FDA Grants Orphan Drug Designation to Tirabrutinib in Primary CNS Lymphoma
Investigators are assessing tirabrutinib, which received orphan drug designation from the FDA, as a treatment for patients with relapsed or refractory primary central nervous system lymphoma in the phase 2 PROSPECT study.
The FDA has granted orphan drug designation to tirabrutinib (ONO-4059) as therapy for patients with primary central nervous system lymphoma (PCNSL), according to a press release from ONO PHARMA USA.1
"We are extremely pleased that tirabrutinib has been granted orphan drug status for the treatment of PCNSL," according to the manufacturers of tirabrutinib.
Tirabrutinib is currently under investigation as a treatment for adult patients with newly diagnosed and relapsed or refractory PCNSL in the phase 2 PROSPECT study (NCT04947319). Tirabrutinib is a highly potent, selective Bruton tyrosine kinase (BTK) inhibitor regulating cellular proliferation and activation through the B-cell receptor, thereby enabling survival, differentiation, and clonal expansion of B-cells.
“We are extremely pleased that tirabrutinib has been granted orphan drug status for the treatment of PCNSL,” Kunihiko Ito, MBA, president and chief executive officer of ONO PHARMA USA, said in the press release. “Currently, ONO is carrying out a phase 2 trial of tirabrutinib in [patients] with newly diagnosed or relapsed/refractory PCNSL, and we look forward to advancing clinical trials so that patients may have therapeutic options as soon as possible.”
In part A of the phase 2 PROSPECT trial, patients with relapsed or refractory PCSNL will receive 480 mg of tirabrutinib monotherapy orally once a day. In part B of the trial, patients are assigned to one of 2 experimental cohorts. Patients will receive 320 mg or 480 mg of tirabrutinib taken orally once a day plus methotrexate, temozolomide (Temodar), and rituximab (Rituxan; MTR), or rituximab plus methotrexate, procarbazine, and vincristine (R-MPV) for 4, 28-day induction cycles or until disease progression.
Primary end points of the PROSPECT study include overall response rate, the incidence and severity of adverse effects (AEs) and serious AEs, and complete response rate. Secondary end points include duration of response, time to response, best overall response, change in corticosteroid doses, and pharmacokinetics.
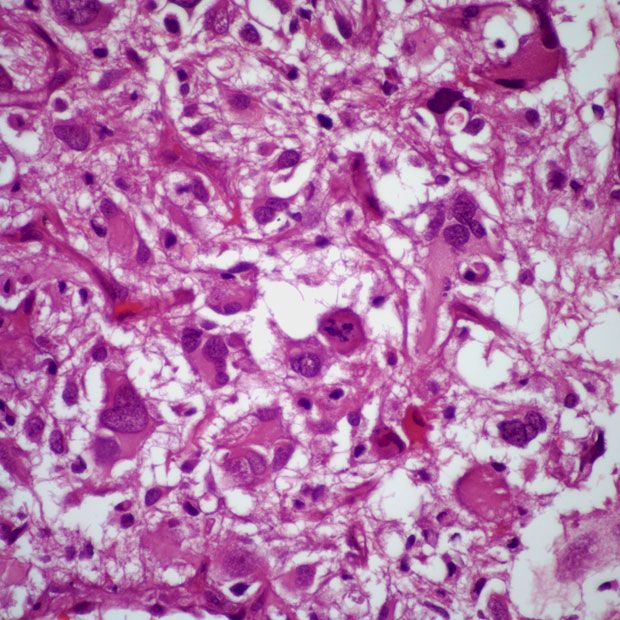
Patients 18 years and older are eligible for enrollment on the trial if they have a pathologic diagnosis of PCNSL, a measurable brain lesion with a minimum diameter larger than 1.0 cm, and an ECOG performance status of 0 to 2. Additional eligibility criteria include having a life expectancy of at least 6 months and adequate bone marrow, renal, and hepatic function.
Patients who have intraocular PCNSL with no brain lesion or intolerance of contrast-enhanced MRI due to allergic reactions to contrast agents are unable to enroll in the trial. Patients are also unsuitable for enrollment if they have a systemic presence of lymphoma, received prior BTK inhibitor treatment, an active malignancy other than PCNSL requiring systemic therapy, or a history of moderate to severe hepatic impairment.
In March 2020, the agent received approval in Japan for the treatment of patients with recurrent or refractory PCNSL in March 2020.2
References
- ONO PHARMA USA's tirabrutinib receives orphan drug designation from the FDA for the treatment of primary central nervous system lymphoma. News release. ONO PHARMA USA. March 23, 2023. Accessed March 27, 2023. prn.to/3zbnCZG
- ONO receives a manufacturing and marketing approval for Velexbru® tablet 80mg, a BTK inhibitor, for treatment of recurrent or refractory primary central nervous system lymphoma in Japan. News release. Ono Pharmaceutical Co., Ltd. March 25, 2020. Accessed March 27, 2023. bit.ly/42Hh2HR