ECC: PD-L1 Inhibition Yields Good Responses in NSCLC Patients Who Smoke
A novel agent that inhibits the PD-1/PD-L1 pathway showed good results in particular among smokers with non-small-cell lung cancer, a particularly promising result from a phase I trial.
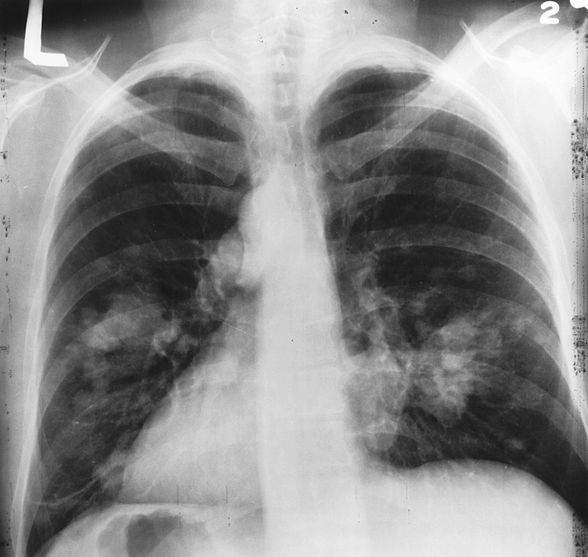
X-ray image of chest with possible lung cancer growth on the left side of the lung.
A novel agent that inhibits the PD-1/PD-L1 pathway showed good results in particular among smokers with non–small-cell lung cancer (NSCLC), a particularly promising result from a phase I trial.
“This is the first study to suggest a potential relationship between smoking history and response to inhibiting the PD-L1/PD-1 pathway-a pathway that is instrumental in enabling cancer cells to escape detection by the immune system,” said Jean-Charles Soria, MD, PhD, of the Institut Gustave Roussy in France, during his presentation at the European Cancer Congress (ECC) in Amsterdam. The new study was a phase I trial of MPDL3280A, a human monoclonal antibody that blocks PD-L1 from binding to receptors including PD-1 and B7.1.
Though ongoing, Dr. Soria presented efficacy data on 53 patients and safety data in 85 patients, all with squamous or nonsquamous NSCLC. The overall response rate was 26% among smokers, compared with only 10% of patients who never smoked. Among those who did respond to the treatment with MPDL3280A, the treatment duration ranged from 170 to 534 days. Some patients responded within 6 weeks, and the median time to first response was 11.9 weeks.
Patients with higher expression in tumor cells of PD-L1 were more likely to respond to the study drug than those with lower expression. Those in the highest quartile of expression had a response rate of 83%, and those in the highest two quartiles combined responded at a 46% rate.
The treatment was considered generally well tolerated, though the rate of grade 3/4 adverse events was 34%. These included pericardial effusion, dehydration, dyspnea, and fatigue. There were no pneumonitis-related deaths.
“Our results so far demonstrate that the compound is capable of producing striking and durable responses in non–small-cell lung cancer patients with metastatic disease who have failed to respond to previous chemotherapy,” Dr. Soria said. “The study defines a novel approach to identifying the patients most likely to respond to treatment and identifies potential association between smoking and responses to MPDL3280A. A new therapy, with few serious adverse side-effects, that is easy to use-one intravenous infusion every 3 weeks-and a robust clinical activity as a single agent should soon be available.”
The current president of the European Cancer Organization, Cornelis van de Velde, added that this is “an extremely important study. Hundreds of millions of Euros have been spent chasing the dream of immunotherapy for lung cancer patients, but with zero results.” The early findings on MPDL3280A, however, suggest such a therapy may potentially be on the way.