Delirium Affects Circadian Rhythm of Breakthrough Pain
MONTREAL-Delirium in patients with advanced cancer appeared to be associated with changes in the circadian distribution of analgesia for breakthrough pain and may be due to a reversal of the normal circadian rhythm in these patients, reported Bruno Gagnon, MD, of McGill University and Montreal General Hospital.
MONTREALDelirium in patients with advanced cancer appeared to be associated with changes in the circadian distribution of analgesia for breakthrough pain and may be due to a reversal of the normal circadian rhythm in these patients, reported Bruno Gagnon, MD, of McGill University and Montreal General Hospital.
The study was conducted as part of a prospective study of delirium in advanced cancer patients in the acute palliative care unit at Grey Nuns Community Hospital & Health Centre, Edmonton, Alberta. The patient charts were retrospectively analyzed for breakthrough analgesia use; however, the patients, nurses, and physicians were blinded to the fact that the review would be carried out.
Breakthrough analgesia use was divided into three time periods: 11:30 pm to 7:30 am (night); 7:30 am to 3:30 pm (day), and 3:30 pm to 11:30 pm (evening), corresponding to the length of the nursing shifts.
The study included 104 eligible patients categorized into three groups based on delirium status: Group 1 (n = 33) had no delirium on admission or during their hospital stay; group 2 (n = 22) had terminal or nonreversible delirium; and group 3 (n = 49) had a changing delirium status (at least one period of delirium in addition to one or more delirium-free periods).
A total of 1,677 patient admission days were analyzed for circadian distribution of breakthrough analgesia doses: 1,254 days without delirium and 423 days with delirium. The researchers found that the circadian distribution of breakthrough analgesia doses differed significantly from a random distribution in both patients with and without delirium (J Pain Symptom Manage 22:826-833, 2001).
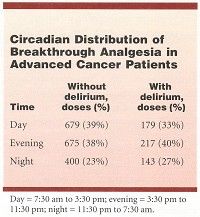
During delirium-free days, patients required more breakthrough analgesia doses during the daytime, compared with a random distribution, whereas when delirium was present, more breakthrough analgesia was used during the evening and at night (see Table).
Similarly, the group 2 patients (terminal delirium) received more breakthrough analgesic doses during the evening, compared with the group 1 (no delirium) patients. Furthermore, among the group 3 patients (changing delirium status), the highest breakthrough analgesia use was during the evening when delirium was present and during the day when delirium was absent.
"Future research studies in advanced cancer patients should screen for the presence of delirium to acknowledge its potential impact on the circadian distribution of breakthrough analgesia use," Dr. Gagnon and his colleagues said.
In clinical practice, they said, physicians "should suspect delirium and test for its presence, especially when a patient’s pattern of breakthrough analgesia use shows a preponderance for evening or nighttime."
One possible explanation for the greater breakthrough analgesia use during the evening in the presence of delirium, the authors said, relates to the fact that patients with delirium can experience a disturbance of their sleep-awake cycle (sleeping during the day and being awake in the evening and at night).