High Tumor Volume Confers CAR T-Cell Therapy Toxicity Risk in LBCL
Data support incorporating volumetric PET biomarkers into toxicity risk prediction for patients receiving CAR T-cell therapy for LBCL.
"Clinically, [these findings] present opportunities for early interventions such as bridging therapy, prophylactic steroids, or tocilizumab to reduce risk before the infusion," according to study investigator Burcin Agridag Ucpinar, MD.
High tumor volume was the most consistent biomarker that correlated with CAR T-cell therapy-associated toxicity including cytokine release syndrome (CRS), immune effector cell-associated neurotoxicity syndrome (ICANS), and non-relapse mortality (NRM) in patients with large B-cell lymphoma (LBCL), according to retrospective data presented at the 2025 Society of Nuclear Medicine & Molecular Imaging Annual Meeting.
Across a total population of 367 patients, the median overall survival (OS) was 48 months (95% CI, 31-not evaluable). Additionally, the OS rate was 72% (95% CI, 67%-77%) at 12 months, 59% (95% CI, 54%-65%) at 24 months, and 53% (95% CI, 47%-60%) at 36 months. Data showed a median progression-free survival (PFS) of 12 months (95% CI, 8.8-18), with a 12-month PFS rate of 50% (95% CI, 45%-56%), a 24-month rate of 41% (95% CI, 36%-47%), and a 36-month rate of 36% (95% CI, 31%-43%).
Statistically significant predictors of grade 3 or higher CRS per univariate analysis included maximum standardized uptake value (SUVmax; OR, 1.61; 95% CI, 1.12-2.34; P = .011), tumor volume (OR, 1.22; 95% CI, 1.12-1.32; P <.001), total lesion glycolysis (TLG; OR, 1.20; 95% CI, 1.11-1.30; P <.001), and elevated lactate dehydrogenase (LDH) prior to lymphodepletion (OR, 6.58; 95% CI, 2.33-23.5; P <.001). Other predictors of high-grade CRS per multivariate analysis included tumor volume (OR, 1.16; 95% CI, 1.06-1.29; P = .001) and elevated LDH (OR, 3.05; 95% CI, 0.88-12.3; P = .079).
Univariate analysis indicated that SUVmax (OR, 1.33; 95% CI, 1.02-1.72; P = .034), tumor volume (OR, 1.12; 1.04-1.19; P = .002), TLG (OR, 1.11; 95% CI, 1.04-1.19; P = .004), Karnofsky performance status prior to CAR T-cell therapy (OR, 2.52; 95% CI, 1.31-5.27; P = .005), and elevated LDH (OR, 1.99; 95% CI, 1.17-3.41; P = .012) correlated with grade 3 or higher ICANS. Additionally, univariate analysis showed that treatment with tisagenlecleucel (Kymriah) vs axicabtagene ciloleucel (axi-cel; Yescarta; OR, 0.40; 95% CI, 0.18-0.84; P <.001) and lisocabtagene maraleucel (liso-cel; Breyanzi) vs axi-cel (OR, 0.28; 95% CI, 0.13-0.54; P <.001) conferred lower risks of high-grade ICANS. Per multivariate analysis, notable predictors of grade 3 or higher ICANS included tumor volume (OR, 1.09; 95% CI, 1.01-1.17; P = .032), Karnofsky performance status prior to CAR T (OR, 2.21; 95% CI, 1.09-4.78; P = .027), tisagenlecleucel vs axi-cel (OR, 0.28; 95% CI, 0.11-0.64; P <.001), and liso-cel vs axi-cel (OR, 0.21; 95% CI, 0.10-0.44; P <.001).
Predictors of grade 3 or higher immune effector cell-associated hematotoxicity (ICAHT) included tumor volume (OR, 1.08; 95% CI, 1.01-1.15; P = .027), TLG (OR, 1.08; 95% CI, 1.01-1.15; P = .026), Karnofsky performance status of less than 90 prior to CAR T-cell therapy (OR, 1.83; 95% CI, 1.08-3.19; P = .024), elevated LDH (OR, 3.12; 95% CI, 1.95-5.03; P <.001), and a Hematotox score of 2 or higher (OR, 2.03; 95% CI, 1.26-3.31; P = .003) based on univariate analysis. Per multivariate analysis, elevated LDH was a significant predictor of high-grade ICAHT (OR, 2.75; 95% CI, 1.62-4.72; P <.001).
Regarding NRM, significant predictors based on univariate analysis included tumor volume (HR, 1.23; 95% CI, 1.13-1.33; P <.001), TLG (HR, 1.15; 95% CI, 1.07-1.24; P = .003), age at CAR T-cell therapy (HR, 1.04; 95% CI, 1.00-1.08; P = .048), and elevated LDH (HR, 2.87; 95% CI, 1.21-6.82; P = .019). Tumor volume was the only significant predictor of NRM per multivariate analysis (HR, 1.20; 95% CI, 1.10-1.30; P <.001).
“Our study found metabolic tumor volume to be the strongest imaging predictor of CRS, ICANS, and [NRM], surpassing SUVmax and TLG,” lead investigator Burcin Agridag Ucpinar, MD, a radiologist at Memorial Sloan Kettering Cancer Center (MSKCC), stated in the presentation. “Clinically, [these findings] present opportunities for early interventions such as bridging therapy, prophylactic steroids, or tocilizumab [Actemra] to reduce risk before the infusion.”
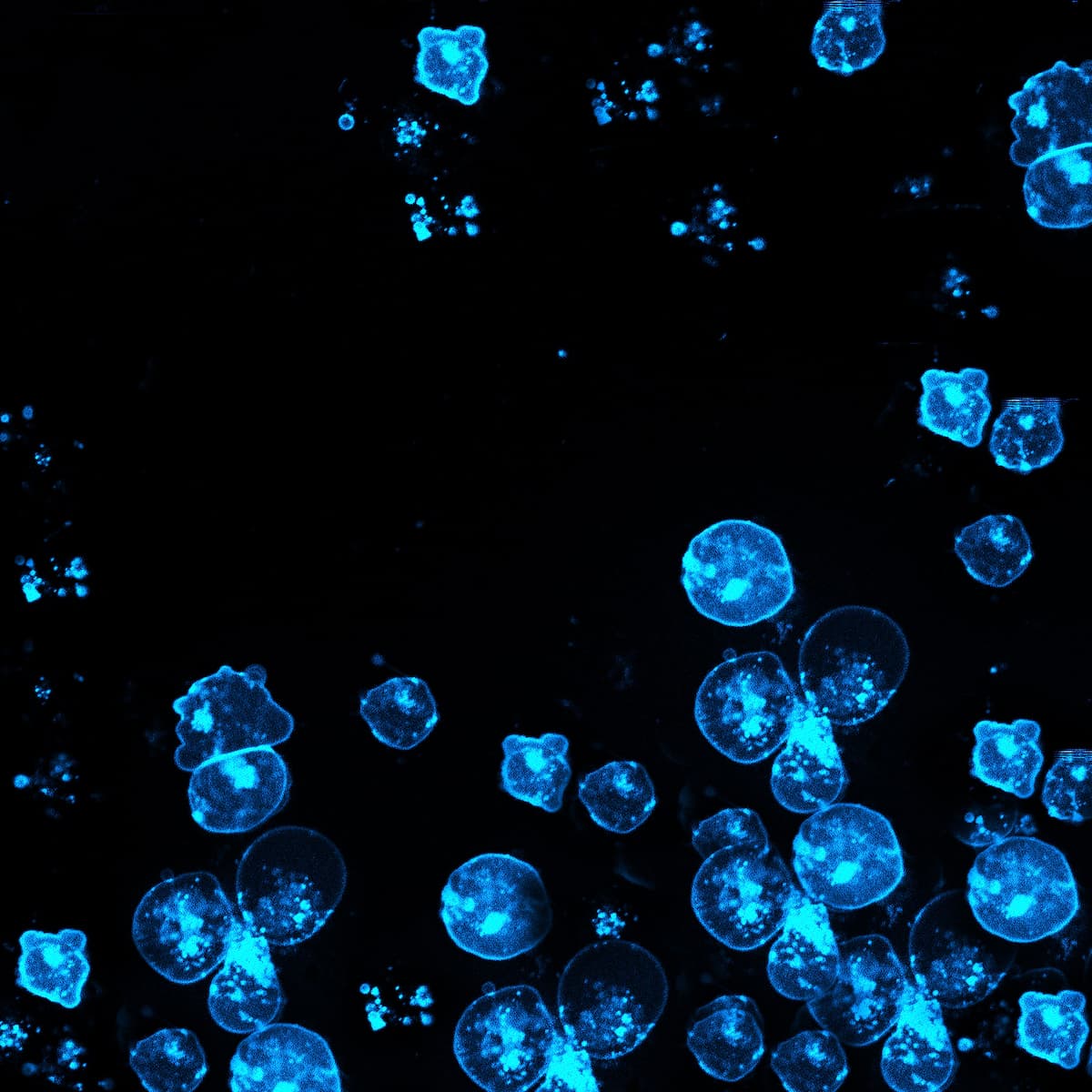
Investigators of this study aimed to evaluate the ability of fludeoxyglucose (FDG) PET/CT to predict toxicity in patients with LBCL who receive CAR T-cell therapy. The analysis included 367 patients with LBCL who received commercial CAR T-cell therapy with pre-infusion body FDG PET/CT imaging at MSKCC from April 2016 to February 2025.
Three radiologists with more than 8 years of experience interpreted pre-treatment FDG PET/CT images, and key tumor burden metrics included tumor volume, SUVmax, and TLG. Investigators evaluated CRS and ICANS based on American Society for Transplantation and Cellular Therapy (ASTCT) criteria and defined early ICAHT as the presence of neutropenia or hematologic suppression. Additionally, the study recorded intensive care unit admission and 30-day mortality, and investigators determined treatment responses per Lugano 2014 criteria.
Use of logistic regression models helped determine associations between radiologic and clinical variables and grade 3 or higher CRS, ICANS, and ICAHT. Multivariate models included covariates such as age, Karnofsky performance status, LDH, CAR T-cell therapy product, non-Hodgkin lymphoma transformation origin, and bridging therapy.
The median patient age was 66 years, and most were male (66%). A majority of the population had diffuse LBCL not otherwise specified (78%), stage III or IV disease (69%), at least 3 prior lines of treatment (74%), and bridging therapy (84%). The most common CAR T-cell therapies included axi-cel (48%), liso-cel (33%), and tisagenlecleucel (19%).
“This is the largest cohort study to date evaluating PET biomarkers for CAR T-cell toxicity in [LBCL]. Volumetric PET parameters, particularly metabolic tumor volume, offer the best predictive value,” Ucpinar concluded. “These insights can help guide individualized strategies such as bridging [therapy] or closer surveillance for high-risk patients.”
Editor’s Note: Ucpinar had no disclosures in her presentation.
Reference
Ucpinar BA, Brown S, Bedmutha A, et al. PET-based biomarkers for toxicity prediction in CAR T-cell therapy for aggressive lymphoma: evidence from a large-scale retrospective analysis. Presented at 2025 SNMMI Annual Meeting; June 21-24, 2025; New Orleans, LA.