Guidelines, Education Permit Safe Outpatient Use of RIT Radioimmunotherapy
WASHINGTON-In 1997, the Nuclear Regulatory Commission issued new guidelines for radiation therapy that, for the first time, permitted outpatient use of radioactive iodine therapy in selected patients (ie, highly compliant patients discharged to low-occupancy settings). Previously, this therapy had required inpatient treatment and 3 days of isolation.
WASHINGTONIn 1997, the Nuclear Regulatory Commission issued new guidelines for radiation therapy that, for the first time, permitted outpatient use of radioactive iodine therapy in selected patients (ie, highly compliant patients discharged to low-occupancy settings). Previously, this therapy had required inpatient treatment and 3 days of isolation.
High Level of Staff Education
Outpatient care involving radioimmunotherapy (RIT) is "more convenient" and "less expensive," but requires a high level of staff education to be done safely, said Carolyn Hendrix, RN, OCN, manager of the Cancer Outpatient Treatment Clinic of the Hoag Cancer Center, Hoag Hospital, Newport Beach, California.
At a poster session of the 27th Annual Congress of the Oncology Nursing Society (abstract 71), she described a model developed at Hoag for treating non-Hodgkin’s lymphoma patients with the investigational RIT iodine-131 tositumomab (Bexxar). The successful use of the treatment program, she said, demonstrates the feasibility of the outpatient approach.
‘Distance, Time, and Shielding’
"Distance, time, and shielding" are the keys to safe RIT treatment, Ms. Hendrix said. Nurses must be trained to work efficiently so that contact with patients getting radioactive antibodies is minimized. The treatment must take place away from highly traveled areas of the hospital (in a lead-shielded isolation room), and all staff involved with these patients must wear badges to monitor radiation.
Patients and staff must be educated about the dangers of radiation and the steps that can lessen them, Ms. Hendrix said.
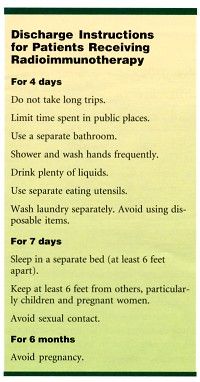
On discharge, she said, patients must receive explicit and detailed instructions on the restrictions that must be observed after radioimmunotherapy (see Table). These instructions include sleeping in a separate bed, staying 6 feet or more away from children and pregnant women, avoiding long trips, limiting time in public places, and generally assuring that other people do not come into direct contact with either patients or their bodily fluids.