The Evolving Biology of Castration-Resistant Prostate Cancer: Review of Recommendations From the Prostate Cancer Clinical Trials Working Group 3
We present a joint perspective from the medical oncology and urologic disciplines on the ongoing efforts to advance clinical trial performance in order to discover new therapies for this fatal disease.
Oncology (Williston Park). 30(2):187–195, 199.

Figure 1. Prostate Cancer Clinical States Model as Updated by the Prostate Cancer Clinical Trials Working Group 3 (PCWG3) Guidelines[14].
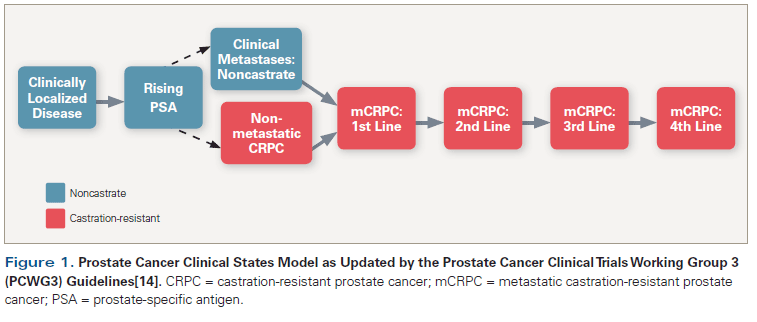
Figure 2. Histopathologic Variants of Metastatic Prostate Cancer
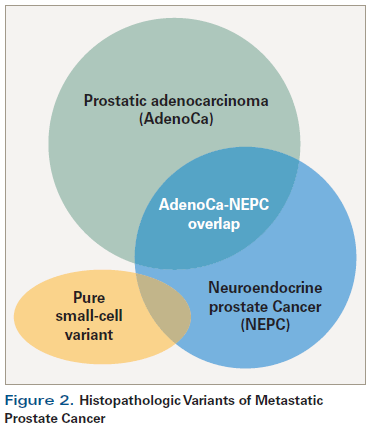
Table 1. Evolution of Recommendation Updates of Prostate Cancer Clinical Trials Working Group 3 (PCWG3) From PCWG2
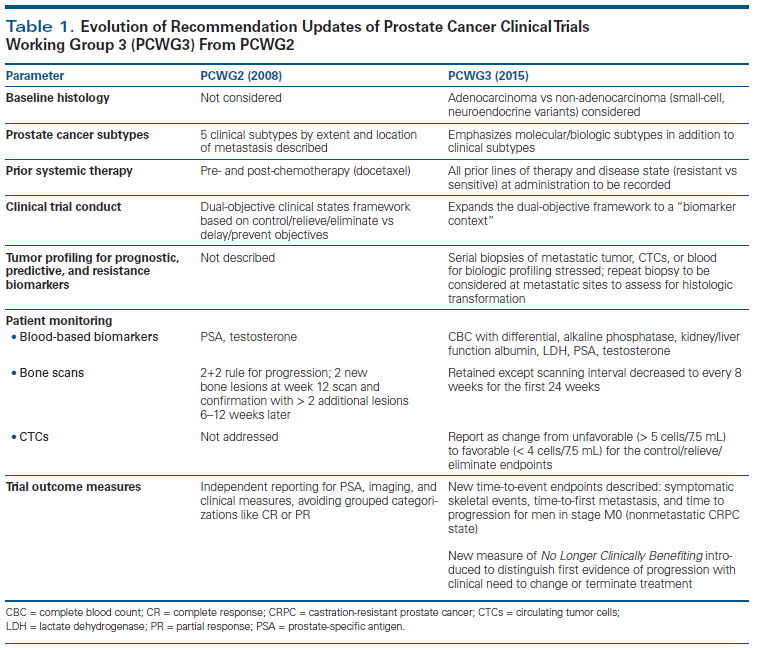
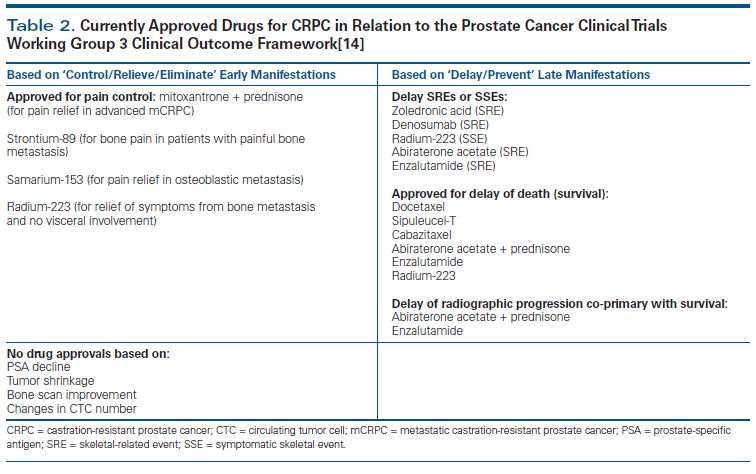
Table 2. Currently Approved Drugs for CRPC in Relation to the Prostate Cancer Clinical Trials Working Group 3 Clinical Outcome Framework[14]
In 2008, the Prostate Cancer Clinical Trials Working Group 2 (PCWG2) developed consensus guidelines for clinical trial design and conduct that redefined trial endpoints, with a dual-objective paradigm: to (1) controlling, relieving, or eliminating disease manifestations at the start of treatment; and (2) preventing or delaying further disease manifestations. Clinical and translational research in prostate cancer has expanded our current-day understanding of the mechanisms of its pathogenesis, as well as the different clinicopathologic and molecular subtypes of the disease, and has improved the therapeutic armamentarium for the management of metastatic castration-resistant prostate cancer (CRPC). These new advances led to the development of the updated PCWG3 guidelines in 2015. In this review, we analyze our evolving understanding of the biology of CRPC, acquired resistance mechanisms, and emerging therapeutic targets in light of the updated PCWG3 guidelines. We present a joint perspective from the medical oncology and urologic disciplines on the ongoing efforts to advance clinical trial performance in order to discover new therapies for this fatal disease.
Introduction
Historical perspective
Prostate cancer is currently the most common malignancy in men and accounted for approximately 233,000 (27%) new cases and 30,000 deaths in the United States in 2014.[1] Since the seminal discovery of the hormone dependence of prostate cancer by Huggins and colleagues more than 7 decades ago, androgen deprivation therapy (ADT) has been the main treatment strategy for metastatic prostate cancer.[2] However, after initial response to ADT, the disease progresses in about 2 to 3 years to a state of castration-resistant prostate cancer (CRPC).[3-5]
Docetaxel was the first agent that showed an improvement in overall survival (OS) in men with metastatic CRPC (mCRPC)and was approved in 2004 for this indication.[6] In 2008, a committee of investigators convened the Prostate Cancer Clinical Trials Working Group 2 (PCWG2) and outlined consensus guidelines for clinical trial design and conduct in mCRPC.[7] The PCWG2 applied a clinical states framework that based trial objectives, design, and outcomes on a dual-objective paradigm: (1) controlling, relieving, or eliminating disease manifestations as an early measure of response; and (2) preventing or delaying disease manifestations in progression as a later time-to-event measure. The clinical framework was based on stepwise milestones along the continuum of progressive disease, defined in terms of primary tumor, presence/absence of metastasis, and testosterone level (whether castrate [< 50 ng/dL] or not). These guidelines have aided in the performance of several well-designed clinical trials.[8,9]
Consequently, significant advances have been made in our current-day understanding of the biology of the evolution of CRPC. Since 2010, translational research has led to the regulatory approval of six new agents for the treatment of mCRPC, including chemotherapeutic agents (cabazitaxel), newer hormonal agents (abiraterone acetate, enzalutamide), immune therapy (sipuleucel-T), radiopharmaceuticals (radium-223 [Ra-223]), and bone-targeted agents (denosumab).[10-12] However, the impact of these therapies on survival has been less than optimal. There is still an acute need to better define predictive and prognostic markers, to optimally sequence the approved agents in treatment protocols, and to develop better targeted therapies.[10-13]
The PCWG3, a group of international experts in prostate cancer, worked from June 2012 to January 2015 to update the PCWG2 recommendations based on the latest advances in our understanding of the biology of mCRPC, newer approved therapeutic agents, detection of high frequency of actionable molecular alterations, and increased recognition of disease heterogeneity.[14]
Current Approved Agents for mCRPC
Chemotherapy
In 2004, the survival benefit of docetaxel was demonstrated in two large trials, making it the standard of care for mCRPC. The phase III TAX-327 trial, which recruited 1,006 chemotherapy-naive patients, showed a 3-month improvement in OS when docetaxel was compared with mitoxantrone treatment (hazard ratio [HR], 0.76 [95% CI, 0.62–0.94]).[15] The Southwestern Oncology Group (SWOG) 99-16 trial revealed a survival advantage of 1.9 months for the combination of docetaxel and estramustine compared with mitoxantrone (HR, 0.8 [95% CI, 0.67–0.97]).[6]
Cabazitaxel is a next-generation taxane approved in 2010 to overcome resistance to docetaxel. In the TROPIC trial, 755 patients who had progressed on docetaxel therapy were randomized to cabazitaxel vs mitoxantrone. Cabazitaxel treatment resulted in a 2.4-month longer median OS (15.1 vs 12.7 months) and a 1.4-month longer progression-free survival (PFS; 2.8 vs 1.4 months; for each, P < .0001). Adverse events noted with this drug were mainly hematologic: grade 3 to 4 neutropenia (82%), febrile neutropenia (8%), and diarrhea (47%).[16]
Role of chemotherapy in metastatic hormone-sensitive (ADT-naive) prostate cancer. In the randomized, open-label, phase III GETUG-AFU 15 trial, 385 men with metastatic hormone-sensitive prostate cancer were randomized between October 2004 and December 2008 to receive ADT plus docetaxel 75 mg/m2 every 3 weeks for 9 cycles (n = 192) or ADT alone (n = 193).[17] On an updated analysis, after a median follow-up of 83.9 months, the primary endpoint of median OS was 62.1 months (95% CI, 49.5–73.7 months) vs 48.6 months (95% CI, 40.9–60.6 months) for the ADT-plus-docetaxel and ADT-alone arms, respectively (HR, 0.88 [95% CI, 0.68–1.14]; P = .3). High-volume disease (HVD) was defined as visceral metastases and/or four or more bone metastases with at least one outside of the vertebral column or pelvis. For HVD patients, median OS was 39.8 months (95% CI, 28–53.4 months) vs 35.1 months (95% CI, 29.9–43.6 months) for the ADT-plus-docetaxel and ADT-alone arms, respectively (HR, 0.78 [95% CI, 0.56–1.09]; P = .14]. There was no significant difference in OS for the low-volume disease (LVD) patients. However, this post-hoc analysis was not powered to analyze this survival difference between subgroups. There was a significant improvement in the predefined secondary endpoints of biochemical PFS (bPFS; HR, 0.73 [95% CI, 0.56–0.94]; P = .014) and radiologic PFS (rPFS; HR, 0.75 [95% CI, 0.58–0.97]; P = .030) in the ADT-plus-docetaxel arm as compared with the ADT-alone arm.
The more recent Eastern Cooperative Oncology Group (ECOG) E3805 CHAARTED trial also evaluated the strategy of combining chemotherapy (docetaxel) with ADT in metastatic ADT-naive disease.[18] A total of 790 men with metastatic hormone-sensitive disease were randomized 1:1 between July 2006 and November 2012 to ADT plus docetaxel (at 75 mg/m2 every 3 weeks for 6 cycles) or ADT alone. After a median follow-up of 28.9 months, the primary endpoint of median OS was 13.6 months longer (57.6 vs 44 months) in the ADT-plus-docetaxel arm compared with the ADT-alone arm (HR, 0.61 [95% CI, 0.47–0.80]; P < .001). In a subset analysis, the biggest difference in OS between the two arms was 17 months; this occurred in the 65% of patients who had HVD: 49.2 months in the ADT-plus-docetaxel arm vs 32.2 months for the ADT-alone arm (HR, 0.60 [95% CI, 0.45–0.81]; P < .001). All secondary endpoints were significantly improved in the ADT-plus-docetaxel arm compared with the ADT-alone arm: median time to biochemical, symptomatic, or radiographic progression was 20.2 vs 11.7 months, respectively (HR, 0.61 [95% CI, 0.51–0.72]; P < .001); and the rate of prostate-specific antigen (PSA) level < 0.1 ng/mL was 27.7% vs 16.8%, respectively (P < .001).
These two studies differed in several respects, which accounted for the statistical differences in outcomes. The CHAARTED study was a larger study (N = 790), and almost twice as many patients had higher-volume and higher-grade disease (66% vs 22%) compared with patients in the GETUG-AFU 15 trial (N = 385). These differences are reflected in the OS in the ADT-alone arms of the two trials (44 vs 48.6 months). Although the GETUG-AFU 15 study did not show a greater OS benefit for docetaxel therapy compared with the CHAARTED trial, both studies showed significant improvement in both bPFS and rPFS.[17,18]
In STAMPEDE, a multi-stage, multi-arm, randomized controlled trial investigating the combination of ADT plus docetaxel in hormone-sensitive metastatic prostate cancer, survival data showed a statistically significant 27% reduction in risk of death in the ADT-plus-docetaxel arm compared with the ADT-alone arm (HR, 0.73 [95% CI, 0.59–0.89]; P = .002). Median OS was 65 months (95% CI, 27 months–not reported) vs 43 months (95% CI, 24–88 months) in the ADT-plus-docetaxel arm compared with the ADT-alone arm.[19]
A systematic review and meta-analysis incorporating data from these three phase III trials (GETUG-AFU 15, CHAARTED, and STAMPEDE) that evaluated chemohormonal therapy in hormone-sensitive metastatic prostate cancer were performed.[20] A total of 2,262 patients had metastatic disease (951 received ADT plus docetaxel; 1,311 received ADT alone). In metastatic prostate cancer, the addition of docetaxel was associated with improved OS (HR, 0.73 [95% CI, 0.60–0.90]; P = .002) and PFS (HR, 0.63 [95% CI, 0.57–0.70]; P < .001). No significant relatonship was demonstrated on subgroup analysis between the addition of docetaxel and presence of HVD or LVD (P = .5).
The efficacy of docetaxel in hormone-sensitive metastatic prostate cancer has not been clearly elucidated; however, the coexistence of androgen receptor (AR)-positive and AR-negative cells in metastatic disease underlies some of the biologic rationale for using the combined hormonal therapies and chemotherapies. In addition, docetaxel has been shown to affect AR trafficking in prostate cancer, and recent discoveries have also shown that androgen ablation controls DNA repair mechanisms in the disease.[21,22] From a clinical perspective, patients with hormone-sensitive disease are in generally better overall health and have better performance status compared with those patients with mCRPC, and thus are able to tolerate dose-intense chemotherapy successfully.[13,20]
Novel hormonal agents
The revelation that CRPC still depends on the key AR-mediated signaling and downstream gene activation for growth and progression led to the discovery of novel hormonal agents.
Abiraterone acetate is a potent cytochrome p450 17A1 (CYP17A1) inhibitor that suppresses androgen synthesis in the adrenals and testes when used to treat mCRPC. It is administered with steroids (prednisone or prednisolone, 5 mg twice per day) to suppress adrenocorticotropic hormone–induced mineralocorticoid excess. Abiraterone was approved in 2011 after two large trials, COU-AA-301 and COU-AA-302, confirmed its efficacy in docetaxel-treated and chemotherapy-naive patients, respectively. In the COU-AA-301 trial, 1,195 patients who had received up to two lines of chemotherapy with at least one docetaxel-based regimen were randomized to prednisone plus abiraterone vs prednisone plus placebo. The median OS for the abiraterone arm was significantly longer: 15.8 vs 11.2 months in the placebo group (HR, 0.74 [95% CI, 0.64–0.86]; P < .001). Abiraterone/prednisone improved pain control, quality of life, and fatigue, and delayed skeletal-related events (SREs).[23] In the COU-AA-302 trial, 1,088 chemotherapy-naive patients with mCRPC with rising PSA levels and minimal symptoms were randomized to prednisone plus abiraterone vs prednisone plus placebo. On final analysis (after a median of 49.4 months of follow-up), there was a significant improvement in median OS in the abiraterone arm of 34.7 vs 30.3 months (HR, 0.8 [95% CI, 0.69–0.83]; P < .001).Common toxicities included mineralocorticoid side effects of hypertension, edema, hypokalemia, and elevated levels on liver function tests.[24,25]
Enzalutamide is a potent second-generation selective AR antagonist that binds to the AR, decreases ligand-dependent nuclear translocation and binding of the AR to DNA, and blocks cellular proliferation. In the AFFIRM trial, 1,199 mCRPC patients who had received prior docetaxel chemotherapy were randomized 2:1 to enzalutamide or placebo. There was a 4.8-month improvement in median OS (18.4 vs 13.6 months) favoring the enzalutamide arm (HR, 0.631; P < .0001).[26] In the phase III PREVAIL study, 1,717 chemotherapy-naive patients with mCRPC (asymptomatic or mildly symptomatic metastatic disease that had progressed despite ADT) were randomized to enzalutamide or placebo. There was a significant improvement in rPFS (HR, 0.19 [95% CI, 0.15–0.23]; P < .001), as well as in median OS, estimated to be 32.4 months vs 30.2 months (HR, 0.7; P < .0001), favoring the enzalutamide arm.[27] The most common side effects observed were fatigue, diarrhea, and hot flashes. These results led to the approval of enzalutamide in both the pre- and post-docetaxel mCRPC settings.
Immunotherapy
Sipuleucel-T is a first-in-class active cellular immunotherapy based on a dendritic cell–based vaccine. Peripheral blood mononuclear cells are activated ex vivo with PA2024 recombinant fusion protein (prostatic acid phosphatase fused to granulocyte-macrophage colony-stimulating factor). In the phase III IMPACT trial, 512 patients were randomized to 3 infusions of sipuleucel-T over 6 weeks vs placebo. There was a 4.1-month improvement in OS (median, 25.8 vs 21.7 months; P = .03). There were no effects on PSA level or time to disease progression. Sipuleucel-T was found to be well-tolerated overall, with side effects related to infusion, such as flu-like symptoms and myalgia.[28]
Radiopharmaceuticals
Ra-223 dichloride is a targeted α-emitter that is selectively taken up at areas of increased bone turnover, emitting high-energy α-particles to induce targeted double-stranded DNA breaks. In the phase III ALSYMPCA trial, 921 mCRPC patients with two or more symptomatic bone metastases and no visceral metastases who were pretreated with or unfit for docetaxel were randomized to Ra-223 or placebo. Patients received 6 injections once every 4 weeks over 6 months. Ra-223 was well-tolerated and resulted in a 3.6-month improvement in OS (14.9 vs 11.3 months; HR, 0.70 [95% CI, 0.58–0.83]; P < .001). All grade 3 adverse events were lower in the Ra-223 arm. Reported side effects were myelosuppression, diarrhea, vomiting, and peripheral edema.[29]
Bone-targeted agents
Denosumab is a human monoclonal antibody against receptor activator of nuclear factor kappa-β ligand and inhibits osteoclast function. In a randomized trial of 1,904 patients with mCRPC, denosumab was superior to zoledronic acid in time to first SRE (median, 20.7 vs 17.1 months; HR, 0.82 [95% CI, 0.71–0.95]; P = .008); however, there was no difference in OS.[30] Both denosumab and zoledronic acid are approved for the prevention of SREs.[11,31]
AUA Guidelines in the Context of Current FDA Approvals
The management of men with castration-resistant disease is an evolving field. The relatively recent approvals of the aforementioned agents, including first- and second-line chemotherapy and immunotherapy agents that affect the androgen axis, as well as radionuclide therapy that improves OS, have been greeted with enthusiasm by patients and clinicians alike. However, these expanded treatment options provide challenges in terms of appropriateness of therapy, patient selection, and treatment sequencing. To aid clinicians in decision making, the American Urological Association (AUA) has developed guidelines for the management of CRPC.[32]
The AUA CRPC guidelines were developed based on the current understanding of the US Food and Drug Administration (FDA)-approved agents. These CRPC guidelines were the result of a multidisciplinary panel assembled by the AUA, using well-described evidence-based methodology. The CRPC guidelines were created with a strong emphasis on clinical application, utilizing common presenting characteristics, including the presence or absence of metastatic disease, degree of symptomatology, prior use of docetaxel chemotherapy, and patient performance status. The end result was the development of an algorithm of six index patients, with clinical guidelines based upon appropriateness of therapy and the strength of the supporting evidence. Since this is a rapidly evolving landscape, the challenge will be to update these guidelines as novel agents gain approval and new indications become approved for existing agents.

Ian M. Thompson, Jr, MD
DUT Health Science Center at San Antonio
San Antonio, TexasWhat Is New in the Treatment of Metastatic Castration-Resistant Prostate Cancer?With the publication of the updated 2015 Prostate Cancer Clinical Trials Working Group 3 (PCWG3) guidelines for metastatic castration-resistant prostate cancer (mCRPC), we see the explosion of knowledge and new treatments synthesized into a single document. Treatment has moved from 60 years of reliance on androgen deprivation therapy, to docetaxel, to a current host of agents with overlapping indications for use but with what seems to be an additive impact on survival. The field has moved from a monolithic approach to one metastatic prostate cancer, to pathologic subtypes that receive differing therapies, to a further explosion in molecular subtypes and an array of potential targets. Although small-cell tumors and tumors with neuroendocrine differentiation have been treated by incorporating cytotoxic chemotherapy, now the tumor can be analyzed in real-time, as soon as castration resistance or tumor progression is observed, which may allow for preemptive therapies, thus extending patient survival.What Information Is Included in the Updated Guidelines? The framework for studies of new agents in advanced prostate cancer is captured in the updated PCWG3 guidelines, which not only include traditional imaging and biomarkers, but also novel approaches such as liquid biopsies using circulating tumor cells, both in numbers of cells and molecular analyses of the cells themselves. Perhaps most importantly, the guidelines stress the patient-centric approach to this disease: Not only should overall survival be considered, but so should control of pain and prevention of potentially catastrophic events during disease progression.What Can We Expect in the Future?Yogi Berra was reported to have said, “It's tough to make predictions, especially about the future.” Perhaps I'm going out on a limb here, but I predict that the PCWG3 guidelines will likely require updating sooner than 7 years from now. In those guidelines we should have greater clarity about the sequencing of current and forthcoming agents and the selection of the optimal agent for a particular patient. However, with the host of new targets and their corresponding therapies, as novel drugs become available, this tsunami of options will likely continue to challenge us with the decision of which agent(s) for which patient.
Clinical and Molecular Subtypes of CRPC
Histologic and pathologic subtypes
A variety of prostate cancer morphologic subtypes have been previously described. The PCWG3 guidelines recommend distinguishing between adenocarcinoma and non-adenocarcinoma biologic subtypes, since this distinction has a great bearing on management stratification (Figure 2). Pure small-cell carcinoma of the prostate is rare (< 1%); however, focal neuroendocrine differentiation with adenocarcinoma is observed in 5% to 10% of cases. Neuroendocrine prostate cancer (NEPC) refers to a spectrum of lethal forms of prostate cancer, with patient survival between 1 and 2 years.[33,34] An updated classification schema of NEPC based on morphology describes small-cell carcinoma, large-cell NEPC, adenocarcinoma with Paneth cells (rare), carcinoid tumors (rare), and adenocarcinoma with neuroendocrine differentiation. Treatment-emergent NEPC can be observed at the development of resistance to ADT or during treatment with newer AR-signaling inhibitors. Immunohistochemical biomarkers such as induction of chromogranin A and synaptophysin, loss of AR and PSA expression, and upregulation of CD56 can help distinguish NEPC from adenocarcinoma. Though debated, a “transdifferentiation” cellular model is the most accepted explanation of the origin of NEPC, and has been demonstrated by AR knockdown.[34]
Clinically, small-cell carcinoma and NEPC are aggressive tumors and manifest with visceral or soft-tissue disease, predominant lytic bone metastasis, disproportionately low PSA levels relative to overall disease burden, and limited response to androgen axis modulation. Molecular analysis has shown that these tumors are characterized by loss of RB tumor suppressor copy number or expression, downregulation of REST (regulator of neuronal gene expression), amplification of AURKA and N-myc, upregulation of the histone deacetylase EZH2, and activation of the PI3-kinase pathway. Pure small-cell carcinoma is frequently treated with a platinum/etoposide combination. In prostate adenocarcinoma admixed with NEPC, it is reasonable to consider a trial of ADT with cytotoxic chemotherapy (docetaxel or a combination of carboplatin/docetaxel).[34]
The PCWG3 guidelines stress the importance of biologic profiling of the tumor at the initiation of any therapy by biopsies of metastatic sites, liquid biopsies such as circulating tumor cells (CTCs) or circulating DNA analysis, or other blood biomarkers of bone turnover or immune function.
Clinical subtypes based on patterns of spread
The five clinical subtypes initially described in the PCWG2 recommendations have been elaborated in the PCWG3 guidelines [7,14]:
• Locally recurrent or persistent disease in the prostate or prostate bed, with no evidence of metastasis on imaging.
• Nonmetastatic disease (M0): a rising PSA level, with no evidence of detectable disease on bone scan or chest/abdomen/pelvis CT.
• Nodal spread and no evident bone or visceral (liver, lung, adrenal, central nervous system) disease.
• Bone disease with or without nodal disease and no evident visceral spread.
• Visceral disease with or without spread to other sites.
Subtypes based on patterns of response to AR-signaling inhibitors
Analysis of post-therapy PSA level changes in patients treated with AR pathway modulators has revealed three response categories [14]:
• Sensitive disease: dramatic and durable decline in PSA level post-therapy.
• Partial sensitivity followed by acquired resistance: PSA level decline followed by slow rise.
• De novo resistance: a transient drop or no response followed by an immediate rise in PSA level.
Evolving molecular subtypes of mCRPC
Prostate cancer is a unique multifocal disease, with clonal subpopulations and varied histologic and molecular abnormalities. Heterogeneity exists both intra-patient and inter-patient, which accounts for the variability in therapeutic responses among patients with the same stage of prostate cancer.[4,5,35] The prostate cancer genome displays few chromosomal gains or losses (most commonly PTEN focal loss) and a low mutation rate. Other relevant genetic alterations include loss of NKX3.1 on chromosome 8p, RB1 on 13q14.2, TP53 on 17p31.1, and the interstitial deletion spanning ERG and TMPRSS2. Mutations in SPOP (encoding substrate binding unit of Cullin-based E3 ubiquitin ligase), TP53, MLL2, FOXA1, and AR have been described in CRPC.[36-39]
RB1 suppressor mutations are seen in 34% of primary prostate cancers and 74% of metastatic prostate cancers. Loss of RB1 function may be linked to castration resistance by activation of AR signaling via unsuppressed E2F transcription factors. Cyclin-dependent kinase inhibitors could enhance AR suppression in RB-positive tumors, while radiotherapy or DNA-damaging agents could be effective in tumors with RB loss. P53 (17p31) alterations are associated with recurrences after radiation, androgen suppression, and reduced docetaxel-induced apoptosis.[38,39]
Genomic studies have shown distinct subclasses of tumors based on E26 transformation-specific gene fusions. ETS fusion–positive cancers have fusions of the 5' untranslated region of an androgen-regulated gene (eg, TMPRSS2) to almost the entire transcription sequence of an ETS transcription family member (eg, ERG, which accounts for ~90% of all fusions). Other non-ERG ETS genes include ETV1, ETV4, ETV5, and FLI1, and comprise approximately 10% of fusions. About 50% to 60% of PSA-screened prostate cancer foci in Caucasian men harbor these fusions. The presence of ERG rearrangements has shown higher response rates to abiraterone. ETS fusion–negative cancers can harbor deletion of CHD1 in 5q21 (10%–17%) and/or mutations in SPOP (5%–10%), and/or can overexpress SPINK1 (10%).[36,37]
A recent multi-institutional effort (Stand Up To Cancer/Prostate Cancer Foundation) analyzed integrative clinical genomics of advanced prostate cancer by prospective whole-exome and transcriptome sequencing of bone and soft-tissue tumor biopsies from a cohort of 150 mCRPC patients. The study showed that approximately 90% of mCRPC cases harbor actionable mutations. Aberrations in AR and ETS genes, TP53, and PTEN were frequent (40%–60%). Novel genomic alterations in PIK3CA/B, R-spondin, BRAF/RAF1, APC, β-catenin, and ZBTB16/PLZF were identified. Aberrations in DNA repair genes such as BRCA1, BRCA2, and ATM were observed at substantially higher frequencies (19.3%) compared with primary prostate cancer. These study findings demonstrate the potential for patient-specific targeted precision medicine in mCRPC.[40,41]
Mechanisms of Resistance to Hormonal Therapy and Chemotherapy
The AR gene is located on chromosome Xq11-12; AR is a 110-kDa nuclear protein that binds to a specific hormone response element called androgen response element (ARE). AR is made of different domains: the N-terminal domain, DNA-binding domain, hinge region, and ligand-binding domain (LBD).[42] CRPC remains addicted to AR signaling; driving mechanisms include AR gene mutations, AR gene overexpression, AR splice variants, and increased expression of transcriptional coactivators. Intraprostatic androgen synthesis (autocrine) can be a significant source of androgen synthesis under androgen inhibition therapy.[43-45]
Primary resistance to abiraterone or enzalutamide is generally defined as radiographic progression within 3 months of therapy and is reported to be less than 10% in chemotherapy-naive mCRPC patients and 20% to 40% in patients pretreated with chemotherapy. Mechanisms of acquired and primary resistance include systemic and intratumoral androgen biosynthesis upregulation, AR gene mutations and amplifications, crosstalk with outlaw pathways, glucocorticoid receptor overexpression, neuroendocrine differentiation, autophagy induction, and immune evasion.[44,46-48] The F876L point mutation in AR confers resistance to enzalutamide.[49] Parallel pathways implicated in acquired resistance to newer hormonal agents include the epidermal growth factor receptor, Src, and PI3K/AKT/mammalian target of rapamycin (mTOR) pathways.[4,36]
In preclinical models, constitutive activation of AR can occur in the absence of ligand, with AR splice variants lacking the LBD. The most commonly expressed variants that drive prostate cancer under ADT are AR-V7 and AR-V567. In an analysis of 31 enzalutamide-treated and 31 abiraterone-treated mCRPC patients, 39% and 19%, respectively, had AR-V7 detected in CTCs. AR-V7–positive patients had lower PSA response rates than AR-V7–negative patients in both the enzalutamide-treated (0% vs 53%; P = .004) and abiraterone-treated (0% vs 68%; P = .004) groups. AR-V7–positive patients had a significantly lower mean clinical or radiographic PFS in both the enzalutamide-treated (2.1 vs 6.1 months; P < .001) and abiraterone-treated (2.3 months vs not reached; P < .001) groups. AR-V7 was present in 9% to 15% of treatment-naive patients but increased during treatment with abiraterone (55%) and enzalutamide (50%), supporting its role in intrinsic and acquired resistance to these agents.[50]
Taxanes are the major chemotherapeutic agents for treatment of patients with mCRPC. Docetaxel targets the cytoskeleton by stabilizing the interaction of β-tubulin subunits of microtubules, preventing depolymerization, and inducing G2/M arrest and apoptosis. It also targets the AR-signaling axis by blocking the nuclear translocation of AR, implicating cross-resistance between docetaxel and antiandrogen therapies.[21] The second-generation taxane cabazitaxel exerts stronger cytotoxic and cytostatic responses compared with docetaxel, and also reduces overall AR levels and FOXO1 expression. de Leeuw and colleagues have shown distinct molecular actions of cabazitaxel vs docetaxel via gene expression profiling.[22] In addition, tumors with a loss of RB1 showed enhanced sensitivity to cabazitaxel. RB1 could thus be the first potential biomarker predicting sensitivity to taxanes in CRPC. The reported molecular mechanisms leading to taxane resistance include increased drug efflux by ATP-binding cassette (ABC) transporters, mutational alterations in tubulin subunits, altered microtubule dynamics, increased expression of anti-apoptotic proteins, and the epithelial-to-mesenchymal transition (EMT) programming in mCRPC.[21] Data from the CABARESC study have shown that the efficacy of cabazitaxel is sustained even in the presence of AR-V7 and after prior administration of hormonal therapies, making it a potent second- and third-line option for mCRPC.[51,52]
PCWG3 Recommendation Updates
The key goals of the PCWG3 recommendations are as follows: (1) to update the framework for clinical trial conduct so as to aid in defining eligibility criteria, using validated biomarkers to enrich patient selection in clinical trial enrollment; (2) to design better interventions to aid in rational drug discovery; and (3) to create novel combination strategies to maximize patient benefit. The key highlights of the evolution of the PCWG3 guidelines from its predecessor are discussed in Table 1.[7-9,14]
In Table 2 we summarize the current FDA-approved agents for the management of CRPC guided by the PCWG3 clinical outcome framework.[14]
Emerging molecular targets and clinical trial design
The optimal sequence for employing current treatment strategies in mCRPC is uncertain, and no treatment-guiding biomarkers have been defined.[11,12] Improving patient outcomes by testing currently available drugs in combination strategies is being explored. Targeting the AR-signaling pathway beyond abiraterone and enzalutamide is an area of active research.[53] Novel CYP17 inhibitors such as galeterone (TOK-001) and VT-464, and AR inhibitors such as ARN-509 and ODM-201, are being tested in clinical trials. EPI-001 is a unique AR antagonist that inhibits the amino-terminus domain of the AR protein and may overcome resistance mediated by splice variants and AR mutations.[47]
The poly-(adenosine diphosphate) [ADP]-ribose polymerases (PARPs) are a family of about 17 multifunctional enzymes, with PARP1 being the most abundant. PARP-1 is an enzyme involved in base excision repair in response to DNA damage, enabling single-strand break repair. Inhibition of PARP causes DNA single-stranded breaks and accumulation of double-stranded breaks at replication forks. These breaks are normally repaired by the homologous-recombination DNA double-stranded repair pathway, key members of which are tumor-suppressor proteins BRCA1 and BRCA2. In patients with DNA repair gene defects, such as BRCA mutations, PARP inhibition can lead to “synthetic lethality,” causing selective tumor cell cytotoxicity that spares normal cells.[54] As described earlier, mCRPC can harbor genomic aberrations interfering with DNA repair.[40] A phase II trial of the PARP inhibitor olaparib in 50 heavily pretreated mCRPC patients showed promising results. Sixteen (33%) of 49 patients had a response to the drug based on a composite endpoint. Next-generation sequencing identified homozygous deletions, mutations, or both in DNA repair genes, including BRCA1/2, FA (Fanconi anemia) genes, and CHEK2 in 16 (33%) patients. Of these patients, 14 (88%) had a response to olaparib, including all 7 patients with BRCA2 mutations.[55]
Other pathways and receptors being targeted in clinical trials for mCRPC include the PI3K/AKT/mTOR pathway, c-Met (cabozantinib), insulin-like growth factor 1, Src-kinase, heat shock proteins (HSP27, HSP90), and clusterin chaperones and angiogenesis pathways. Ongoing phase II studies are evaluating AURKA inhibitors in metastatic NEPC.[36,37,44] Immune modulation with vaccines (PROSTVAC), checkpoint inhibition (ipilimumab), and combination strategies are also being evaluated in mCRPC clinical trials.[56]
Conclusion and Future Directions
Despite major strides in unraveling the biology of mCRPC and the advent of new therapies, the disease still remains a fatal diagnosis. Collaboration between multiple institutions and cooperative groups is aimed at a comprehensive molecular classification of the disease. The search for ideal biomarkers has led to CTC analysis as an initial real-time disease marker, and ongoing research should standardize more biomarker platforms and prognostic models into routine practice. The PCWG3 guidelines will be an added thrust to the coordination of rational clinical trial design in this highly heterogeneous disease, enabling novel discoveries and clarifying sequential treatment strategies that will improve patient outcomes in the future.
Financial Disclosure:Dr. Kelly receives research support from Sanofi-Aventis; he also serves on the advisory board of Churchill Pharmaceuticals.
References:
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5-29.
2. Huggins C, Hodges CV. Studies on prostatic cancer. I. The effect of castration, of estrogen and androgen injection on serum phosphatases in metastatic carcinoma of the prostate. CA Cancer J Clin. 1972;22:232-240.
3. Attard G, Parker C, Eeles RA, et al. Prostate cancer. Lancet 2015 Jun 11. pii: S0140-6736(14)61947-4. [Epub ahead of print]
4. Katsogiannou M, Ziouziou H, Karaki S, et al. The hallmarks of castration-resistant prostate cancers. Cancer Treat Rev. 2015;41:588-597.
5. Lian F, Sharma NV, Moran JD, Moreno CS. The biology of castration-resistant prostate cancer. Curr Probl Cancer. 2015;39:17-28.
6. Tannock IF, de Wit R, Berry WR, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502-12.
7. Scher HI, Halabi S, Tannock I, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26:1148-59.
8. Scher HI. Building on Prostate Cancer Working Group 2 to change the paradigm from palliation to cure. Am Soc Clin Oncol Educ Book. 2014:e204-e212.
9. Scher HI, Morris MJ, Basch E, Heller G. End points and outcomes in castration-resistant prostate cancer: from clinical trials to clinical practice. J Clin Oncol. 2011;29:3695-704.
10. Bahl A, Masson S, Birtle A, et al. Second-line treatment options in metastatic castration-resistant prostate cancer: a comparison of key trials with recently approved agents. Cancer Treat Rev. 2014;40:170-77.
11. Lorente D, Mateo J, Perez-Lopez R, et al. Sequencing of agents in castration-resistant prostate cancer. Lancet Oncol. 2015;16:e279-e292.
12. Maines F, Caffo O, Veccia A, et al. Sequencing new agents after docetaxel in patients with metastatic castration-resistant prostate cancer. Crit Rev Oncol Hematol. 2015; 96:498-506.
13. Valenca LB, Sweeney CJ, Pomerantz MM. Sequencing current therapies in the treatment of metastatic prostate cancer. Cancer Treat Rev. 2015;41:332-40.
14. Scher HI, Morris MJ, Stadler WM, et al. The Prostate Cancer Working Grouyp 3 (PCWG3) consensus for trials in castrate resistant prostate cancer (CRPC). J Clin Oncol. 2015; 33(suppl): abstr 5000.
15. Berthold DR, Pond GR, Soban F, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer: updated survival in the TAX 327 study. J Clin Oncol. 2008;26:242-45.
16. de Bono JS, Oudard S, Ozguroglu M, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147-54.
17. Gravis G, Boher JM, Joly F, et al. Androgen deprivation therapy (ADT) plus docetaxel versus ADT alone in metastatic non castrate prostate cancer: impact of metastatic burden and long-term survival analysis of the randomized phase 3 GETUG-AFU15 trial. Eur Urol. 2015 Nov 20. pii:S0302-2838(15)01103-3. [Epub ahead of print]
18. Sweeney CJ, Chen YH, Carducci M, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373:737-46.
19. James ND, Sydes MR, Mason MD, et al. Docetaxel and/or zoledronic acid for hormone-naïve prostate cancer: first overall survival results from STAMPEDE (NCT00268476) [abstract 5001]. J Clin Oncol. 2015;33(suppl): abstr 5001.
20. Tucci M, Bertaglia V, Vignani F, et al. Addition of docetaxel to androgen deprivation therapy for patients with hormone-sensitive metastatic prostate cancer: a systematic review and meta-analysis. Eur Urol. 2015 Sep 25. pii: S0302-2838(15)00907-0. [Epub ahead of print]
21. Martin SK, Kyprianou N. Exploitation of the androgen receptor to overcome taxane resistance in advanced prostate cancer. Adv Cancer Res. 2015;127:123-58.
22. de Leeuw R, Berman-Booty LD, Knudsen KE, et al. Novel actions of next-generation taxanes benefit advanced stages of prostate cancer. Clin Cancer Res. 2015;21:795-807.
23. de Bono JS, Logothetis CJ, Molina A, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 2011;364:1995-2005.
24. Ryan CJ, Smith MR, de Bono JS, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med 2013;368:138-48.
25. Ryan CJ, Smith MR, Fizazi K, et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2015;16:152-60.
26. Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187-97.
27. Beer TM, Armstrong AJ, Rathkopf DE, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424-33.
28. Kantoff PW, Higano CS, Shore ND, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411-22.
29. Parker C, Nilsson S, Heinrich D, et al; ALSYMPCA Investigators. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369:213-23.
30. Smith MR, Saad F, Coleman R, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trial. Lancet. 2012;379:39-46.
31. Crawford ED, Higano CS, Shore ND, et al. Treating patients with metastatic castration resistant prostate cancer: a comprehensive review of available therapies. J Urol. 2015; 194:1537-47.
32. Cookson MS, Lowrance WT, Murad MH, Kibel AS; American Urological Association. Castration-resistant prostate cancer: AUA guideline amendment. J Urol. 2015;193:491-9.
33. Aggarwal R, Zhang T, Small EJ, Armstrong AJ. Neuroendocrine prostate cancer: subtypes, biology, and clinical outcomes. J Natl Compr Canc Netw. 2014;12:719-26.
34. Beltran H, Tomlins S, Aparicio A, et al. Aggressive variants of castration-resistant prostate cancer. Clin Cancer Res. 2014;20:2846-50.
35. Tomlins SA, Alshalalfa M, Davicioni E, et al. Characterization of 1577 primary prostate cancers reveals novel biological and clinicopathologic insights into molecular subtypes. Eur Urol. 2015;68:555-67.
36. Grasso CS, Wu YM, Robinson DR, et al. The mutational landscape of lethal castration-resistant prostate cancer. Nature. 2012;487:239-43.
37. Gundem G, Van Loo P, Kremeyer B, et al. The evolutionary history of lethal metastatic prostate cancer. Nature. 2015;520:353-7.
38. Lorente D, De Bono JS. Molecular alterations and emerging targets in castration resistant prostate cancer. Eur J Cancer. 2014;50:753-64.
39. Rodrigues DN, Butler LM, Estelles DL, de Bono JS. Molecular pathology and prostate cancer therapeutics: from biology to bedside. J Pathol. 2014;232:178-84.
40. Robinson D, Van Allen EM, Wu YM, et al. Integrative clinical genomics of advanced prostate cancer. Cell. 2015;161:1215-28.
41. Fraser M, Berlin A, Bristow RG, van der Kwast T. Genomic, pathological, and clinical heterogeneity as drivers of personalized medicine in prostate cancer. Urol Oncol. 2015; 33:85-94.
42. Tan MH, Li J, Xu HE, et al. Androgen receptor: structure, role in prostate cancer and drug discovery. Acta Pharmacol Sin. 2015;36:3-23.
43. Augello MA, Den RB, Knudsen KE. AR function in promoting metastatic prostate cancer. Cancer Metastasis Rev. 2014;33:399-411.
44. Yuan X, Cai C, Chen S, et al. Androgen receptor functions in castration-resistant prostate cancer and mechanisms of resistance to new agents targeting the androgen axis. Oncogene. 2014;33:2815-25.
45. Kahn B, Collazo J, Kyprianou N. Androgen receptor as a driver of therapeutic resistance in advanced prostate cancer. Int J Biol Sci. 2014;10:588-95.
46. Buttigliero C, Tucci M, Bertaglia V, et al. Understanding and overcoming the mechanisms of primary and acquired resistance to abiraterone and enzalutamide in castration resistant prostate cancer. Cancer Treat Rev. 2015;41:884-92.
47. De Maeseneer DJ, Van Praet C, Lumen N, Rottey S. Battling resistance mechanisms in antihormonal prostate cancer treatment: Novel agents and combinations. Urol Oncol. 2015;33:310-21.
48. Loriot Y, Eymard JC, Patrikidou A, et al. Prior long response to androgen deprivation predicts response to next-generation androgen receptor axis targeted drugs in castration resistant prostate cancer. Eur J Cancer. 2015;51:1946-52.
49. Azad AA, Volik SV, Wyatt AW, et al. Androgen receptor gene aberrations in circulating cell-free DNA: biomarkers of therapeutic resistance in castration-resistant prostate cancer. Clin Cancer Res. 2015;21:2315-24.
50. Antonarakis ES, Lu C, Wang H, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N Engl J Med. 2014;371:1028-38.
51. Onstenk W, Sieuwerts AM, Kraan J, et al. Efficacy of cabazitaxel in castration-resistant prostate cancer is independent of the presence of AR-V7 in circulating tumor cells. Eur Urol. 2015;68:939-45.
52. van Soest RJ, Nieuweboer AJ, de Morree ES, et al. The influence of prior novel androgen receptor targeted therapy on the efficacy of cabazitaxel in men with metastatic castration-resistant prostate cancer. Eur J Cancer. 2015 Aug 13. pii:S0959-8049(15)00743-1. [Epub ahead of print]
53. Bambury RM, Rathkopf DE. Novel and next-generation androgen receptor-directed therapies for prostate cancer: beyond abiraterone and enzalutamide. Urol Oncol. 2015 Jul 7. pii: S1078-1439(15)00269-0. [Epub ahead of print]
54. Brenner JC, Ateeq B, Li Y, et al. Mechanistic rationale for inhibition of poly(ADP-ribose) polymerase in ETS gene fusion-positive prostate cancer. Cancer Cell. 2011;19:664-78.
55. Mateo J, Carreira S, Sandhu S, et al. DNA-repair defects and olaparib in metastatic prostate cancer. N Engl J Med. 2015;373:1697-1708.
56. Saad F, Miller K. Current and emerging immunotherapies for castration-resistant prostate cancer. Urology. 2015;85:976-86.