ESMO 2025: Key Anticipated Updates in Breast and Lung Tumors
Trials slated for presentation at the 2025 ESMO Congress may reveal practice-changing data across different breast and lung cancer populations.
Prior data from the phase 3 DESTINY-Breast05 trial (NCT04622319) showed that trastuzumab deruxtecan prolonged invasive disease-free survival vs trastuzumab emtansine among patients with HER2-positive breast cancer and residual invasive disease following neoadjuvant therapy.
Researchers and clinicians from around the world are gearing up for the 2025 European Society for Medical Oncology (ESMO) Annual Congress in Berlin, Germany. On the horizon are highly anticipated reports and updates regarding novel therapeutic approaches, translational data, and other innovations that may move the needle across different cancer types and specialties.
This year’s meeting will include a wide range of late-breaking abstracts and presentations showcasing developments in various breast and lung cancer populations. From data focusing on the triple-negative setting to trials exploring HER2 alterations in lung tumors, here are some of the notable abstracts that may shape clinical practice in the future.
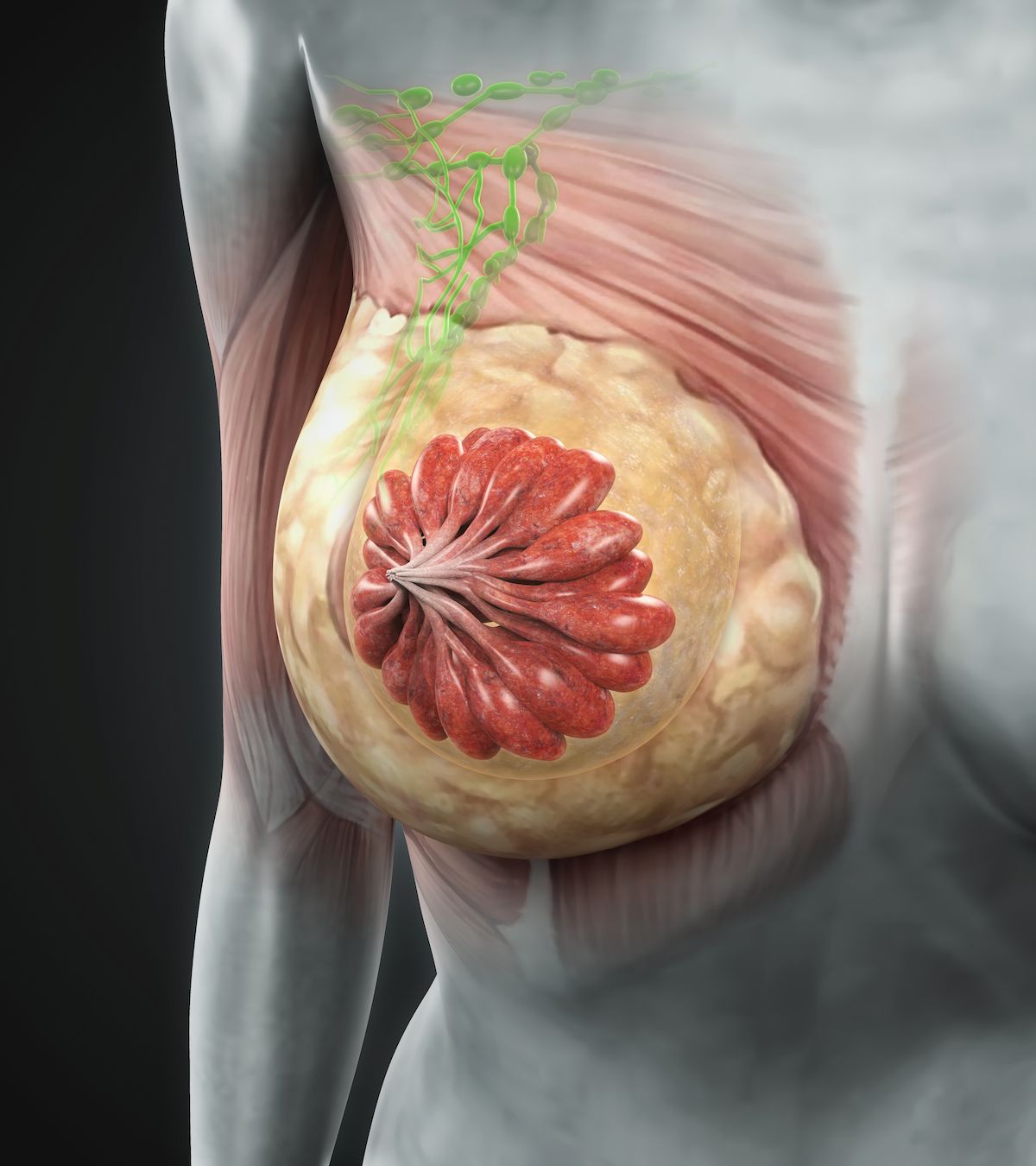
What to Watch in Breast Cancer
LBA1: Trastuzumab deruxtecan (T-DXd) vs trastuzumab emtansine (T-DM1) in patients (pts) with high-risk human epidermal growth factor receptor 2–positive (HER2+) primary breast cancer (BC) with residual invasive disease after neoadjuvant therapy (tx): Interim analysis of DESTINY-Breast05.
Presentation: October 18, 4:52 – 5:04 PM CEST by Charles E Geyer Jr., MD
In a letter to the readers from Neil M. Iyengar, MD, co-director of Breast Medical Oncology, director of Cancer Survivorship Services, and associate professor of Hematology and Medical Oncology at Winship Cancer Institute at Emory University, and the co-editor-in-chief of ONCOLOGY®, he identified the late-breaking abstract on the phase 3 DESTINY-Breast05 trial (NCT04622319) as a presentation to look out for at the meeting. He noted the study as a potential “advancement in the treatment of high-risk, early-stage HER2-positive breast cancer.”
Investigators recently shared topline data from a planned interim analysis showing that fam-trastuzumab deruxtecan (T-DXd; Enhertu) prolonged invasive disease-free survival (iDFS) vs trastuzumab emtansine (T-DM1; Kadcyla) among those with residual invasive disease in the breast or axillary lymph nodes following prior neoadjuvant therapy.1 At the time of analysis, the safety profile of T-DXd appeared to be consistent with prior reports of the agent.
LBA20: Primary results from ASCENT-03: a randomized phase 3 study of sacituzumab govitecan (SG) vs chemotherapy (Chemo) in patients (pts) with previously untreated advanced triple-negative breast cancer (TNBC) who are unable to receive PD-(L)1 inhibitors (PD-[L]1i).
Presentation: October 19, 9:15 – 9:25 AM CEST by Javier Cortés, MD, PhD
In the realm of triple-negative disease, Iyengar highlighted a late-breaking abstract on findings from the phase 3 ASCENT-03 study (NCT05382299) evaluating sacituzumab govitecan-hziy (Trodelvy) vs chemotherapy for patients with frontline disease.
According to findings that investigators shared in May 2025, sacituzumab govitecan significantly prolonged progression-free survival (PFS) vs chemotherapy in this patient population.2 There appeared to be no detriment to overall survival (OS) with the use of sacituzumab govitecan, although data for this end point were not yet mature.
At the time of this analysis, principal trial investigator Javier Cortés, MD, head of the International Breast Cancer Center in Spain, stated that approximately half of patients “with metastatic triple-negative breast cancer [TNBC] do not receive treatment” after frontline therapy, which demonstrated an “urgent need for innovative treatment options in this early setting.”2 Given that traditional chemotherapy has functioned as “the standard of care for early treatment of metastatic [TNBC],” Cortes stated that “therapeutic advances in this disease area serve a critical unmet need for patients and the broader oncology community.”
LBA21: First-line (1L) datopotamab deruxtecan (Dato-DXd) vs chemotherapy in patients with locally recurrent inoperable or metastatic triple-negative breast cancer (mTNBC) for whom immunotherapy was not an option: primary results from the randomised, phase 3 TROPION-Breast02 trial.
Presentation: October 19, 9:25 – 9:35 AM CEST by Rebecca Dent, MD, MSc
According to a post on X3 from Paolo Tarantino, MD, PhD (@PTarantinoMD), another anticipated update in breast cancer relates to the phase 3 TROPION-Breast02 trial (NCT05374512) evaluating datopotamab deruxtecan (dato-DXd; Datroway) in the front-line setting vs investigator’s choice of chemotherapy among patients with recurrent inoperable or metastatic TNBC who are ineligible to receive chemotherapy.
Recent topline data from TROPION-Breast02 showed that dato-DXd produced significant improvements in the primary end points of PFS and OS vs chemotherapy across this population.4 The safety profile of the experimental therapy was comparable with previous reports of the agent.
Tarantino, a research fellow at the Dana-Farber Cancer Institute, noted that the data comparing dato-DXd vs chemotherapy in frontline immunotherapy-ineligible metastatic TNBC will “likely” be “practice-changing.”3 He described how the trial may “lead to a third TOPO1 antibody drug conjugate [ADC]” becoming “available for [metastatic] TNBC,” which may pose the subsequent question of how to best sequence these ADCs.
“As we recognize Breast Cancer Awareness Month, these data remind us that awareness must fuel investment in research and equitable access to innovations,” Iyengar wrote regarding this anticipated research. “The progress on display at ESMO is not just scientific progress; it is human progress, representing the combined efforts of patients, clinicians, and scientists determined to outpace breast cancer.”
The Latest to Look for in Lung Cancer
LBA4: Phase III study of ivonescimab plus chemotherapy versus tislelizumab plus chemotherapy as first-line treatment for advanced squamous non-small cell lung cancer (HARMONi-6).
Presentation: October 19, 4:30 – 4:42 PM CEST by Lu Shun, MD, PhD
In a post on X5, Amol Akhade, MD, a medical oncologist at Hiranandani Hospital (@SuyogCancer), identified the top lung cancer data he was anticipating at the latest ESMO meeting. A key late-breaking abstract he described was the phase 3 HARMONi-6 study (NCT05840016) investigating the first-in-class PD-1/VEGF bispecific antibody ivonescimab plus chemotherapy vs tislelizumab-jsgr (Tevimbra) and chemotherapy as frontline therapy for patients with advanced squamous non–small cell lung cancer (NSCLC).
Previously, developers announced prespecified interim analysis findings from HARMONi-6, which showed that the ivonescimab combination reached the trial’s primary end point of PFS.6 Across the intention-to-treat (ITT) population, ivonescimab plus chemotherapy appeared to “decisively beat” tislelizumab in terms of PFS outcomes. The investigational combination also conferred clinically meaningful PFS benefits in patients with PD-L1–positive and PD-L1–negative disease.
At the time of analysis, ivonescimab produced no new safety signals. The incidences of grade 3 or higher bleeding events and treatment-related serious adverse effects (AEs) were comparable between treatment arms.
Principal investigator Lu Shun, MD, PhD, director of Shanghai Lung Cancer, Shanghai Chest Hospital, Shanghai Jiao Tong University School of Medicine, described the findings of HARMONi-6 as a “breakthrough” that “not only advances the treatment of [NSCLC] but also marks a significant milestone in global oncology immunotherapy.”6 Furthermore, he stated that ivonescimab may offer “a promising new treatment option for patients with advanced squamous carcinoma,” one that may “overcome the limitations of bevacizumab [Avastin] in treating squamous [NSCLC]” while improving the “clinical benefits of immunotherapy for NSCLC.”
LBA74: Zongertinib as first-line treatment in patients with advanced HER2-mutant NSCLC: Beamion LUNG 1
Presentation: October 17, 4:32 – 4:42 PM CEST by Sanjay Popat, BSc, MBBS, FRCP, PhD
Another notable late-breaking abstract is a presentation on updated results from the phase 1b Beamion LUNG-1 trial (NCT04886804), in which patients with advanced HER2-mutated NSCLC were assigned to receive treatment with zongertinib (Hernexeos). Of note, this presentation will reveal findings among patients who received zongertinib in the frontline setting.
Prior data from the Beamion LUNG-1 trial supported the FDA’s accelerated approval of zongertinib for adults with previously managed metastatic or unresectable nonsquamous NSCLC harboring HER2 tyrosine kinase domain (TKD)–activating mutations, in August 2025.7 Among 71 patients who received prior treatment with platinum-based chemotherapy and no anti-HER2 tyrosine kinase inhibitors or ADCs, zongertinib yielded an objective response rate (ORR) of 75% (95% CI, 63%-83%), with 58% maintaining a response for 6 months or longer. Among 34 patients who received prior chemotherapy and a HER2-targeting ADC, these respective rates were 44% (95% CI, 29%-61%) and 27%.
As part of an upcoming proffered paper session, new data from Beamion LUNG-1 may reveal whether the clinical benefits of zongertinib also extend to an earlier treatment setting.
LBA75: Sevabertinib (BAY 2927088) in advanced HER2-mutant non-small cell lung cancer (NSCLC): results from the SOHO-01 study
Presentation: October 17, 4:22 – 4:32 PM CEST by Xiuning Le, MD, PhD
Another trial with regulatory implications in the lung cancer world is the phase 1/2 SOHO-01 trial (NCT05099172), the findings of which will be exhibited in a proffered paper session at ESMO. Investigators assessed sevabertinib as a treatment for patients with HER2-mutated NSCLC.
In May 2025, the FDA granted priority review to a new drug application for sevabertinib among patients with previously treated HER2-mutated NSCLC based on data from the SOHO-01 trial.8 Previous findings shared at the 2025 American Society of Clinical Oncology (ASCO) Annual Meeting demonstrated an ORR of 59.3% (95% CI, 47.8%-70.1%) per investigator assessment and 60.5% (95% CI, 49.0%-71.2%) per blinded independent central review among patients with pretreated HER2-mutated NSCLC.9 Responses with zongertinib appeared to be consistent across patient subgroups in the pretreated population.
According to Herbert H. Loong, FASCO, FRCP, MBBS, clinical associate professor in the Department of Clinical Oncology and the deputy medical director of the Phase 1 Clinical Trials Centre at The Chinese University of Hong Kong, in China, the presented data at ASCO showed that zongertinib produced “meaningful and durable responses” in this pretreated NSCLC population.9
References
- ENHERTU (fam-trastuzumab deruxtecan-nxki) demonstrated highly statistically significant and clinically meaningful improvement in invasive disease-free survival vs. T-DM1 in DESTINY-Breast05 phase III trial in patients with high-risk early breast cancer following neoadjuvant therapy. News release. AstraZeneca. September 29, 2025. Accessed October 13, 2025. https://tinyurl.com/4v3ax79f
- ASCENT-03: Trodelvy demonstrates highly statistically significant & clinically meaningful improvement in progression free survival in patients with first-line metastatic triple-negative breast cancer who are not candidates for checkpoint inhibitors. News release. Gilead. May 23, 2025. Accessed October 13, 2025. https://tinyurl.com/kzckwdbw
- @PTarantinoMD. One week to #ESMO25. An unprecedented ESMO conference. Seven positive press releases, anticipating the expansion of T-DXd to the curative setting, two Trop2 ADCs reaching first-line mTNBC, 2 novel ET-based combos, adjuvant CDK4/6i improving OS. See you in Berlin! #ESMOAmbassadors. October 9, 2025. Accessed October 13, 2025. https://x.com/PTarantinoMD/status/1976244542853808316
- Datroway demonstrated statistically significant and clinically meaningful improvement in overall survival as 1st-line therapy for patients with metastatic triple-negative breast cancer for whom immunotherapy was not an option in TROPION-Breast02. News release. AstraZeneca. October 6, 2025. Accessed October 13, 2025. https://tinyurl.com/5a8a4r69
- @SuyogCancer. 🚨 Top #LungCancer highlights from #ESMO25 🚨HARMONi-6: Ivonescimab + chemo vs tislelizumab in 1L sqNSCLC OptiTROP-Lung04: TROP2 ADC after EGFR-TKI New HER2 TKIs – Zongertinib & Sevabertinib SKYSCRAPER-03: TIGIT + atezo vs PACIFIC standard ELEVATE: Ensartinib adjuvant in ALK+ NSCLC DeLLphi-304: DLL3 T-cell engager in SCLC ADCs, HER2, TIGIT & DLL3 — the next wave is here 🌊 #ESMO2025 @OncoAlert @OncBrothers @myESMO. September 29, 2025. Accessed October 13, 2025. https://x.com/SuyogCancer/status/1972844281623933411
- Ivonescimab in combination with chemotherapy demonstrates statistically significant and strongly positive results in first-line treatment of squamous non-small cell lung cancer (sq-NSCLC) vs. tislelizumab in combination with chemotherapy. News release. Akesobio. April 22, 2025. Accessed October 13, 2025. https://tinyurl.com/3r7379fu
- FDA grants accelerated approval to zongertinib for non-squamous NSCLC with HER2 TKD activating mutations. News release. FDA. August 8, 2025. Accessed October 13, 2025. https://tinyurl.com/bdh2d4uc
- U.S. FDA accepts new drug application under priority review for sevabertinib (BAY 2927088) in HER2-mutant non-small cell lung cancer. News release. Bayer. May 28, 2025. Accessed October 13, 2025. https://tinyurl.com/2t5vb5ky
- Loong HH, Li L, Wu L, et al. SOHO-01: Safety and efficacy of BAY 2927088 in patients with advanced HER2-mutant non-small cell lung cancer (NSCLC) who were pretreated but naïve to HER2-targeted therapy or had not received any treatment for advanced disease. J Clin Oncol. 2025;43(16):abstract 8504. doi:10.1200/JCO.2025.43.16_suppl.8504