Engineered T Cells Elicit Clinical Response in Advanced Myeloma
Eighty percent of patients with advanced multiple myeloma had a clinical response to a new T cell–receptor therapy that used T cells to target cells expressing NY-ESO-1.
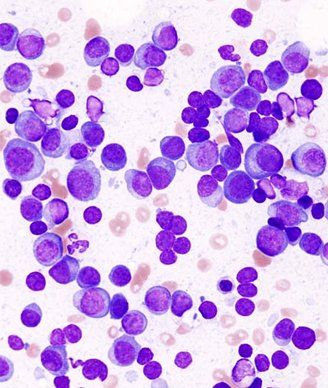
Multiple myeloma, May-Grünwald-Giemsa stain. Image © KGH
Results of a phase I/II study found that 80% of patients with advanced multiple myeloma had a clinical response to a new T cell–receptor therapy that used T cells to target cells expressing NY-ESO-1.
“We show in this study that infusion of ex vivo–expanded NY-ESOc259 TCR–engineered T cells was well-tolerated without significant safety concerns and that engineered T cells expanded in vivo, trafficked to disease tissue, persisted and showed durable target-specific antitumor activity,” wrote Aaron P. Rapoport, MD, of the University of Maryland School of Medicine, and colleagues in Nature Medicine.
In the study, 20 patients with NY-ESO-01 and/or LAGE-1 antigen–positive advanced multiple myeloma underwent apheresis to have T cells removed and then received a median of 2.4 billion NY-ESO-1 engineered CD3 T cells 2 days after undergoing autologous stem cell transplantation (ASCT).
According to the study, the engineered T cells expanded, persisted, trafficked to marrow, and exhibited a cytotoxic phenotype.
With a median follow-up of 21.1 months, 15 of 20 patients were alive, including 10 patients who were also progression free. Sixteen of the 20 patients (80%) had a clinical response to treatment. Fourteen patients had a complete response and two patients had a very good partial response.
“This is encouraging, given the predisposition of patients on our study to worse outcomes owing to an enrollment requirement for high-risk or advanced disease, a considerable frequency of prior ASCT and the known association of cancer-testis antigen expression with poor prognosis,” the researchers wrote.
With a median follow-up of 30.1 months, the median progression-free survival was 19.1 months and the median overall survival was 32.1 months.
The researchers observed that disease progression was associated with the loss of gene-modified T cells, suggesting that methods for sustaining long-term persistence of engineered T cells in more patients may improve outcomes.
“Taken together, our data support the continued development of NY-ESO-1– and LAGE-1–TCR–engineered T cells for treatment of myeloma and suggest that methods for enhancing long-term survival and function of the cells may improve treatment durability,” the researchers wrote. “Such strategies may include repeat infusions and/or incorporation of immune-modulatory agents such as checkpoint inhibitors and maintenance lenalidomide.”
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.