FDA Receives BLA for Obe-cel in R/R Acute Lymphoblastic Leukemia
Data from the phase 2 FELIX study support the biologics license application for obecabtagene autoleucel as a treatment for patients with relapsed/refractory acute lymphoblastic leukemia.
Supporting data for the BLA came from the phase 1b/2 FELIX study (NCT04404660), which investigators originally presented at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting.
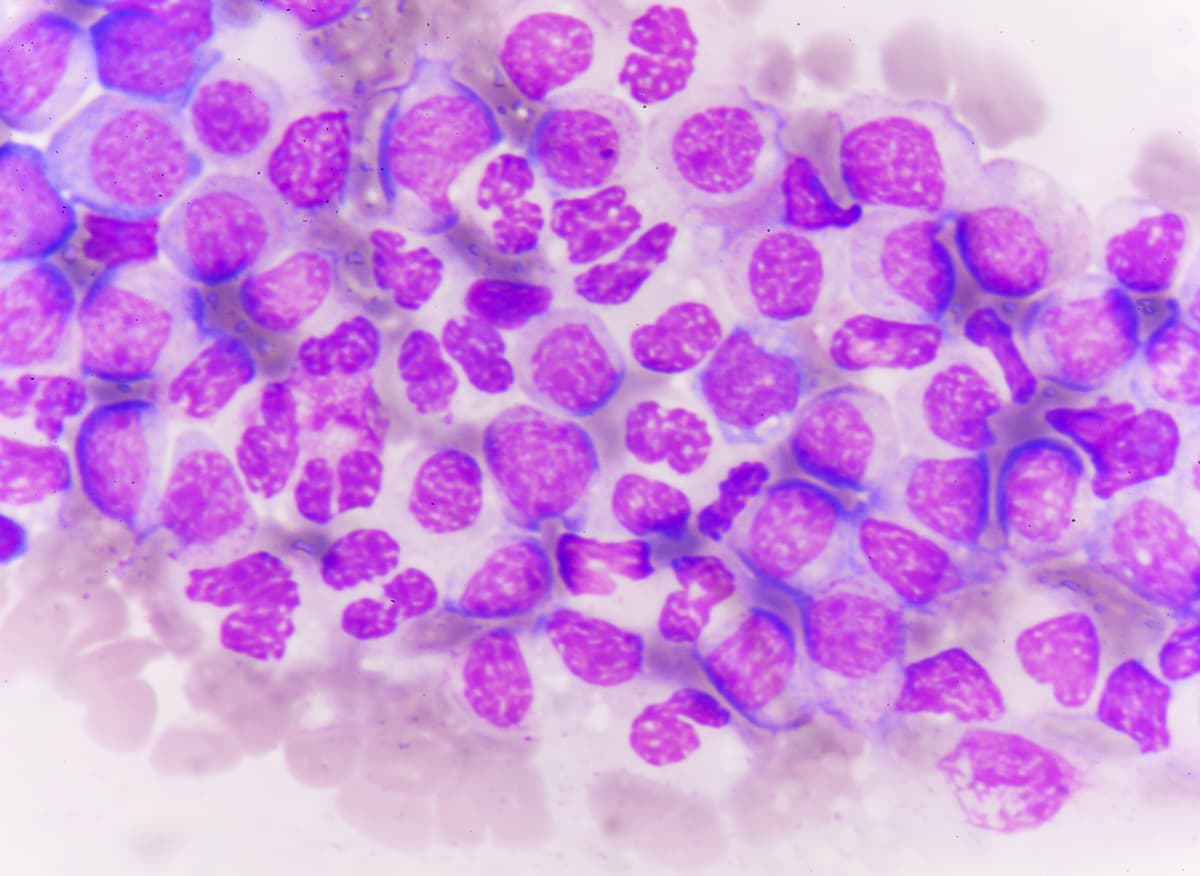
Developers have submitted a biologics license application (BLA) to the FDA in support of obecabtagene autoleucel (obe-cel; AUTO1) as a treatment for adult patients with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL), according to a press release from Autolus Therapeutics.1
The investigational CD19-targeting CAR T-cell therapy was designed with a rapid binding off-rate to prevent T cells from excessively activating. It is believed that the quick off-rate profile of obe-cel may limit T cell exhaustion and toxicity, thereby producing enduring responses in patients with relapsed/refractory ALL.
“We are looking forward to continuing working with the FDA through the regulatory approval process,” Christian Itin, PhD, chief executive officer at Autolus, said in the press release. “I would like to thank the treating physicians, patients, caregivers, and the dedicated team at Autolus for their support, trust and commitment for the program to reach this important milestone.”
Supporting data for the BLA came from the phase 1b/2 FELIX study (NCT04404660), which investigators originally presented at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting.
Of 94 patients who received an infusion, 54.3% achieved a complete response (CR), and 21.3% had a CR with incomplete count recovery (CRi).2 Investigators reported an objective response rate (ORR) of 76% (95% CI, 66%-84%; P <.0001). Overall, 97% of patients with a response and evaluable samples achieved minimal residual disease (MRD) negativity at the 10–4 level based on flow cytometry.
Any-grade and grade 3/4 cytokine release syndrome affected 75.5% and 3.2% of patients who underwent infusion, respectively. Moreover, 25.5% and 7.4% of patients experienced any-grade and grade 3/4 immune effector cell-associated neurotoxicity syndrome, respectively.
In the FELIX trial, patients underwent pre-conditioning chemotherapy with cyclophosphamide plus fludarabine followed by obe-cel at a target dose of 410 x 106 CAR T cells as a split dose on day 1 and day 10.
The trial’s primary end points included frequency of adverse effects (AEs) and serious AEs in phase 1b and ORR in phase 2. Secondary end points included the CR rate, duration of remission, progression-free survival, and incidence and duration of severe hypogammaglobulinemia.
Patients 18 years and older with relapsed/refractory B-cell ALL, an ECOG performance status of 0 or 1, and documented CD19 positivity within 1 month of screening were able to enroll ion the trial. Additional eligibility criteria included having adequate renal, pulmonary, hepatic, and cardiac function. To enroll in the primary cohort IIA in the phase 2 portion of the trial, patients needed to have at least 5% blasts in bone marrow at screening.
Those who were diagnosed with Burkitt’s leukemia/lymphoma or had a history or presence of clinically relevant central nervous system pathology were unable to enroll on the trial. Patients were also unsuitable for enrollment if they had uncontrolled fungal, bacterial, or viral infections that needed to be managed with systemic antimicrobials; active or latent Hepatitis B virus or active Hepatitis C virus; or previous CD19-targeting therapy not including blinatumomab (Blincyto).
References
- Autolus Therapeutics submits biologics license application to U.S. Food and Drug Administration for obecabtagene autoleucel (obe-cel) for patients with relapsed/refractory (r/r) adult B-cell acute lymphoblastic leukemia (ALL). News release. Autolus Therapeutics. November 27, 2023. Accessed November 27, 2023. https://shorturl.at/nzIJY
- Roddie C, Sandhu KS, Tholouli E, et al. Safety and efficacy of obecabtagene autoleucel (obe-cel, AUTO1), a fast-off rate CD19 CAR, in relapsed/refractory adult B-cell acute lymphoblastic leukemia (r/r B-ALL): Top line results of the pivotal FELIX study. J Clin Oncol. 2023;41(suppl 16):7000. doi:10.1200/JCO.2023.41.16_suppl.7000