Durvalumab Plus Bevacizumab Improves PFS Outcomes in Unresectable HCC
Phase 3 EMERALD-1 trial results reveal that no new adverse events were identified with durvalumab plus bevacizumab in patients with unresectable HCC.
Phase 3 EMERALD-1 trial results reveal that no new adverse events were identified with durvalumab plus bevacizumab in patients with unresectable HCC.
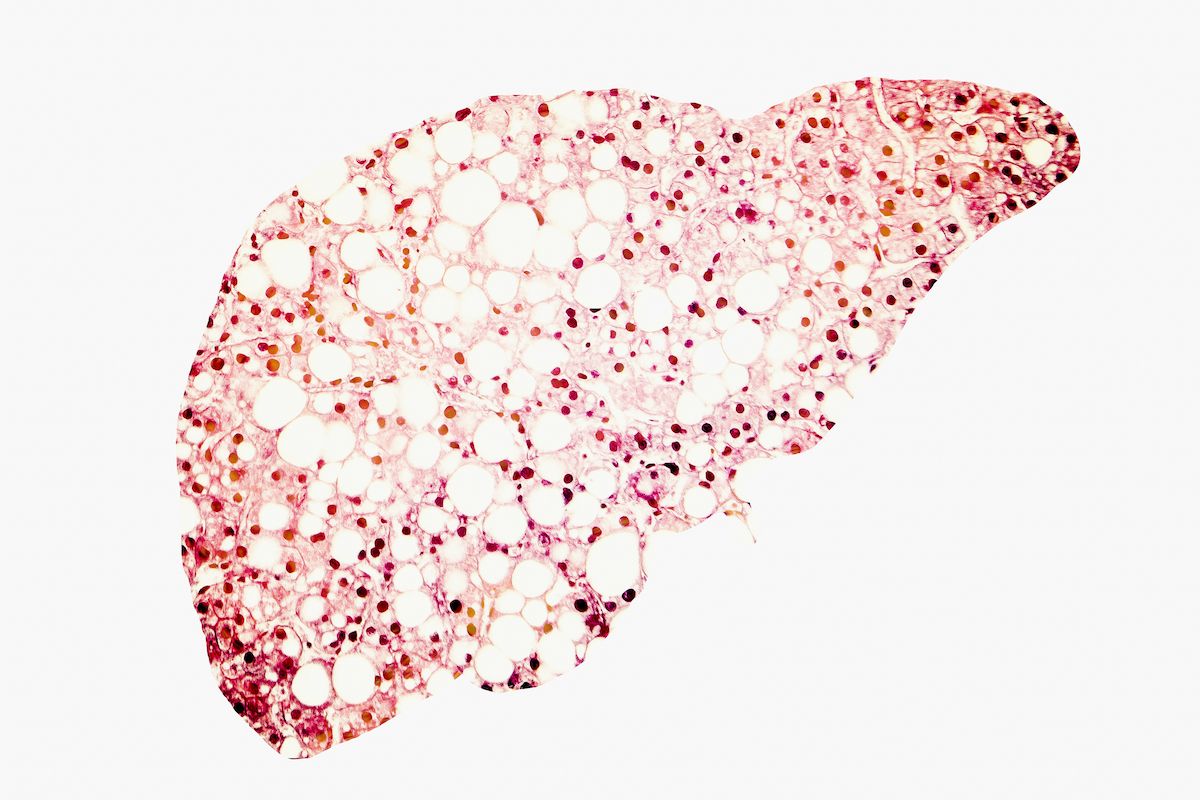
Durvalumab (Imfinzi), in combination with bevacizumab (Avastin) plus transarterial chemoembolization (TACE) met its primary end point of progression-free survival (PFS) when treating adult patients with unresectable hepatocellular carcinoma (HCC) amenable to embolization, according to results from the phase 3 EMERALD trial (NCT03778957) published in The Lancet.
Investigators found that at the data cutoff, the median duration of follow-up for PFS was 27.9 months (95% CI, 27.4-30.4), median PFS was 15.0 months (95% CI, 11.1-18.9) with durvalumab plus bevacizumab vs 8.2 months (95% CI, 6.9-11.1) with placebo (HR, 0.77; 95% CI, 0.61-0.98; two-sided log-rank P = .032). Furthermore, durvalumab plus placebo alone, which elicited a median PFS of 10.0 months (95% CI, 9.0-12.7), did not significantly improve PFS over placebo alone of 8.2 months (95% CI, 6.9-11.1; HR, 0.94; 95% CI, 0.75-1.19; two-sided log-rank P = .64). A total 22% of the combination group, 19% of the durvalumab group, and 16% of the placebo group remained progression free as of data cutoff.
“The EMERALD1 study was positive: durvalumab plus bevacizumab and TACE significantly improved [PFS] compared with TACE alone, with no new adverse effects identified in a heterogeneous population of participants with unresectable hepatocellular carcinoma amenable to [embolization],” Bruno Sangro, MD, director of the Liver Unit and professor of Internal Medicine at Clínica Universidad de Navarra, Pamplona, Spain, said in the publication with study coinvestigators. “Additional follow-up and analyses, as well as the final overall survival analysis, will help [characterize] the potential role of durvalumab plus bevacizumab plus TACE as a new standard of care in this population.”
A total of 887 patients were screened for the trial, with 616 eligible for enrollment. Eligible patients were randomly assigned 1:1:1 to receive durvalumab plus bevacizumab (n = 204), durvalumab plus placebo (n = 207), or placebo alone (n = 205). Randomization was stratified by TACE modality, geographical region, and portal vein invasion.
In the durvalumab plus bevacizumab group, patients were given 1500 mg of intravenous (IV) durvalumab plus TACE once every 4 weeks, followed by 1120 mg of concurrent durvalumab plus 15 mg/kg of IV bevacizumab once every 3 weeks. Patients in the durvalumab plus placebo group received the same regimen with IV sterile saline in place of bevacizumab. Additionally, patients in the placebo group received TACE plus sterile saline or dextrose solution intravenously once every 4 weeks, followed by concurrent placebo once every 3 weeks.
The median age was 65.0 years (IQR, 59.0-72.0), patients were predominantly male (78%), 61% were Asian, and 29% were White. Most patients received 1 (30%) or 2 (33%) TACE procedures. Additionally, 25% of the combination group, 30% of the durvalumab plus placebo group, and 21% of the placebo only group had oesophageal varices at baseline.
The primary study end point was PFS by blinded independent committee review (BICR) per RECIST with durvalumab plus bevacizumab vs placebo alone. Key secondary end points included PFS with durvalumab plus placebo vs placebo alone, overall survival, and time to deterioration of European Organization for Research and Treatment of Cancer (EORTC-QLQ-C30 and EORTC QLQ-HCC18.
Safety analysis reveals that treatment-related adverse events (TRAEs) occurred in 81% and 45% of the combination and placebo arms, respectively. Furthermore, grade 3 or 4 TRAEs occurred in 27% and 6% of respective arms, including 19% and 5% experiencing serious TRAEs. Furthermore, TRAEs leading to discontinuations occurred in 12% of the combination arm and 3% of the placebo arm, respectively, with TRAEs leading to deaths occurring in 10% and 6% of each arm.
Reference
Sangro B, Kudo M, Erinjeri JP, et al. Durvalumab with or without bevacizumab with transarterial chemoembolisation in hepatocellular carcinoma (EMERALD-1): a multiregional, randomised, double-blind, placebo-controlled, phase 3 study. Lancet. Published online January 8, 2025. doi:10.1016/ S0140-6736(24)02680-1