FDA Accepts sNDA for Decitabine/Cedazuridine Combo in Newly Diagnosed AML
A PDUFA date for decitabine/cedazuridine and venetoclax in newly diagnosed AML has been set for February 25, 2026.
A PDUFA date for decitabine/cedazuridine and venetoclax in newly diagnosed AML has been set for February 25, 2026.
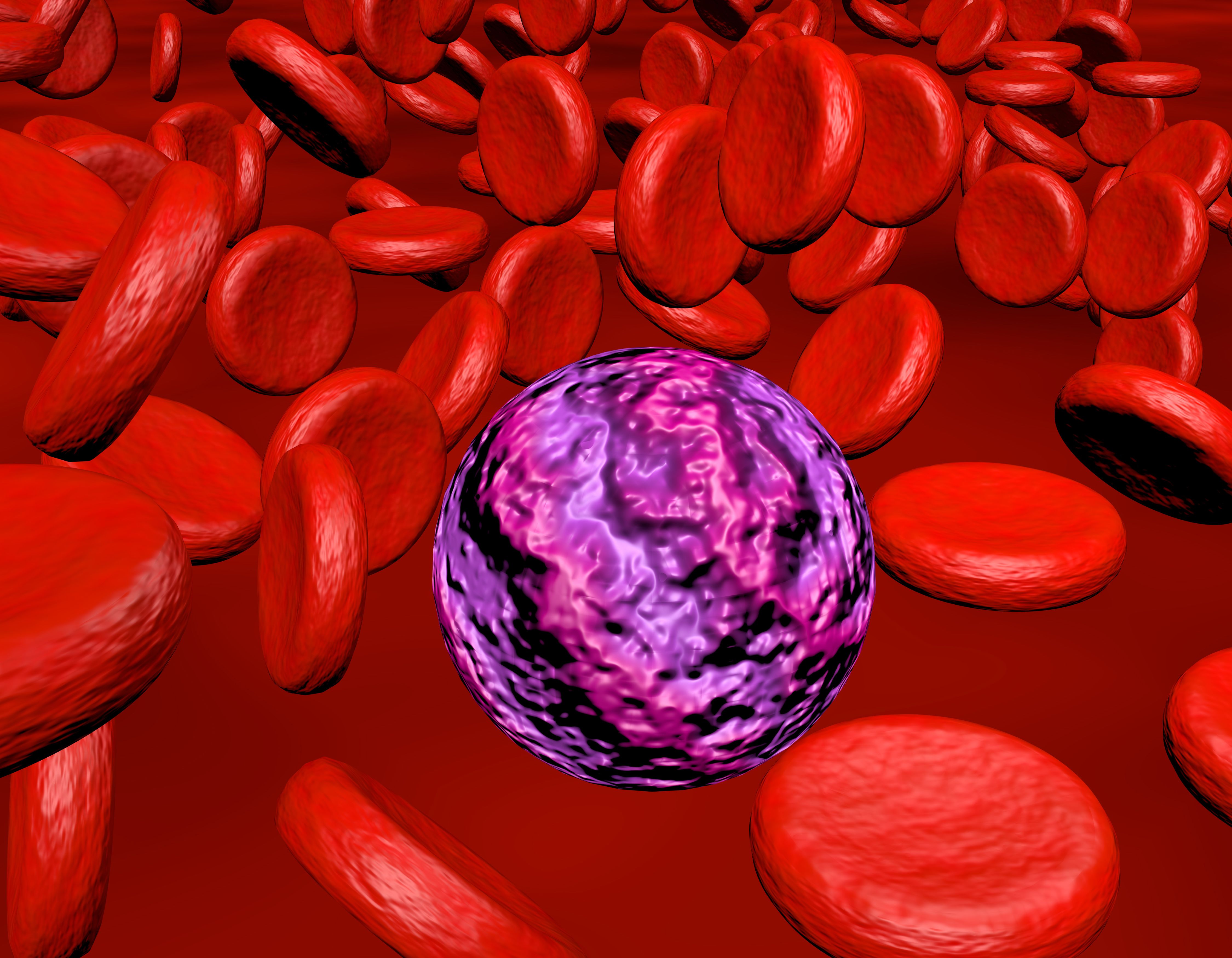
A supplemental new drug application (sNDA) has been accepted by the FDA for decitabine and cedazuridine (Inqovi) plus venetoclax (Venclexta) for patients with newly diagnosed acute myeloid leukemia (AML) who are ineligible for intensive induction chemotherapy, according to a press release from Taiho Oncology.1
The Prescription Drug User Fee Act Date has been set for February 25, 2026.
Supporting results for the sNDA were based on the phase 2b ASCERTAIN-V (ASTX727-07) trial (NCT04975919), which were presented at the European Hematology Association 2025 Congress.2
"We have an unwavering dedication to developing innovative new cancer treatments, and the FDA's acceptance of our sNDA for [decitabine and cedazuridine] in combination with venetoclax highlights the need for novel approaches in AML," said Harold Keer, MD, PhD, chief medical officer at Taiho Oncology. "If approved for patients with AML who are not eligible to undergo intensive induction chemotherapy, [decitabine and cedazuridine] in combination with venetoclax would offer the first all-oral alternative to current therapies."
A total of 101 patients were enrolled in the phase 2b portion of the study. On cycle 1, day 1, patients were given decitabine/cedazuridine plus venetoclax at 100 mg; on day 2, it was 200 mg; on days 3 to 5, it was 400 mg; and on days 6 to 28, venetoclax at 400 mg was given. For cycle 2 and beyond, decitabine/cedazuridine and venetoclax were given at 400 mg on days 1 to 5 and on days 6 to 28, venetoclax was given at 400 mg.
The primary end point in the phase 2b trial was complete response (CR) rate based on European Leukemia Net (ELN) 2017 criteria. The secondary end point was the effect of venetoclax on decitabine and cedazuridine in cycles 1 to 3, CR with incomplete hematologic recovery (CRi), CR with partial hematologic recovery (CRh), overall survival (OS), duration of response, and safety.
The median patient age was 78 years, 81.2% of patients were 75 years or older, 60.4% of patients were male, and 51.5% had an ECOG performance status of 1. ELN 2017 classification showed that 31.7% had favorable status, 33.7% had intermediate status, and 29.7% had adverse status. The most common mutation at baseline was TP53 in 16.8% of patients.
The CR rate was 46.5% (95% CI, 36.5%-56.7%), with a CRi rate of 16.8%, CRh rate of 5.0%, a CR plus CRi rate of 63.4% (95% CI, 53.2%-72.7%), a CR plus CRh rate of 51.5% (95% CI, 41.3%-61.6%), and a CR plus CRi and CRh rate of 63.4% (95% CI, 53.2%-72.7%). The median time to a CR was 2.4 months (95% CI, 0.7-15.3). A total of 80.0% (95% CI, 63.9%-89.5%) had a CR continuing at 9 months, and the median duration of follow-up was 11.2 months.
The median OS was 15.5 months (95% CI, 7.6-not evaluable [NE]). Additionally, 49 patients who experienced a CR/CRh/CRi had minimal residual disease (MRD) evaluated through local multiparameter flow cytometry. Of note, 55.1% achieved MRD negativity at any time, the median OS for those with MRD negativity was NE (95% CI, 12.1-NE), and the median OS for those with MRD positivity was 15.5 months (95% CI, 7.4-NE).
A median of 4 cycles was completed in the phase 2b arm, and 31.7% of investigators performed bone marrow examination. When looking at results from phase 1 to phase 2b, investigators found a decrease in mean dosing days for venetoclax and decitabine/cedazuridine starting with cycle 1 of 27.3 days and 5.0 days in phase 1 to 23.9 days and 5.0 days in phase 2b, respectively. For cycle 3, results showed 18.8 days and 4.9 days for phase 1 and 17.5 days and 4.4 days for phase 2b.
Regarding safety, 99.0% of patients experienced any-grade adverse effects (AEs), 80.2% had treatment-related AEs (TRAEs), 84.2% had serious AEs, 35.6% had serious TRAEs, 98.0% had grade 3 or higher AEs, and 72.3% had grade 3 or higher TRAEs.
AEs leading to treatment discontinuation occurred in 8.9% of patients, treatment interruption in 68.3%, dose reduction in 13.9%, and death in 15.8%.
References
- Taiho Oncology and Taiho Pharmaceutical announce U.S. FDA acceptance of supplemental new drug application for INQOVI in combination with venetoclax to treat patients with acute myeloid leukemia. News release. Taiho Oncology. July 9, 2025. Accessed July 10, 2025. https://tinyurl.com/mrxuh9st
- Roboz GJ, Zeidan AM, Mannis GN, et al. All-oral decitabine-cedazuridine (DEC-C) + venetoclax (VEN) in patients with newly diagnosed acute myeloid leukemia (AML) ineligible for induction chemotherapy: phase 1/2 clinical trial results. Abstract presented at: European Hematology Association 2025 Congress; June 12-15, 2025; Milan, Italy. Abstract S135.