Cutaneous T-Cell Lymphoma: Current and Emerging Therapies
Julia Dai, MD, and Madeleine Duvic, MD, present a comprehensive review of the current state of research and treatment in cutaneous T-cell lymphoma.
ABSTRACT
Cutaneous T-cell lymphomas (CTCLs) are clinically heterogeneous T-cell lymphomas that arise in the skin and are characterized by their clinical and pathological features. This review will focus on mycosis fungoides (MF) and Sézary syndrome (SS), which represent 60% to 80% and less than 10% of CTCL cases, respectively. While most patients with MF present with patches and plaques and can be successfully treated with skin-directed therapies, a minority of patients progress from early to advanced stages or undergo large cell transformation. SS is defined as erythroderma, lymphadenopathy, and more than 1000 circulating atypical T-cells/uL with cerebriform nuclei. It has a poor overall survival of 2.5 years. Given the overall rarity of CTCLs, it is notable that clinical trials of treatments for MF/SS have been successfully completed, resulting in FDA approvals of novel therapies with increasing overall response rates. This review outlines the current multidisciplinary approach to diagnosing and treating MF/SS, with a focus on combining skin-directed therapies with emerging targeted and investigational systemic therapies. Integrating these anticancer therapies with skin care and bacterial decolonization is critical for comprehensive management. Curing patients with MF/SS may be possible by using a personalized medicine approach including novel combination strategies, restoration of T helper 1 cytokines, and avoidance of immunosuppressive regimens.
Oncology (Williston Park). 2023;37(2):55-62.
DOI: 10.46883/2023.25920984
Introduction
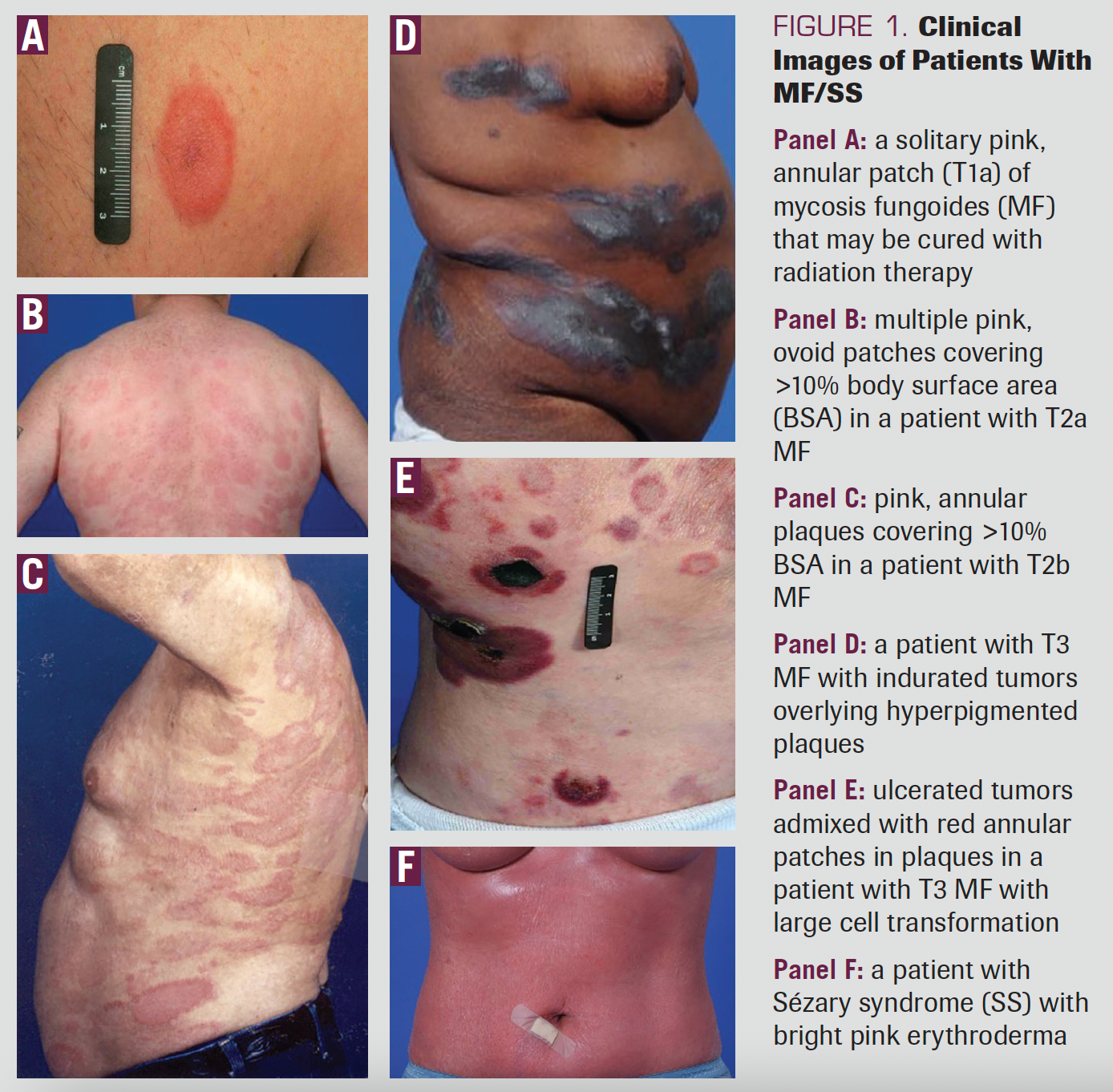
Cutaneous T-cell lymphoma (CTCL) describes a group of clinically heterogeneous T-cell lymphomas that arise in the skin.1 Mycosis fungoides (MF), the most common CTCL, represents 60% to 80% of all CTCLs whereas Sézary syndrome (SS), the erythrodermic and leukemic variant, affects fewer than 10% of patients with CTCL. Most patients with MF present with stage IA disease, defined as patches and plaques involving less than 10% of the body surface area (Figure 1). For most individuals diagnosed with early-stage disease, this is a chronic skin affliction managed with skin-directed therapy (SDT) with acceptable disease control and possible complete remissions. If the disease progresses, the treatment of MF/SS consists of sequential therapies that have increasing toxicity and potential immunosuppression.
When the first randomized study of patients with CTCL was conducted at the National Institutes of Health in 1989, no survival advantage was seen with electron beam radiation therapy (EBT) combined with chemotherapy compared with less aggressive sequential topical therapies.2 Thus, the oncologist should be aware of the full toolbox of possible non-immunosuppressive treatments, especially skin-directed therapies and immunotherapies that can prolong the lifespan of patients with MF or SS.
FIGURE 1. Clinical Images of Patients With MF/SS
Skin-Directed Therapies
SDTs are the mainstay for treatment of early-stage disease, but they also have an important role in disease palliation in patients with advanced disease. Because MF/SS is a chronic skin disease that likely requires treatment for many years, management should start out as conservatively as possible, with the goals of putting the disease in a prolonged or permanent remission and controlling pruritus.
Topical steroids
We use high-potency topical clobetasol 0.05% twice daily as a first-line SDT. If lesions resolve, the frequency or potency should be slowly tapered. Tapering is desirable because steroids decrease collagen production; this leads to skin atrophy, which can be severe in intertriginous areas and on the face and neck.
For patients with extensive skin involvement or erythroderma, application of topical triamcinolone 0.1% with wet warm towels for 15 minutes (wet wraps) can be helpful for controlling the itching and skin lesions for a limited period.
Topical nitrogen mustard
Topical nitrogen mustard (NM) has been used off label as a frontline SDT in MF for decades. In 2013, mechlorethamine 0.016% gel (Valchlor gel) was approved by the FDA for use in MF.3 NM may be used as salvage therapy for patients who failed topical steroids or as a maintenance therapy following EBT. The most common adverse effect (AE) seen with NM is contact dermatitis, which is thought to elicit an inflammatory response that may lead to earlier disease clearance. Topical steroids have been used in conjunction with NM but may limit the contact dermatitis.
Topical retinoids
Vitamin A is a lipid-soluble, essential nutrient that dimerizes and binds to retinoid receptors. Its action depends on the type of retinoid: With retinoic acid receptors (RARs), it can induce T-cell or keratinocyte differentiation, and with retinoid X receptors (RXRs), it can induce apoptosis of tumor cells. Topical bexarotene (Targretin gel) is an RXR retinoid approved for the treatment of MF based on phase 1 and 2 trials.4 The RAR retinoid tazarotene is approved for acne and psoriasis and demonstrates efficacy similar to that of bexarotene in patients with MF. Topical retinoids are especially helpful for hypertrophic, psoriatic, acral, or follicular lesions. Retinoids will cause irritation in intertriginous areas and should be used sparingly in these regions.
Topical immunotherapy
Imiquimod 5% cream (Aldara) is a Toll-like receptor (TLR)-7 agonist approved for treatment of genital warts. Several case reports observed that imiquimod 5% cream twice daily is effective in treating tumors in MF. Topical resiquimod is a more potent TLR-7 and TLR-8 agonist and demonstrated efficacy in patients with MF in a phase 1 trial.5 Both imiquimod and resiquimod may cause irritation and may have an abscopal effect, possibly through the generation of γ-interferon, interleukin (IL)-12, and natural killer (NK) cells.
Two steroid-sparing topical calcineurin agents (pimecrolimus and tacrolimus) have been used off label to treat areas at risk for atrophy, such as eyelids or genitalia. In a phase 2 trial evaluating topical pimecrolimus 1% cream twice daily for 16 weeks in early-stage MF, response rates of 54% and 73% were seen in patients with stage IA and IB disease, respectively.6
Phototherapy
Phototherapy with narrowband ultraviolet B (nbUVB) or psoralen plus ultraviolet A (PUVA) are often the first therapies considered after topical therapies have failed.7 PUVA is a combination of oral psoralen, a photosensitizing agent, followed by UVA exposure. PUVA is more effective than nbUVB for treating more extensive plaque disease. Choice of phototherapy depends on the patient’s clinical phenotype and access to phototherapy centers. Phototherapy may be used alone or combined with topical steroids as well as topical/oral retinoids; however, adjunctive treatment with NM is not recommended.
Photodynamic therapy
Photodynamic therapy is a novel treatment that combines fluorescent light and a topical photochemical (eg, hypericin) applied prior to light exposure. A phase 2 trial demonstrated safety and efficacy of topical hypericin to individual lesions followed by visible light exposure.8 A phase 3 study of hypericin ointment with photodynamic therapy demonstrated an index lesion response rate (defined as 50% or greater improvement) in 49% of lesions after 3 cycles of therapy.9
Electron beam radiation (EBT) therapy
Treatment with EBT has the highest response rates, greater than 90%. Complete response rates are highest in patients with T1 and T2 disease, and early use of low-dose radiation to a solitary lesion may be curative. Low-dose (12 Gy) total skin EBT (TSEBT) can be used for disease control and palliation of symptoms in patients with disseminated skin disease,10 whereas higher doses (up to 36 Gy) are recommended to debulk skin compartment disease prior to allogeneic hematopoietic stem cell transplantation (alloHSCT).11,12
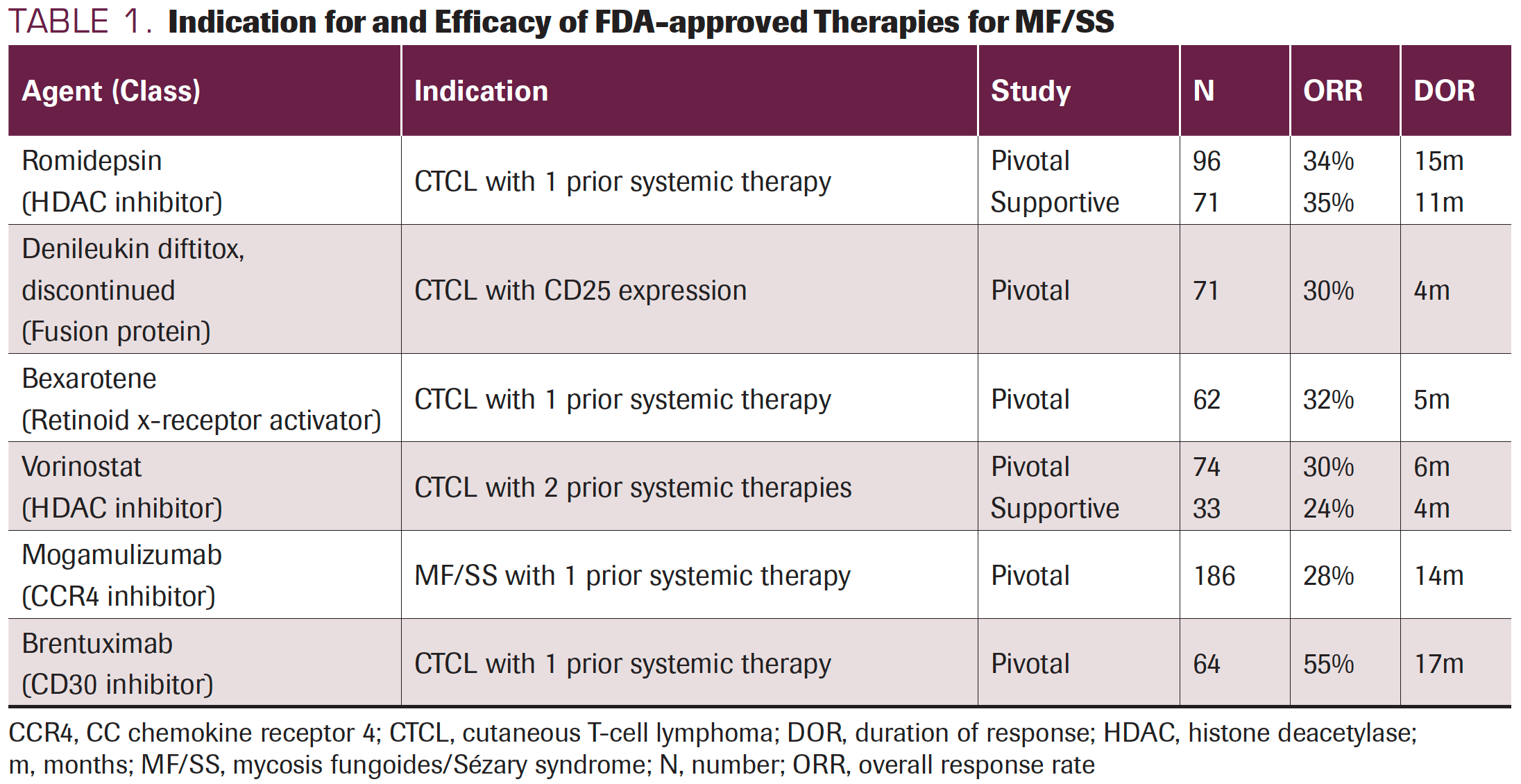
TABLE 1. Indication for and Efficacy of FDA-approved Therapies for MF/SS
First-line Systemic Therapies
Extracorporeal photopheresis
In patients with erythrodermic MF and SS, the frontline therapy is extracorporeal photopheresis (ECP), which combines phototherapy with leukapheresis.13 ECP may be administered for 2 consecutive days every month or, if disease is progressing, every 2 weeks. ECP as monotherapy has been shown to have overall response rates (ORRs) ranging from 33% to 75%.14,15 Studies demonstrate that ECP prolongs survival in patients with erythrodermic and advanced MF/SS, and they support the use of ECP as first-line treatment for many patients with stage III and IV disease. Photopheresis may be combined with immunomodulatory agents like oral retinoids and interferon.
Oral retinoids
Oral retinoids are often selected as first-line systemic therapy for patients who have failed SDT (Table 2). Two phase 2 trials led to the FDA approval of oral bexarotene based on the ORR of 48% at the optimal dose of 300 mg/m2 daily in a combined group of patients with early and advanced-stage MF/SS.16,17 In practice, oral bexarotene is started at 75 mg to 150 mg daily with gradual escalation to a goal dose of 300 mg/m2 daily. Because bexarotene causes central hypothyroidism leading to hypertriglyceridemia, we initiate patients on low-dose levothyroxine (eg, 25-75 mcg daily) and fenofibrate 145 mg daily. There is a cumulative dose effect of bexarotene, and it may take 6 or more months for a response at the lower dose range. Bexarotene is the only FDA-approved retinoid for MF/SS. However, other retinoids such as acitretin and isotretinoin may be less cost-prohibitive and associated with similar efficacy.18 Retinoids have been combined with other therapies and used for maintenance after EBT.
Interferons and interleukins
As the immune system of patients with advanced-stage MF/SS is shifted toward T-helper 2 (Th2) cytokines, treatment with interferons (IFNs) may aid in restoring the T-helper 1 (Th1)/ Th2 balance.19 IFN-α and pegylated IFN-α both have demonstrated efficacy of 64%, making them among the more effective therapies used alone or in combination with ECP or retinoids.20 IFN-γ is as effective as IFN-α and tends to be associated with fewer AEs.
IL-12 activates NK cells and cytotoxic CD8+ T cells, thereby potentiating the production of IFN-γ and reversing the drift from Th1 to Th2 cytokines. A phase 1 trial of recombinant human IL-12 (rhIL-12) administered intralesionally or subcutaneously twice weekly for up to 24 weeks demonstrated clinical response across multiple disease phenotypes.21 Our phase 2 trial of rhIL-12 in patients with early-stage MF found that twice-weekly subcutaneous administration of rhIL-12 showed an ORR of 43%.22 IL-12 is not commercially available, but it is a promising agent that warrants further investigation.
Histone deacetylase inhibitors
Histone deacetylase inhibitors (HDACi) are small molecules that block deacetylation of tumor suppressor genes and cell cycle regulatory pathways. Vorinostat is an oral HDACi that is FDA-approved for the treatment of MF/SS; its ORR is 29%.23,24 Vorinostat has been largely replaced by romidepsin, an FDA-approved HDACi that is given intravenously (IV) weekly for 3 consecutive weeks of a 4-week cycle. A phase 2 trial demonstrated an ORR of 34%.25 Responses were seen across all stages and disease subtypes. Multiple clinical trials utilizing these inhibitors in combination with other treatments are under investigation.
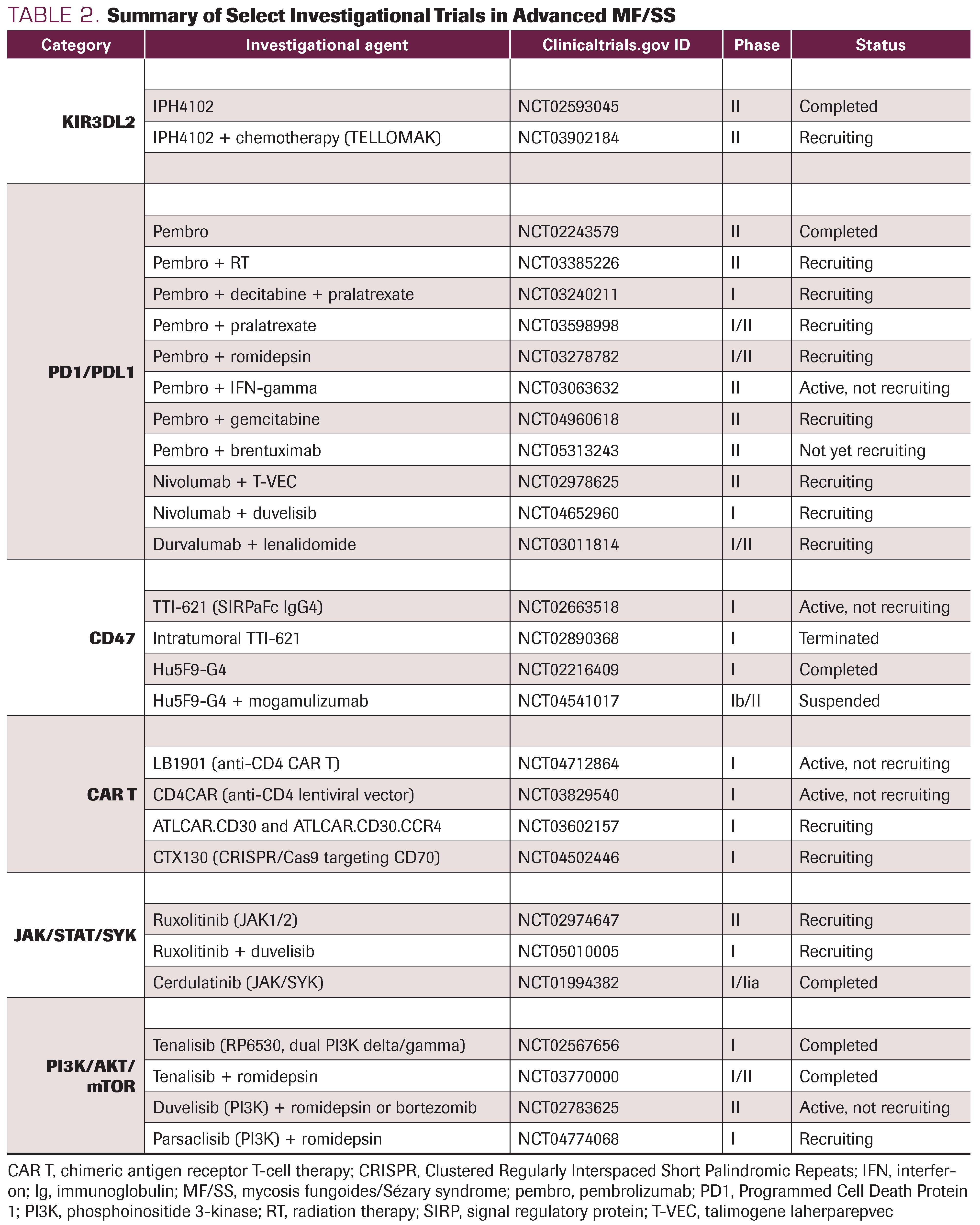
TABLE 2. Summary of Select Investigational Trials in Advanced MF/SS
Targeted Immunotherapies
E7777
Initially known as denileukin diftitox (Ontak), E7777 is emerging as a more stable and less toxic recombinant fusion protein. As Ontak, this agent was initially evaluated in a phase 1 study of patients with hematologic malignancies expressing CD25, and it demonstrated an ORR of 37%, including 5 complete responses.26 A 2-dose randomized study of patients with stage IB-IVA MF/SS showed an ORR of 30%.27 A second randomized study of patients with stage IA-III MF/ SS demonstrated an ORR of 44%.28 Patients whose skin biopsy had greater than 25% CD25 expression appeared to perform better (ORR, 78%) than patients having low to undetectable expression (ORR, 20%). These pivotal studies led to the full approval by the FDA in 2008. However, Ontak was withdrawn in 2014 for inconsistencies in the folding of the protein, and the new formulation, E7777, has since been in development. A recent phase 2 registration trial in 71 patients established a dose of 9 ug/kg/day.29 Preliminary results show an ORR of 44%. Potential AEs are infusion reactions and capillary leak syndrome. Guidelines to prevent and manage capillary leak syndrome have been developed.30
Brentuximab vedotin
Brentuximab vedotin (BV) is an antibody-drug conjugate to monomethyl auristatin E that targets CD30. In a phase 2 trial, high response rates were seen in patients with MF (54%), primary cutaneous anaplastic large cell lymphoma (100%), and lymphomatoid papulosis (100%).31 Patients with MF demonstrated similar response rates, irrespective of low, medium, or high CD30 expression (50%, 58%, and 50%, respectively). In a parallel phase 2 trial of patients with stage IB-IV MF/SS, ORR was 70%.32 Clinical responses were seen across all levels of CD30 expression, although median CD30max was higher in responders than in nonresponders. The randomized phase 3 ALCANZA trial showed that BV was superior to physician’s choice (oral bexarotene or methotrexate) in patients with CD30+ CTCL based on an ORR lasting at least 4 months (56.3% vs 12.5%).33 Longer median progression-free survival (PFS) intervals were observed in patients treated with BV compared with physician’s choice (16.7 vs 3.5 months).
Peripheral neuropathy is the major dose-related AE, seen in 67% of patients. After discontinuing treatment, symptoms improve with time in most patients.
Mogamulizumab
Mogamulizumab is a humanized monoclonal antibody that is defucosylated to enhance antibody-dependent cellular cytotoxicity. Its target is the CC chemokine receptor 4 (CCR4), a receptor expressed by malignant cells across multiple clinical phenotypes in MF/SS and also on the surface of Th2 and regulatory T cells (Tregs).
A phase 1/2 trial in 41 patients with MF/SS demonstrated an ORR of 37%, including a response in 18 of 19 (95%) patients with B1 or greater blood involvement.34 In the phase 3 MAVORIC registration trial, 372 patients with MF/SS were randomized to receive either mogamulizumab (1 mg/ kg IV weekly for 4 weeks, then every 2 weeks) or vorinostat.35 Global ORR was 28% for patients treated with mogamulizumab, and a higher ORR of 47% in patients with SS was observed.
Mogamulizumab-associated rash (MAR) is seen in 16% to 24% of treated patients. Skin biopsies may aid in distinguishing MAR from disease, as MAR demonstrates features of spongiotic, psoriasiform, or interface dermatitis with a predominance of CD8+ T cells. Given mogamulizumab’s profound effect in reducing Tregs, which are integral to successful engraftment, mogamulizumab should not be administered in the months leading up to alloHSCT.
IPH4102
KIR3DL2 (also known as CD158k) is a member of a family of inhibitory killer cell immunoglobulin-like receptors (KIRs) found on NK cells. KIR3DL2 is expressed in more than 85% of patients with SS. It has been proposed as a diagnostic and prognostic marker for SS that is superior to loss of CD26 or CD7. IPH4102, also known as lacutamab, is a fully humanized monoclonal antibody targeting KIR3DL2 that binds to receptors of target cells, inducing NK-cell mediated lysis. A phase 1, international, multicenter trial of 44 patients with MF/SS demonstrated an ORR of 43% in SS patients with minimal AEs.36 A phase 2 trial (TELLOMAK; NCT03902184) is ongoing to study the efficacy of IPH4102 alone or in combination with chemotherapy in patients with advanced MF/SS.
Pembrolizumab and nivolumab
The use of immune checkpoint inhibitors, such as the anti–PD-1 agents pembrolizumab and nivolumab, has demonstrated how reinvigorating exhausted tumor-infiltrating lymphocytes may restore the host antitumor response in many cancers. Their role in MF/SS is less defined owing to the expression of these markers on both nonmalignant and malignant T cells. Hence, blocking PD-1 in malignant cells in T-cell lymphomas may theoretically promote tumor growth. Treatment with pembrolizumab resulted in an ORR of 38% in patients with advanced MF/SS in a phase 2 trial.37 A transient disease flare characterized by erythroderma and pruritus was seen in more than half of patients with SS. The phase 1 study of nivolumab in patients with hematologic malignancy also demonstrated clinical responses in 15% of patients with MF/SS.38 Ongoing trials are studying the use of checkpoint inhibitors in combination with other therapies (Table 2).
Single-Agent Chemotherapy
Folate antagonists
Pralatrexate is a dihydrofolate reductase inhibitor with higher activity and greater selectivity for cancer cells than methotrexate. In a dose de-escalation study in CTCL, pralatrexate 15 mg/m2/week for 3 of 4 weeks resulted in an ORR of 45%.39 We found that addition of oral bexarotene at 150-300 mg/m2 based on preclinical activity enhanced the efficacy to an ORR of 61%; the safety profile was consistent with that previously seen with individual study drugs.40 Durable responses were observed, with a median PFS of 12.8 months. We recommend pretreatment with oral folinic acid (leucovorin) at 25 mg twice daily for 3 days at the start of each pralatrexate cycle and vitamin B12 at 1 mg intramuscularly every 8 to 10 weeks.
Gemcitabine
Gemcitabine is a pyrimidine nucleoside analogue. Its use in patients with CTCL has been studied, utilizing a dose of 1000-1200 mg/m2/week for 3 of 4 weeks.41 A dose reduction—treatment for 2 weeks rather than 3—has been used in the elderly with good tolerability. In our phase 2 trial of patients with advanced CTCL, we observed an ORR of 68% (17 of 25 patients).42 Gemcitabine should be administered carefully in patients with a recent history of radiation given the potential for radiation recall.
Liposomal doxorubicin
Liposomal doxorubicin (Doxil) is an anthracycline with antineoplastic effects. In the first published study of liposomal doxorubicin in patients with MF, treatment of 20 mg/m2 once monthly resulted in an ORR of 80% (8 of 10 patients).43
Combination chemotherapy
Patients with advanced MF/SS, especially those with large cell transformation, may develop tumors and bulky lymphadenopathy so severe and extensive that combination chemotherapy may be considered. Several regimens have been used, but no data suggest that one is better than another. Romidepsin and E7777 have been studied in combination with CHOP (cyclophosphamide, vincristine, prednisone, and bleomycin), and studies of mogamulizumab with CHOP in other T-cell lymphomas are ongoing (Table 2). Response rates may be high, but responses are often short-lived without increased survival. Subsequent relapsed disease may be even more aggressive, and the risk of immunosuppression associated with chemotherapy may result in high morbidity and mortality from opportunistic infections in patients with whose skin and/or immune system are already compromised.
Other Investigational Agents
Bortezomib
Bortezomib inhibits proteasome-dependent NF-κB signaling. A phase 2 study of bortezomib in 12 patients with advanced MF or peripheral T-cell lymphoma (PTCL) with isolated skin involvement demonstrated an ORR of 67%.44 Patients were treated with a dose of 1.3 mg/m2 twice weekly for 2 weeks followed by 1 week off. Treatment was well tolerated and responses were durable, lasting 7 to 14 months. In vitro studies have suggested that bortezomib may also enhance the activity of HDACi.
Lenalidomide
Lenalidomide is an oral immunomodulatory agent that induces Th1 cytokine production and augments NK cell cytotoxicity. In a phase 2 exploratory trial, lenalidomide was found to be active in patients with advanced MF/SS with an ORR of 28% (9 of 32 patients, all partial responses).45 Many patients were unable to tolerate 25 mg daily. Although doses of 10 mg daily were better tolerated, they were not as effective. In a small, sequential phase 1 study, lenalidomide demonstrated efficacy in combination with romidepsin with an ORR of 44% (4 of 9 patients).46
JAK-STAT inhibitors
Janus kinase-signal transducer and activator of transcription (JAK-STAT) is a signaling pathway that is critical in mediating inflammatory skin diseases, including atopic dermatitis, psoriasis, alopecia areata, and vitiligo. Mutations in the JAK-STAT pathway have been reported in SS cells by whole genome sequencing. In a phase 2 trial evaluating oral ruxolitinib, a JAK1/2 inhibitor, in patients with T-cell lymphoma with or without activating JAK-STAT mutations, 1 of 7 patients with MF/ SS demonstrated a clinical response.47
SYK inhibitors
Overexpression of SYK, a protein tyrosine kinase, occurs in T cell lymphomas and is thought to contribute to malignant cell growth and survival. In a phase 2 study of cerdulatinib, a dual SYK/JAK inhibitor, in patients with T-cell lymphoma, ORR was 35% with the highest activity in patients with MF (ORR 45%).48 Rapid improvements in pruritus occurred, and several patients experienced a durable response.
PI3K inhibitors
Modulation of phosphatidylinositol 3-kinase (PI3K), a lipid kinase involved in intracellular signal transduction, may contribute to the survival and differentiation of malignant tumor cells. Duvelisib and tenalisib are PI3K inhibitors with activity against the δ and γ isoforms, which are key effectors in the innate and adaptive immune response and in modulating the tumor microenvironment through tumor-associated macrophages. A phase 1 study of duvelisib demonstrated an ORR of 32% in MF/SS.49 A phase 1/1b study of tenalisib in patients with T-cell lymphoma showed an ORR of 45% in MF/SS.50
Anti-CD47
CD47 has garnered much interest as a macrophage checkpoint (or “do not eat me” signal) that is overexpressed in many cancer types. In a phase 1 study of intralesional TT1-621, a CD47- SIRPα inhibitor, 35 patients with MF/ SS were treated in a sequential dose escalation study with intralesional TT1-621 alone or in combination with pembrolizumab or pegylated IFN-α.51 A response in Composite Assessment of Index Lesion Severity (CAILS) score was seen in 34% (10 of 29 evaluable patients). A phase 1 study of IV TT1- 621 reported an ORR of 21% in 29 patients with MF/SS.52
Chimeric Antigen Receptor
Chimeric antigen receptor (CAR T) are an emerging therapy in which the patient’s own CD8+ T cells are engineered and expanded in culture to recognize and eliminate tumor-specific antigen, independent of MHC. In 2017, the first CAR T therapy was approved for the treatment of B-cell lymphoma using a CD19 target. However, the use of therapy in patients with T-cell lymphoma may offer unique challenges because sustained elimination of T-cells would result in severe immunosuppression with infectious complications. To optimize “on-target, off-tumor” selection, CAR T-cells using targets CD30 and CCR4 are being studied in advanced MF/SS (Table 2).
Allogeneic stem cell Transplantation
AlloHSCT may result in long-term remission in a subset of patients with MF/SS and should be considered upfront for younger patients in otherwise good health who are refractory to multiple therapies or who demonstrate a high-risk profile of disease with poor life expectancy. Optimizing timing of alloHSCT when the disease is well controlled is critical, as alloHSCT administered while the patient has clinically active disease or poor immunity due to treatment toxicity may lead to relapse.
Preparatory cytoreduction with reduced-intensity or nonmyeloablative regimens is preferred as patients with advanced MF/SS are older, and posttransplant infectious complications may contribute to high morbidity and mortality in the setting of immunosuppression and skin barrier breakdown. TSEBT is often an important component because the skin is a frequent site of posttransplant relapse.
The preparatory regimen at The University of Texas MD Anderson Cancer Center incorporates TSEBT and nonmyeloablative conditioning with fludarabine and antithymocyte globulin (ATG).53 We have observed durable remissions in patients with SS after alloHSCT (13/24 patients; 54%).54 A Stanford University group has reported on their experience in patients with advanced MF/SS using the conditioning regimen of TSEBT, total lymphoid irradiation, and ATG, citing clinical and molecular remission in 43% of patients and 5-year OS of 56%.13
Treatment algorithm in advanced disease
There is no standard treatment or sequence of treatments for patients with advanced MF/SS. Treatment selection is predicated on clinical stage as well as burden of activity within each disease compartment (skin, blood, nodal, and visceral). At MD Anderson Cancer Center, we begin with therapies associated with fewer toxicities that may still offer a high response rate and durability of response. For patients with leukemic disease, treatment with oral bexarotene, ECP, and mogamulizumab are considered to be frontline therapies, with early evaluation for alloHSCT in the appropriate populations. In contrast, patients with tumors or bulky lymph node disease, especially those with large cell transformation, may be preferentially considered for treatment with BV or pralatrexate. In our experience, management with chemotherapy portends worse outcomes. Integration of relevant biomarkers, such as CD30 for BV and other next generation– sequencing mutational panels for investigational agents (eg, CCR4, KIR3DL2, JAK) should be assessed for targetable mutations. Finally, skin-directed treatment with topicals, phototherapy, and radiation (TSEBT or to individual lesions) should be incorporated to augment treatment response and enhance quality of life. Treatment within a multidisciplinary team— including dermatologists, oncologists, radiation oncologists, and bone marrow transplant specialists—is ideal for comprehensive care.
Supportive Care
Patients with erythrodermic MF or SS who are having flares are often colonized with staphylococcus aureus (S aureus), which can develop into methicillin-resistant S aureus. Colonization must be eliminated for the patient to improve. Soaking in a bathtub of water mixed with a half-cup of bleach may help decolonize bacteria from the skin. Mupirocin 2% ointment may be useful for decolonization of nares and skin lesions.
We do not favor use of systemic corticosteroids for symptom palliation, as we frequently observe steroid dependence with resistance to subsequent therapies.
Pruritus may profoundly affect quality of life in patients with MF/ SS. Effective management will lessen patients’ psychological and emotional burden and also minimize secondary skin infection through less frequent manipulation of the skin. Topical steroids may offer temporary relief from pruritus and should be integrated with gentle emollients to optimize the skin barrier. Oral agents, such as gabapentin and aprepitant, may offer additional relief. Although oral antihistamines are generally ineffective for relieving severe pruritus, an evening dose may be considered for its sedating effects.
AUTHOR AFFILIATIONS:
Julia Dai, MD1; and Madeleine Duvic, MD1
1Department of Dermatology, University of Texas MD Anderson Cancer Center, Houston, TX.
CORRESPONDING AUTHOR:
Julia Dai, MD
Department of Dermatology
University of Texas MD Anderson Cancer Center
1515 Holcombe Blvd
Faculty Center Tower, Floor 11, Box 1452
Houston, TX 77030
Tel: 713-515-7961
Email: jdai6@mdanderson.org
CONFLICT OF INTEREST STATEMENT
MD has served on the Soligenix scientific advisory board and has received consulting fees from Bioniz, Codiac, and Citius.
FUNDING SOURCES
None.
REFERENCES
- Jawed SI, Myskowski PL, Horwitz S, Moskowitz A, Querfeld C. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70(2):205.e1-e16; quiz 221-222. doi:10.1016/j.jaad.2013.07.049
- Kaye FJ, Bunn PA Jr, Steinberg SM, et al. A randomized trial comparing combination electron-beam radiation and chemotherapy with topical therapy in the initial treatment of mycosis fungoides. N Engl J Med. 1989;321(26):1784-1790. doi:10.1056/NEJM198912283212603
- Lessin SR, Duvic M, Guitart J, et al. Topical chemotherapy in cutaneous T-cell lymphoma: positive results of a randomized, controlled, multicenter trial testing the efficacy and safety of a novel mechlorethamine, 0.02%, gel in mycosis fungoides. JAMA Dermatol. 2013;149(1):25-32. doi:10.1001/2013.jamadermatol.541
- Breneman D, Duvic M, Kuzel T, Yocum R, Truglia J, Stevens VJ. Phase 1 and 2 trial of bexarotene gel for skin-directed treatment of patients with cutaneous T-cell lymphoma. Arch Dermatol. 2002;138(3):325-332. doi:10.1001/archderm.138.3.325. Published correction appears in Arch Dermatol. 2002;138(10):1386.
- Rook AH, Gelfand JM, Wysocka M, et al. Topical resiquimod can induce disease regression and enhance T-cell effector functions in cutaneous T-cell lymphoma. Blood. 2015;126(12):1452-1461. doi:10.1182/blood-2015-02-630335. Published correction appears in Blood. 2015;126(25):2765.
- Ortiz-Romero PL, Maroñas Jiménez L, Muniesa C, et al. Activity and safety of topical pimecrolimus in patients with early stage mycosis fungoides (PimTo-MF): a single-arm, multicentre, phase 2 trial. Lancet Haematol. 2022;9(6):e425-e433. doi:10.1016/S2352-3026(22)00107-7
- Olsen EA, Hodak E, Anderson T, et al. Guidelines for phototherapy of mycosis fungoides and Sézary syndrome: a consensus statement of the United States Cutaneous Lymphoma Consortium. J Am Acad Dermatol. 2016;74(1):27-58. doi:10.1016/j.jaad.2015.09.033
- Rook AH, Wood GS, Duvic M, Vonderheid EC, Tobia A, Cabana B. A phase II placebo-controlled study of photodynamic therapy with topical hypericin and visible light irradiation in the treatment of cutaneous T-cell lymphoma and psoriasis. J Am Acad Dermatol. 2010;63(6):984-990. doi:10.1016/j.jaad.2010.02.039
- Kim EJ, Mangold AR, DeSimone JA, et al. Efficacy and safety of topical hypericin photodynamic therapy for early-stage cutaneous T-cell lymphoma (mycosis fungoides): the FLASH phase 3 randomized clinical trial. JAMA Dermatol. 2022;158(9):1031-1039. doi:10.1001/jamadermatol.2022.2749
- Hoppe RT, Harrison C, Tavallaee M, et al. Low-dose total skin electron beam therapy as an effective modality to reduce disease burden in patients with mycosis fungoides: results of a pooled analysis from 3 phase-II clinical trials. J Am Acad Dermatol. 2015;72(2):286-292. doi:10.1016/j.jaad.2014.10.014
- Duvic M, Donato M, Dabaja B, et al. Total skin electron beam and non-myeloablative allogeneic hematopoietic stem-cell transplantation in advanced mycosis fungoides and Sezary syndrome. J Clin Oncol. 2010;28(14):2365-2372. doi:10.1200/JCO.2009.25.8301
- Weng W-K, Arai S, Rezvani A, et al. Nonmyeloablative allogeneic transplantation achieves clinical and molecular remission in cutaneous T-cell lymphoma. Blood Adv. 2020;4(18):4474-4482. doi:10.1182/bloodadvances.2020001627
- Gao C, McCormack C, van der Weyden C, et al. Prolonged survival with the early use of a novel extracorporeal photopheresis regimen in patients with Sézary syndrome. Blood. 2019;134(16):1346-1350. doi:10.1182/blood.2019000765
- Stevens SR, Bowen GM, Duvic M, et al. Effectiveness of photopheresis in Sézary syndrome. Arch Dermatol. 1999;135(8):995-997. doi:10.1001/archderm.135.8.995-a
- Quaglino P, Knobler R, Fierro MT, et al. Extracorporeal photopheresis for the treatment of erythrodermic cutaneous T-cell lymphoma: a single center clinical experience with long-term follow-up data and a brief overview of the literature. Int J Dermatol. 2013;52(11):1308-1318. doi:10.1111/ijd.12121
- Duvic M, Hymes K, Heald P, et al; Bexarotene Worldwide Study Group. Bexarotene is effective and safe for treatment of refractory advanced-stage cutaneous T-cell lymphoma: multinational phase II-III trial results. J Clin Oncol. 2001;19(9):2456-2471. doi:10.1200/JCO.2001.19.9.2456
- Duvic M, Martin AG, Kim Y, et al; Worldwide Bexarotene Study Group. Phase 2 and 3 clinical trial of oral bexarotene (Targretin capsules) for the treatment of refractory or persistent early-stage cutaneous T-cell lymphoma. Arch Dermatol. 2001;137(5):581-593.
- Molin L, Thomsen K, Volden G, et al. Oral retinoids in mycosis fungoides and Sézary syndrome: a comparison of isotretinoin and etretinate. a study from the Scandinavian Mycosis Fungoides Group. Acta Derm Venereol. 1987;67(3):232-236.
- Suchin KR, Cassin M, Gottleib SL, et al. Increased interleukin 5 production in eosinophilic Sézary syndrome: regulation by interferon alfa and interleukin 12. J Am Acad Dermatol. 2001;44(1):28-32. doi:10.1067/mjd.2001.109853
- Olsen EA, Rosen ST, Vollmer RT, et al. Interferon alfa-2a in the treatment of cutaneous T cell lymphoma. J Am Acad Dermatol. 1989;20(3):395-407. doi:10.1016/s0190-9622(89)70049-9
- Rook AH, Wood GS, Yoo EK, et al. Interleukin-12 therapy of cutaneous T-cell lymphoma induces lesion regression and cytotoxic T-cell responses. Blood. 1999;94(3):902-908.
- Duvic M, Sherman ML, Wood GS, et al. A phase II open-label study of recombinant human interleukin-12 in patients with stage IA, IB, or IIA mycosis fungoides. J Am Acad Dermatol. 2006;55(5):807-813. doi:10.1016/j.jaad.2006.06.038
- Duvic M, Talpur R, Ni X, et al. Phase 2 trial of oral vorinostat (suberoylanilide hydroxamic acid, SAHA) for refractory cutaneous T-cell lymphoma (CTCL). Blood. 2007;109(1):31-39. doi:10.1182/blood-2006-06-025999. Published correction appears in Blood. 2007;109(12):5086.
- Olsen EA, Kim YH, Kuzel TM, et al. Phase IIb multicenter trial of vorinostat in patients with persistent, progressive, or treatment refractory cutaneous T-cell lymphoma. J Clin Oncol. 2007;25(21):3109-3115. doi:10.1200/JCO.2006.10.2434
- Whittaker SJ, Demierre M-F, Kim EJ, et al. Final results from a multicenter, international, pivotal study of romidepsin in refractory cutaneous T-cell lymphoma. J Clin Oncol. 2010;28(29):4485-4491. doi:10.1200/JCO.2010.28.9066
- LeMaistre CF, Saleh MN, Kuzel TM, et al. Phase I trial of a ligand fusion-protein (DAB389IL-2) in lymphomas expressing the receptor for interleukin-2. Blood. 1998;91(2):399-405.
- Olsen E, Duvic M, Frankel A, et al. Pivotal phase III trial of two dose levels of denileukin diftitox for the treatment of cutaneous T-cell lymphoma. J Clin Oncol. 2001;19(2):376-388. doi:10.1200/JCO.2001.19.2.376
- Prince HM, Duvic M, Martin A, et al. Phase III placebo-controlled trial of denileukin diftitox for patients with cutaneous T-cell lymphoma. J Clin Oncol. 2010;28(11):1870-1877. doi:10.1200/JCO.2009.26.2386
- Kawai H, Ando K, Maruyama D, et al. Phase II study of E7777 in Japanese patients with relapsed/refractory peripheral and cutaneous T-cell lymphoma. Cancer Sci. 2021;112(6):2426-2435. doi:10.1111/cas.14906
- Duvic M, Talpur R. Optimizing denileukin diftitox (Ontak) therapy. Future Oncol. 2008;4(4):457-469. doi:10.2217/14796694.4.4.457
- Duvic M, Tetzlaff MT, Gangar P, Clos AL, Sui D, Talpur R. Results of a phase II trial of brentuximab vedotin for CD30+ cutaneous T-cell lymphoma and lymphomatoid papulosis. J Clin Oncol. 2015;33(32):3759-3765. doi:10.1200/JCO.2014.60.3787
- Kim YH, Tavallaee M, Sundram U, et al. Phase II investigator-initiated study of brentuximab vedotin in mycosis fungoides and Sézary syndrome with variable CD30 expression level: a multi-institution collaborative project. J Clin Oncol. 2015;33(32):3750-3758. doi:10.1200/JCO.2014.60.3969
- Prince HM, Kim YH, Horwitz SM, et al; ALCANZA study group. Brentuximab vedotin or physician’s choice in CD30-positive cutaneous T-cell lymphoma (ALCANZA): an international, open-label, randomised, phase 3, multicentre trial. Lancet. 2017;390(10094):555-566. doi:10.1016/S0140-6736(17)31266-7
- Duvic M, Pinter-Brown LC, Foss FM, et al. Phase 1/2 study of mogamulizumab, a defucosylated anti-CCR4 antibody, in previously treated patients with cutaneous T-cell lymphoma. Blood. 2015;125(12):1883-1889. doi:10.1182/blood-2014-09-600924
- Kim YH, Bagot M, Pinter-Brown L, et al; MAVORIC Investigators. Mogamulizumab versus vorinostat in previously treated cutaneous T-cell lymphoma (MAVORIC): an international, open-label, randomised, controlled phase 3 trial. Lancet Oncol. 2018;19(9):1192-1204. doi:10.1016/S1470-2045(18)30379-6. Published correction appears in Lancet Oncol. 2018;19(11):e581.
- Bagot M, Porcu P, Marie-Cardine A, et al. IPH4102, a first-in-class anti-KIR3DL2 monoclonal antibody, in patients with relapsed or refractory cutaneous T-cell lymphoma: an international, first-in-human, open-label, phase 1 trial. Lancet Oncol. 2019;20(8):1160-1170. doi:10.1016/S1470-2045(19)30320-1
- Khodadoust MS, Rook AH, Porcu P, et al. Pembrolizumab in relapsed and refractory mycosis fungoides and Sézary syndrome: a multicenter phase II study. J Clin Oncol. 2020;38(1):20-28. doi:10.1200/JCO.19.01056
- Lesokhin AM, Ansell SM, Armand P, et al. Nivolumab in patients with relapsed or refractory hematologic malignancy: preliminary results of a phase Ib study. J Clin Oncol. 2016;34(23):2698-2704. doi:10.1200/JCO.2015.65.9789
- Horwitz SM, Kim YH, Foss F, et al. Identification of an active, well-tolerated dose of pralatrexate in patients with relapsed or refractory cutaneous T-cell lymphoma. Blood. 2012;119(18):4115-4122. doi:10.1182/blood-2011-11-390211
- Duvic M, Kim YH, Zinzani PL, Horwitz SM. Results from a phase I/II open-label, dose-finding study of pralatrexate and oral bexarotene in patients with relapsed/refractory cutaneous T-cell lymphoma. Clin Cancer Res.2017;23(14):3552-3556. doi:10.1158/1078-0432.CCR-16-2064
- Zinzani PL, Venturini F, Stefoni V, et al. Gemcitabine as single agent in pretreated T-cell lymphoma patients: evaluation of the long-term outcome. Ann Oncol. 2010;21(4):860-863. doi:10.1093/annonc/mdp508
- Duvic M, Talpur R, Wen S, Kurzrock R, David CL, Apisarnthanarax N. Phase II evaluation of gemcitabine monotherapy for cutaneous T-cell lymphoma. Clin Lymphoma Myeloma.2006;7(1): 51-58. doi:10.3816/CLM.2006.n.039
- Wollina U, Graefe T, Kaatz M. Pegylated doxorubicin for primary cutaneous T-cell lymphoma: a report on ten patients with follow-up. J Cancer Res Clin Oncol. 2001;127(2):128-134. doi:10.1007/s004320000178
- Zinzani PL, Musuraca G, Tani M, et al. Phase II trial of proteasome inhibitor bortezomib in patients with relapsed or refractory cutaneous T-cell lymphoma. J Clin Oncol. 2007;25(27):4293-4297. doi:10.1200/jco.2007.11.4207
- Querfeld C, Rosen ST, Guitart J, et al. Results of an open-label multicenter phase 2 trial of lenalidomide monotherapy in refractory mycosis fungoides and Sézary syndrome. Blood. 2014;123(8):1159-1166. doi:10.1182/blood-2013-09-525915
- Mehta-Shah N, Lunning MA, Moskowitz AJ, et al. Romidepsin and lenalidomide-based regimens have efficacy in relapsed/refractory lymphoma: combined analysis of two phase I studies with expansion cohorts. Am J Hematol. 2021;96(10):1211-1222. doi:10.1002/ajh.26288
- Moskowitz AJ, Ghione P, Jacobsen E, et al. A phase 2 biomarker-driven study of ruxolitinib demonstrates effectiveness of JAK/STAT targeting in T-cell lymphomas. Blood. 2021;138(26):2828-2837. doi:10.1182/blood.2021013379
- Horwitz SM, Feldman TA, Hess BT, et al. A phase 2 study of the dual SYK/JAK inhibitor cerdulatinib demonstrates good tolerability and clinical response in relapsed/refractory peripheral T-cell lymphoma and cutaneous T-cell lymphoma. Blood.2019;134(Suppl 1):466. doi:10.1182/blood-2019-123986
- Horwitz SM, Koch R, Porcu P, et al. Activity of the PI3K-δ,γ inhibitor duvelisib in a phase 1 trial and preclinical models of T-cell lymphoma. Blood. 2018;131(8):888-898. doi:10.1182/blood-2017-08-802470
- Huen A, Haverkos BM, Zain J, et al. Phase I/Ib study of tenalisib (RP6530), a dual PI3K δ/γ inhibitor in patients with relapsed/refractory T-cell lymphoma. Cancers (Basel). 2020;12(8):2293. doi:10.3390/cancers12082293
- Querfeld C, Thompson JA, Taylor MH, et al. Intralesional TTI-621, a novel biologic targeting the innate immune checkpoint CD47, in patients with relapsed or refractory mycosis fungoides or Sézary syndrome: a multicentre, phase 1 study. Lancet Haematol. 2021;8(11):e808-e817. doi:10.1016/S2352-3026(21)00271-4
- Ansell SM, Maris MB, Lesokhin AM, et al. Phase I study of the CD47 blocker TTI-621 in patients with relapsed or refractory hematologic malignancies. Clin Cancer Res. 2021;27(8):2190-2199. doi:10.1158/1078-0432.CCR-20-3706
- Hosing C, Bassett R, Dabaja B, et al. Allogeneic stem-cell transplantation in patients with cutaneous lymphoma: updated results from a single institution. Ann Oncol. 2015;26(12):2490-2495. doi:10.1093/annonc/mdv473
- Polansky M, Talpur R, Daulat S, Hosing C, Dabaja B, Duvic M. Long-term complete responses to combination therapies and allogeneic stem cell transplants in patients with Sézary syndrome. Clin Lymphoma Myeloma Leuk. 2015;15(5):e83-e93. doi:10.1016/j.clml.2014.09.013
Highlighting Insights From the Marginal Zone Lymphoma Workshop
Clinicians outline the significance of the MZL Workshop, where a gathering of international experts in the field discussed updates in the disease state.