhibitor—received pirtobrutinib.45 The ORR was 51% and the CR rate was 25% in patients who were previously exposed to a BTK inhibitor. In patients who were BTK naïve, the ORR was 82% and the CR rate was 18%. Incidence of atrial fibrillation and bleeding was less than 2%, making this a promising therapy in patients with MCL.45
BTK inhibitors are being increasingly explored as frontline therapy, with promising results. A phase 2 study evaluated ibrutinib plus rituximab as first-line therapy in older patients and reported an ORR of 96%. The phase 2 OASIS-II study (NCT04802590) evaluated ibrutinib, venetoclax, and obinutuzumab in relapsed and treatment-naïve patients.42 In this study, 15 patients were treatment naïve and their ORR was 86%, with 73% attaining undetectable minimal residual disease (MRD).42 The combination of acalabrutinib with venetoclax has also been studied, with early-phase trials showing good safety and efficacy. The phase 3 SHINE study (NCT01776840) randomly assigned 523 patients who were treatment naïve and older than 65 years to receive ibrutinib, bendamustine, and rituximab or BR.46 Patients who responded to therapy were given maintenance rituximab for 2 years; ibrutinib was continued until disease progression. At a median follow-up of 7 years, PFS was superior in the ibrutinib arm compared with the chemotherapy-only arm (80 vs 5.2 months). However, there was no difference in OS. Although there was a lower incidence of death due to progressive disease in the ibrutinib arm compared with the chemotherapy arm (11% vs 21%, respectively), there was a higher incidence of death due to AEs (11% vs 6%). Subgroup analysis did not show a statistically significant improvement in outcomes in the patients with high-risk disease and TP53 mutations with the ibrutinib-based regimen, suggesting that ibrutinib may not entirely overcome the poor prognostic significance of TP53 mutations.
In a phase 1 study, 12 patients received acalabrutinib, rituximab, and bendamustine for 3 cycles, followed by acalabrutinib, rituximab, and cytarabine for 3 cycles.47 Patients who responded to therapy underwent stem cell collection for ASCT. The ORR with this regimen was 85%. Based on these results, a larger phase 2 study, EA4181 (NCT04115631), is currently enrolling patients to evaluate MRD rates and ORRs.
BCL-2 Inhibitors
Venetoclax is a selective, oral BCL-2 inhibitor that has shown to be active in MCL. In a phase 1 study of 28 BTK inhibitor–naïve patients with relapsed/refractory MCL, single-agent venetoclax resulted in an ORR of 75% and a median PFS of 14 months.48 The ORR was 50% in patients who were BTK refractory. In clinical practice, venetoclax is being used as a single agent in BTK-refractory settings. Venetoclax has synergistic activity with BTK inhibitors; combination therapies show impressive response rates in high-risk disease, particularly in patients with TP53 mutations.49 Combination therapy is being actively investigated in combination in the frontline and relapsed settings.
Immunomodulatory Agents
Lenalidomide, a second-generation IMiD, has shown efficacy in MCL. In the single-arm phase 2 MCL-001 study (NCT00737529), single-agent lenalidomide showed an ORR of 28% and a duration of response of 16.6 months in patients with relapsed/refractory MCL.49 A phase 1/2 study evaluating a rituximab/lenalidomide combination showed an ORR of 57%, with a PFS of 11 months and an OS of 24 months.50 Retrospective studies showed poor outcomes with rituximab/lenalidomide in patients who are BTK refractory, so this combination is not preferred in post-BTK relapse settings. This regimen is reserved for patients who are unable to tolerate or have a contraindication to BTK inhibitors. Lenalidomide has been combined with BTK inhibitors and BCL-2 inhibitors, with ORRs ranging from 50% to 56%.
Risk-Adapted Approach
Given the heterogeneity in MCL’s disease biology, several studies are being designed using a risk-stratified approach.19 Given the poor outcomes of chemotherapy for patients with high-risk mutations, it is advisable to enroll such patients in clinical trials. In the phase 2 WINDOW II study (NCT03710772), patients were risk stratified as low-risk (Ki-67 less than 30%, low MIPI, lacking high-risk mutations, tumors smaller than 3 cm) and high-risk (Ki-67 of more than 30%, TP53, NSD2, NOTCH mutations, complex karyotype or 17p deletion, MYC positivity, blastoid/pleomorphic histology, partial response to induction).51 All patients received ibrutinib, rituximab, and venetoclax as an induction regimen. Following induction, patients who were low risk were observed, and patients who were high risk received R-HyperCVAD alternating with methotrexate/cytarabine. The ORR with this regimen was 96%.
The phase 2 BOVEN study (NCT03824483) is evaluating zanubrutinib, obinutuzumab, and venetoclax in patients with TP53 mutations.52 This study incorporates MRD and response-guided treatment duration. Patients received zanubrutinib plus venetoclax for a minimum of 2 years and, based on MRD undetectable status and response, were placed on surveillance. The study is ongoing, but the initial results show an ORR of 86%.
CAR T-Cell Therapy
Brexucabtagene autoleucel (KTE-X19), an anti-CD19 autologous chimeric antigen receptor (CAR) T-cell product, is FDA approved for the treatment of relapsed/refractory MCL.53 In the pivotal phase 2 ZUMA-2 study (NCT02601313), 68 patients with relapsed/refractory MCL were treated with lymphodepleting chemotherapy, followed by a single infusion of KTE-X19. All patients had disease progression on BTK inhibitors and had received 3 or more prior lines of therapy. At a median follow-up of 12 months, the ORR was 93%, with a CR rate of 67%. At 6 months, 79% were MRD negative.53 What is notable is that although the ORR was more than 90% in patients with TP53 mutations, it was less than 50% in those with Ki-67and 80% in patients with blastoid histology. The incidence of grade 3 or higher cytokine release syndrome (CRS) was 15% and neurotoxicity was 31%.
Lisocabtagene maraleucel, an anti-CD19 CAR T-cell product, is also being evaluated in MCL. The phase 1 MCL-TRANSCEND- NHL-001 study (NCT02631044) enrolled 32 patients with relapsed/refractory MCL (2 or more prior lines of therapy).54 At a median follow-up of 6 months, the ORR was 84%, with a CR rate of 59%. As with KTE-X19, efficacy was noted in patients with high-risk features.
Promising Therapies
Bispecific Antibodies
Bispecific T-cell engagers (BiTEs) are agents that can engage CD3 and redirect T cells against B cells that express specific antigens, such as CD20 and CD19. Glofitamab is an intravenously administered CD20 × CD3 BiTE, engineered with a 2:1 configuration of CD20:CD3.55 Updated subgroup analysis of this study showed that 29 patients with MCL had an ORR of 83%.56 It was well tolerated, with grade 3 or higher CRS and infections occurring in 14% and 13% of the patients, respectively. No grade 3 or higher neurotoxicity was reported.
Epcoritamab is a subcutaneously administered CD20 × CD3 BiTE, with initial studies showing an ORR of 50% in patients with MCL.57
Antibody-Drug Conjugates
Zilovertamab vedotin is an antibody-drug conjugate that binds specifically to the ROR1, which is an oncoprotein that is expressed in MCL and other B-cell malignancies.58 The preliminary data report promising safety and efficacy in heavily pretreated patients with MCL, with an ORR of 47%. The commonly observed AEs were peripheral neuropathy and neutropenia.
Conclusions
Advances made in MCL have improved patient outcomes significantly. The current standard of care for transplant-eligible patients includes high-dose chemoimmunotherapy with a cytarabine-based regimen, followed by ASCT. Patients with high-risk molecular mutations, such as TP53 mutations, continue to do poorly despite conventional treatment approaches, which puts the role of conventional chemotherapy in such patients into question. Studies incorporating BTK inhibitors have shown superior outcomes in patients with high-risk mutations when compared with conventional chemoimmunotherapy. With several novel agents being developed for this disease, there is a need to better risk stratify, identify high-risk mutations, and tailor treatments accordingly. Studies are ongoing, evaluating the role of MRD; it is also being used as a tool to guide therapies and is likely to be incorporated in clinical settings. BiTE antibodies, anti-ROR1 antibodies, and next-generation CAR T cells are promising. Many more potential new molecules that are in clinical trials could eventually be incorporated into the current treatment landscape. With the rapid advances being made in the field of MCL, the future looks promising.
Author Affiliations
1Division of Oncology, Department of Medicine,
University of Nebraska Medical Center,
Fred and Pamela Buffet Cancer center,
Omaha, NE 68198
Corresponding Author
Avyakta Kallam MBBS
Assistant Professor,
Division of Oncology,
Department of Medicine,
University of Nebraska Medical Center,
986840 Nebraska Medical Center,
Omaha, NE 68198
Emails : avyaktakallam@gmail.com; jmvose@unmc.edu
References
- Wang Y, Ma S. Risk factors for etiology and prognosis of mantle cell lymphoma. Expert Rev Hematol. 2014;7(2):233-243. doi:10.1586/17474086.2014.889561.
- Smedby KE, Hjalgrim H. Epidemiology and etiology of mantle cell lymphoma and other non-Hodgkin lymphoma subtypes. Semin Cancer Biol. 2011;21(5):293-298. doi:10.1016/j.semcancer.2011.09.010
- Shah BD, Martin P, Sotomayor EM. Mantle cell lymphoma: a clinically heterogeneous disease in need of tailored approaches. Cancer Control. 2012;19(3):227-235. doi:10.1177/107327481201900307
- Di M, Cui C, Kothari SK, et al. Survival of mantle cell lymphoma in the era of Bruton tyrosine kinase inhibitors: a population-based analysis. Blood Adv. 2022;6(11):3339-3342. doi:10.1182/bloodadvances.2021006934
- Keating SJ, Rege S, McBride A, Shah R, Qian J, Chirikov V. Real-world treatment (tx) patterns, cost, and overall survival (OS) by the line of therapy among patients (pt) with mantle cell lymphoma (MCL): a SEER-Medicare (SM) analysis. J Clin Oncol. 2022;40(28 Suppl):abstr 19. doi:10.1200/JCO.2022.40.28_suppl.019
- Zain J, Bhagat G. Mantle cell lymphoma. In: Armitage JO, Mauch PM, Harris NL, Coiffier B, Dalla-Favera R, eds. Non-Hodgkin Lymphomas. 2nd ed. Wolters Kluwer; 2010:284.
- Berger F, Felman P, Sonet A, et al. Nonfollicular small B-cell lymphomas: a heterogeneous group of patients with distinct clinical features and outcome. Blood. 1994;83(10):2829-2835.
- Majlis A, Pugh WC, Rodriguez MA, Benedict WF, Cabanillas F. Mantle cell lymphoma: correlation of clinical outcome and biologic features with three histologic variants. J Clin Oncol. 1997;15(4):1664-1671. doi:10.1200/JCO.1997.15.4.1664
- Bosch F, López‐Guillermo A, Campo E, et al. Mantle cell lymphoma: presenting features, response to therapy, and prognostic factors. Cancer. 1998;82(3):567-575. doi:10.1002/(sici)1097-0142(19980201)82:3<567::aid-cncr20>3.0.co;2-z
- Weisenburger DD, Armitage JO. Mantle cell lymphoma – an entity comes of age. Blood. 1996;87(11):4483-4494.
- Duggan MJ, Weisenburger DD, Ye YL, et al. Mantle zone lymphoma. a clinicopathologic study of 22 cases. Cancer. 1990;66(3):522-529. doi:10.1002/1097-0142(19900801)66:3<522::aid-cncr2820660320>3.0.co;2-4
- Weisenburger DD, Kim H, Rappaport H. Mantle‐zone lymphoma: a follicular variant of intermediate lymphocytic lymphoma. Cancer. 1982;49(7):1429-1438. doi:10.1002/1097-0142(19820401)49:7<1429::aid-cncr2820490720>3.0.co;2-5
- Weisenburger DD, Vose JM, Greiner TC, et al. Mantle cell lymphoma. a clinicopathologic study of 68 cases from the Nebraska Lymphoma Study Group. Am J Hematol. 2000;64(3):190-196. doi:10.1002/1096-8652(200007)64:3<190::aid-ajh9>3.0.co;2-b
- Barista I, Romaguera JE, Cabanillas F. Mantle-cell lymphoma. Lancet Oncol. 2001;2(3):141-148. doi:10.1016/S1470-2045(00)00255-2. Published corrections appear in Lancet Oncol. 2001;2(4):198 and 2002;3(7):396.
- Obrador-Hevia A, Fernández de Mattos S, Villalonga P, Rodríguez J. Molecular biology of mantle cell lymphoma: from profiling studies to new therapeutic strategies. Blood Rev. 2009;23(5):205-216. doi:10.1016/j.blre.2009.03.001
- Aukema SM, Hoster E, Rosenwald A, et al. Expression of TP53 is associated with the outcome of MCL independent of MIPI and Ki-67 in trials of the European MCL network. Blood. 2018;131(4):417-420. doi:10.1182/blood-2017-07-797019
- Mozos A, Royo C, Hartmann E, et al. SOX11 expression is highly specific for mantle cell lymphoma and identifies the cyclin D1-negative subtype. Haematologica. 2009;94(11):1555-1562. doi:10.3324/haematol.2009.010264. Published correction appears in Haematologica. 2010;95(9):1620.
- Hartmann EM, Campo E, Wright G, et al. Pathway discovery in mantle cell lymphoma by integrated analysis of high-resolution gene expression and copy number profiling. Blood. 2010;116(6):953-961. doi:10.1182/blood-2010-01-263806
- Kumar A, Eyre TA, Lewis KL, Thompson MC, Cheah CY. New directions for mantle cell lymphoma in 2022. Am Soc Clin Oncol Educ Book. 2022;42:1-15. doi:10.1200/EDBK_349509
- Halldórsdóttir AM, Lundin A, Murray F, et al. Impact of TP53 mutation and 17p deletion in mantle cell lymphoma. Leukemia. 2011;25(12):1904-1908.doi:10.1038/leu.2011.162
- Vandenberghe E, De Wolf‐Peeters C, van den Oord J, et al. Translocation (11;14): a cytogenetic anomaly associated with B‐cell lymphomas of non‐follicle centre cell lineage. J Pathol. 1991;163(1):13-18. doi:10.1002/path.1711630104
- Tsujimoto Y, Yunis J, Onorato-Showe L, Erikson J, Nowell PC, Croce CM. Molecular cloning of the chromosomal breakpoint of B-cell lymphomas and leukemias with the t(11;14) chromosome translocation. Science. 1984;224(4656):1403-1406. doi:10.1126/science.6610211
- Eskelund CW, Dahl C, Hansen JW, et al. TP53 mutations identify younger mantle cell lymphoma patients who do not benefit from intensive chemoimmunotherapy. Blood. 2017;130(17):1903-1910. doi:10.1182/blood-2017-04-779736
- Ek S, Dictor M, Jerkeman M, Jirström K, Borrebaeck CAK. Nuclear expression of the non B-cell lineage Sox11 transcription factor identifies mantle cell lymphoma. Blood. 2008;111(2):800-805. doi:10.1182/blood-2007-06-093401
- Silkenstedt E, Linton K, Dreyling M. Mantle cell lymphoma – advances in molecular biology, prognostication and treatment approaches. Br J Haematol. 2021;195(2):162-173. doi:10.1111/bjh.17419
- Hoster E, Dreyling M, Klapper W, et al; German Low Grade Lymphoma Study Group (GLSG); European Mantle Cell Lymphoma Network. A new prognostic index (MIPI) for patients with advanced-stage mantle cell lymphoma. Blood. 2008;111(2):558-565. doi:10.1182/blood-2007-06-095331
- Hoster E, Klapper W, Hermine O, et al. Confirmation of the mantle-cell lymphoma International Prognostic Index in randomized trials of the European Mantle-Cell Lymphoma Network. J Clin Oncol. 2014;32(13):1338-1346. doi:10.1200/JCO.2013.52.2466
- Maddocks K. Update on mantle cell lymphoma. Blood. 2018;132(16):1647-1656. doi:10.1182/blood-2018-03-791392
- Geisler CH, Kolstad A, Laurell A, et al; Nordic Lymphoma Group. Long-term progression-free survival of mantle cell lymphoma after intensive front-line immunochemotherapy with in vivo–purged stem cell rescue: a nonrandomized phase 2 multicenter study by the Nordic Lymphoma Group. Blood. 2008;112(7):2687-2693. doi:10.1182/blood-2008-03-147025
- Geisler CH, Kolstad A, Laurell A, et al. Long-term progression-free survival of mantle cell lymphoma after intensive front-line immunochemotherapy with in vivo–purged stem cell rescue: a nonrandomized phase 2 multicenter study by the nordic lymphoma group. Blood. 2008;112(7):2687-2693.
- Flinn IW, van der Jagt R, Kahl BS, et al. Randomized trial of bendamustine-rituximab or R-CHOP/R-CVP in first-line treatment of indolent NHL or MCL: the BRIGHT study. Blood. 2014;123(19):2944-2952. doi:10.1182/blood-2013-11-531327
- Rummel MJ, Niederle N, Maschmeyer G, et al; Study group indolent Lymphomas (StiL). Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: an open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet. 2013;381(9873):1203-1210. doi:10.1016/S0140-6736(12)61763-2. Published correction appears in Lancet. 2013;381(9873):1184.
- Hermine O, Hoster E, Walewski J, et al; European Mantle Cell Lymphoma Network. Addition of high-dose cytarabine to immunochemotherapy before autologous stem-cell transplantation in patients aged 65 years or younger with mantle cell lymphoma (MCL Younger): a randomised, open-label, phase 3 trial of the European Mantle Cell Lymphoma Network. Lancet. 2016;388(10044):565-575. doi:10.1016/S0140-6736(16)00739-X
- Chihara D, Cheah CY, Westin JR, et al. Rituximab plus hyper‐CVAD alternating with MTX/Ara‐C in patients with newly diagnosed mantle cell lymphoma: 15‐year follow‐up of a phase II study from the MD Anderson Cancer Center. Br J Haematol. 2016;172(1):80-88. doi:10.1111/bjh.13796
- Dreyling M, Lenz G, Hoster E, et al. Early consolidation by myeloablative radiochemotherapy followed by autologous stem cell transplantation in first remission significantly prolongs progression-free survival in mantle-cell lymphoma: results of a prospective randomized trial of the European MCL Network. Blood. 2005;105(7):2677-2684. doi:10.1182/blood-2004-10-3883
- Riedell PA, Hamadani M, Ahn KW, et al. Effect of time to relapse on overall survival in patients with mantle cell lymphoma following autologous haematopoietic cell transplantation. Br J Haematol. 2021;195(5):757-763. doi:10.1111/bjh.17865
- Le Gouill S, Thieblemont C, Oberic L, et al; LYSA Group. Rituximab after autologous stem-cell transplantation in mantle-cell lymphoma. N Engl J Med. 2017;377(13):1250-1260. doi:10.1056/NEJMoa1701769
- Hilal T, Wang Z, Almader‐Douglas D, Rosenthal A, Reeder CB, Jain T. Rituximab maintenance therapy for mantle cell lymphoma: a systematic review and meta‐analysis. Am J Hematol. 2018;93(10):1220-1226. doi:10.1002/ajh.25226
- Wang, M. L., Hagemeister, F., Westin, J. R., Fayad, L., Samaniego, F., Turturro, F., ... & Romaguera, J. E. (2014). Ibrutinib and rituximab are an efficacious and safe combination in relapsed mantle cell lymphoma: preliminary results from a phase II clinical trial. Blood, 124(21), 627.
- Jerkeman M, Winther Eskelund C, Hutchings M, et al. Ibrutinib, lenalidomide, and rituximab in relapsed or refractory mantle cell lymphoma (PHILEMON): a multicentre, open-label, single-arm, phase 2 trial. Lancet Haematol. 2018;5(3):e109-e116. doi:10.1016/S2352-3026(18)30018-8
- Tam, Constantine Si Lun, Andrew Warwick Roberts, Mary Ann Anderson, Sarah-Jane Dawson, Rodney J. Hicks, Christiane Pott, David A. Westerman et al. "The combination of ibrutinib and venetoclax (ABT-199) to achieve complete remissions in patients with relapsed/refractory mantle cell lymphoma: Preliminary results of the phase II AIM study." (2016): 7548-7548.
- Le Gouill, Steven, Franck Morschhauser, David Chiron, Krimo Bouabdallah, Guillaume Cartron, Olivier Casasnovas, Caroline Bodet-Milin et al. "Ibrutinib, obinutuzumab, and venetoclax in relapsed and untreated patients with mantle cell lymphoma: a phase 1/2 trial." Blood, The Journal of the American Society of Hematology 137, no. 7 (2021): 877-887.
- Wang M, Rule S, Zinzani PL, et al. Acalabrutinib in relapsed or refractory mantle cell lymphoma (ACE-LY-004): a single-arm, multicentre, phase 2 trial. Lancet. 2018;391(10121):659-667. doi:10.1016/S0140-6736(17)33108-2
- Song Y, Zhou K, Zou D, et al. Treatment of patients with relapsed or refractory mantle-cell lymphoma with zanubrutinib, a selective inhibitor of Bruton's tyrosine kinase. Clin Cancer Res. 2020;26(16):4216-4224. doi:10.1158/1078-0432.CCR-19-3703
- Mato AR, Shah NN, Jurczak W, et al. Pirtobrutinib in relapsed or refractory B-cell malignancies (BRUIN): a phase 1/2 study. Lancet. 2021;397(10277):892-901. doi:10.1016/S0140-6736(21)00224-5
- Wang ML, Jurczak W, Jerkeman M, et al; SHINE Investigators. Ibrutinib plus bendamustine and rituximab in untreated mantle-cell lymphoma. N Engl J Med. 2022;386(26):2482-2494. doi:10.1056/NEJMoa2201817
- Guy D, Watkins M, Wan F, et al. A pilot study of acalabrutinib with bendamustine/rituximab followed by cytarabine/rituximab (R-ABC) for untreated mantle cell lymphoma. Blood. 2020;136(Suppl 1):8-9. doi:10.1182/blood-2020-143095
- Eyre TA, Walter HS, Iyengar S, et al. Efficacy of venetoclax monotherapy in patients with relapsed, refractory mantle cell lymphoma after Bruton tyrosine kinase inhibitor therapy. Haematologica. 2019;104(2):e68-e71. doi:10.3324/haematol.2018.198812
- Goy A, Sinha R, Williams ME, et al. Single-agent lenalidomide in patients with mantle-cell lymphoma who relapsed or progressed after or were refractory to bortezomib: phase II MCL-001 (EMERGE) study. J Clin Oncol. 2013;31(29):3688-3695. doi:10.1200/JCO.2013.49.2835
- Ruan J, Martin P, Shah B, et al. Lenalidomide plus rituximab as initial treatment for mantle-cell lymphoma. N Engl J Med. 2015;373(19):1835-1844. doi:10.1056/NEJMoa1505237
- Wang M, Jain P, Lee HJ, et al. Ibrutinib plus rituximab and venetoclax (IRV) followed by risk-stratified observation or short course R-hyperCVAD/MTX in young patients with previously untreated mantle cell lymphoma – phase-II WINDOW-2 clinical trial. Blood. 2021;138(Suppl 1):abstr 3525. doi:10.1182/blood-2021-153390
- Kumar A, Soumerai JD, Abramson JS, et al. Preliminary safety and efficacy from a multicenter, investigator-initiated phase II study in untreated TP53 mutant mantle cell lymphoma with zanubrutinib, obinutuzumab, and venetoclax (BOVen). Blood. 2021;138(Suppl 1):abstr 3540. doi:10.1182/blood-2021-151831
- Wang M, Munoz J, Goy A, et al. KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2020;382(14):1331-1342. doi:10.1056/NEJMoa1914347
- Sheikh S, Migliorini D, Lang N. CAR T-based therapies in lymphoma: a review of current practice and perspectives. Biomedicines. 2022;10(8):1960. doi:10.3390/biomedicines10081960
- Hutchings M, Morschhauser F, Iacoboni G, et al. Glofitamab, a novel, bivalent CD20-targeting T-cell–engaging bispecific antibody, induces durable complete remissions in relapsed or refractory B-cell lymphoma: a phase I trial. J Clin Oncol. 2021;39(18):1959-1970. doi:10.1200/JCO.20.03175
- Phillips TJ, Forero-Torres A, Sher T, et al. Interim analysis of a phase I study of INCB040093, a PI3Kδ inhibitor, alone or in combination with INCB039110, a selective JAK1 inhibitor, in patients (pts) with relapsed or refractory (r/r) B-cell malignancies. J Clin Oncol. 2015;33(Suppl 15):abstr 8520. doi:10.1200/jco.2015.33.15_suppl.8520
- Roost Clausen M, Lugtenburg P, Hutchings M, et al. Subcutaneous epcoritamab in patients with relapsed/refractory B-cell non-Hodgkin lymphoma: safety profile and antitumor activity. J Clin Oncol. 2021;39(Suppl 15):abstr 7518. doi:10.1200/JCO.2021.39.15_suppl.7518
- Wang ML, Barrientos JC, Furman RR, et al. Zilovertamab vedotin targeting of ROR1 as therapy for lymphoid cancers. NEJM Evidence. 2022;1(1):EVIDoa2100001. doi:10.1056/EVIDoa2100001
Highlighting Insights From the Marginal Zone Lymphoma Workshop
Clinicians outline the significance of the MZL Workshop, where a gathering of international experts in the field discussed updates in the disease state.