Data Show Improved Posttransplant Outcomes in Elderly AML Population
Real-world data may serve as a benchmark for future studies in elderly patients with acute myeloid leukemia.
“In tandem with the marked increase in elderly patients receiving allo-HSCT, we observed an impressive improvement over time in [LFS] and [OS]. These data indicate that allo-HSCT should no longer be optional but should be mandatory for elderly patient,” according to Ali Bazarbachi, MD, PhD.
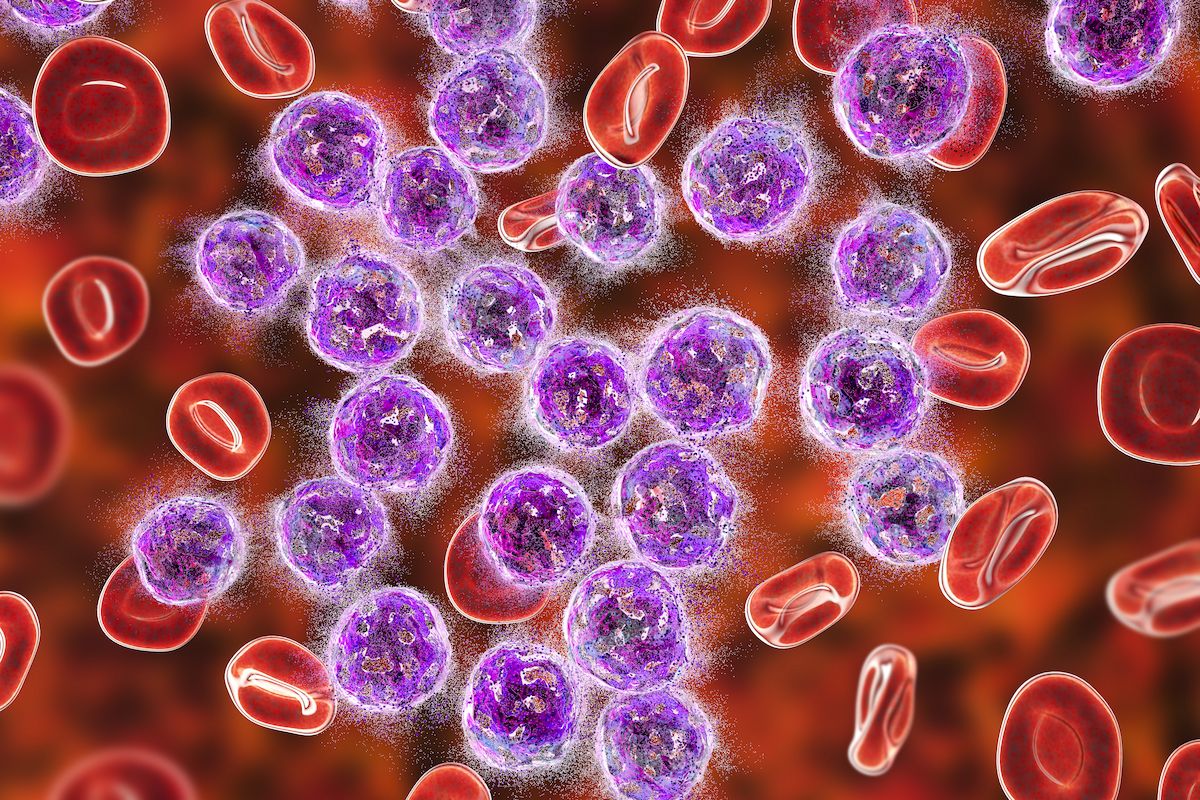
Outcomes following allogeneic hematopoietic stem cell transplantation (allo-HSCT) have improved over time regardless of disease status at the time of transplant among elderly patients with acute myeloid leukemia (AML), according to findings published in Clinical Cancer Research.1
With a median follow-up of 40 months (IQR, 38-42), the 3-year incidence of relapse changed from 37% to 31% and then to 30% across the 3 periods of 2000 to 2009, 2010 to 2014, and 2015 to 2021 (P = .001). At 3 years, leukemia-free survival (LFS) increased from 32% to 38% and then to 44% (P = .001), and overall survival (OS) increased from 37% to 42% and then to 49% (P = .001). Relapse incidence significantly decreased while LFS, OS, and graft-vs-host disease (GVHD)–free and relapse-free survival (GRFS) significantly increased after 2015 compared with other periods based on multivariate analysis.
For patients in first complete remission (CR1), LFS changed from 39% to 44% and then to 47% across each relevant period (P = .005); investigators reported an increase in OS from 43% to 48% and then to 52% (P = .006). Among those in second or subsequent CR (CR2+), LFS changed from 29% to 40% and then to 47% over time (P = .001), while OS went from 37% to 44% and then to 52% (P = .001).
“Over time, significant progress in allo-HSCT has decreased mortality and allowed for the delivery of allo-HSCT to older patients. However, little information is available about the global impact of these changes and the predictive factors for post-transplant outcomes, and available data on outcomes from retrospective and prospective studies are mixed,” senior author Ali Bazarbachi, MD, PhD, a professor of medicine, anatomy, and cell biology and physiological sciences; associate dean for basic research; and director of the Bone Marrow Transplantation Program at the American University of Beirut-Medical Center in Lebanon, said in a press release on these findings.2
“We hoped these large-scale, real-world data could serve as a benchmark for future studies in this setting. Our study represents one of the largest analyses to date assessing trends over time and predictive factors for outcomes in elderly [patients with] AML after allo-HSCT,” he added.
Investigators of this retrospective, registry-based, multicenter study assessed outcomes in 7215 adult patients with AML who received an allograft transplant from 2000 to 2021. Patients 65 years and older with matched sibling donors, 10/10 or 9/10 unrelated donors, or haploidentical donors were eligible to be included in this analysis. Investigators also included those who had stem cell sources in the bone marrow or G-CSF–mobilized peripheral blood; patients who underwent in vitro T-cell depletion were not included in the analysis.
Specifically, the analysis included 728 patients who underwent a transplant from 2000 to 2009, 1775 who received treatment from 2010 to 2014, and 4712 who were treated between 2015 and 2021. Investigators reported NPM1 mutations in and FLT3 ITD in 37% and 30% of patients, respectively. Additionally, 64% of patients were in CR1, 14% were in CR2+, and 22% had active disease at the time of transplant.
According to the investigators, patients who underwent a transplant in more recent years were more likely to be older, in CR1, and have an adverse-risk karyotype. Additionally, it was less probable for those who received a transplant more recently to have a matched sibling donor.
“In tandem with the marked increase in elderly patients receiving allo-HSCT, we observed an impressive improvement over time in [LFS] and [OS]. These data indicate that allo-HSCT should no longer be optional but should be mandatory for elderly patient,” Bazarbachi concluded.2
References
- Bazarbachi A, Labopin M, Moukalled N, et al. Improvements in posttransplant outcomes over two decades in older patients with acute myeloid leukemia in the EBMT ALWP Study.Clin Cancer Res. Published online March 22, 2024. doi:10.1158/1078-0432.CCR-23-3673.
- Outcomes after stem cell transplant in elderly patients with acute myeloid leukemia have improved since 2000. News release. American Association for Cancer Research. March 22, 2024. Accessed April 9, 2024. https://tinyurl.com/4hmt4trv
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.