FOLFOX Plus Ramucirumab Fails to Improve PFS in Gastric, Esophageal Cancer
Adding ramucirumab to FOLFOX did not delay progression in patients with untreated advanced gastric or esophageal adenocarcinoma, according to trial results presented at the 2014 ASCO Annual Meeting.
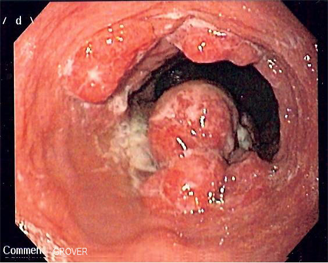
Endoscopic image of an esophageal adenocarcinoma seen at the gastroesophageal junction; source: Montek, Wikimedia Commons
CHICAGO-Adding ramucirumab to FOLFOX did not delay progression in patients with untreated advanced gastric or esophageal adenocarcinoma, according to the results of a phase II trial presented Monday at the 2014 American Society of Clinical Oncology (ASCO) Annual Meeting.
However, the anti-VEGFR2 monoclonal antibody was found to improve disease control rate, and to provide a longer progression-free survival in a subgroup of patients with gastric or gastroesophageal junction adenocarcinoma.
The results of the study (abstract 4004) were presented by Harry H. Yoon, MD, of the Mayo Clinic, Rochester, Minn.
“Adenocarcinoma of the esophagus and the gastroesophageal junction has increased dramatically in the last 30 years in the United States,” Yoon said during his presentation. “Whereas, incidence of subcardial gastric cancers has generally decreased. Still, the prognosis in all three tumor locations is poor.”
This study was designed to explore the use of ramucirumab, an anti-VEGFR2 monoclonal antibody in the first-line treatment of patients with untreated metastatic or locally advanced gastric, esophageal, or gastroesophageal junction adenocarcinoma. The trial included 168 patients from 47 US sites who were randomly assigned to 8 mg/kg ramucirumab plus mFOLFOX or placebo plus mFOLFOX. The protocol allowed discontinuation of one or more agents while continuing others. The primary endpoint was progression-free survival. Almost half of the patients on each arm had esophageal cancer.
Analysis of the intent-to-treat population showed that patients assigned to ramucirumab/FOLFOX had a median progression-free survival of 6.44 months compared with 6.74 months for patients assigned to the placebo arm (HR = 0.98). Similarly, no significant difference on overall survival was found between the two treatment arms (HR = 1.08).
However, disease control rate was higher in the ramucirumab arm compared with the placebo arm (85% vs 67%; P = .008). Sixty-nine percent of patients in the placebo arm and 43% of patients assigned ramucirumab discontinued treatment.
“In light of the high rates of treatment discontinuation in the ramucirumab arm, we took a close look at adverse events,” Yoon said.
The adverse event with the highest frequency in the ramucirumab arm was thrombocytopenia (56%); 39% of patients in the placebo arm had thrombocytopenia. Other adverse events with high rates in the ramucirumab arm were decreased appetite (42%), dehydration (28%), and hypokalemia (20%).
Overall though, Yoon said that there were no new ramucirumab-related safety signals identified in this trial.
The researchers conducted an exploratory analysis of progression-free survival at therapy discontinuation for non-progressive disease by tumor location and found no statistically significant difference in progression-free survival was identified for patients with esophageal adenocarcinoma; however, patients with gastric or gastroesophageal junction cancer assigned to ramucirumab had a median progression-free survival of 9.3 months compared with 7.6 months for patients assigned placebo (P = .036)