Homoharringtonine May be ‘Better Alternative’ to Etoposide In Pediatric AML
Investigators of a prospective study of 1253 patients find that outcomes with the experimental homoharringtonine-based regimen either meet or exceed those with a classic etoposide-based regimen.
"Our results indicate that the HHT-based induction regimen could result in higher CR [rates] and improved survival, which may be a better alternative for the treatment of de novo patients with childhood AML, particularly those with AML1-ETO [positivity]," according to the study authors.
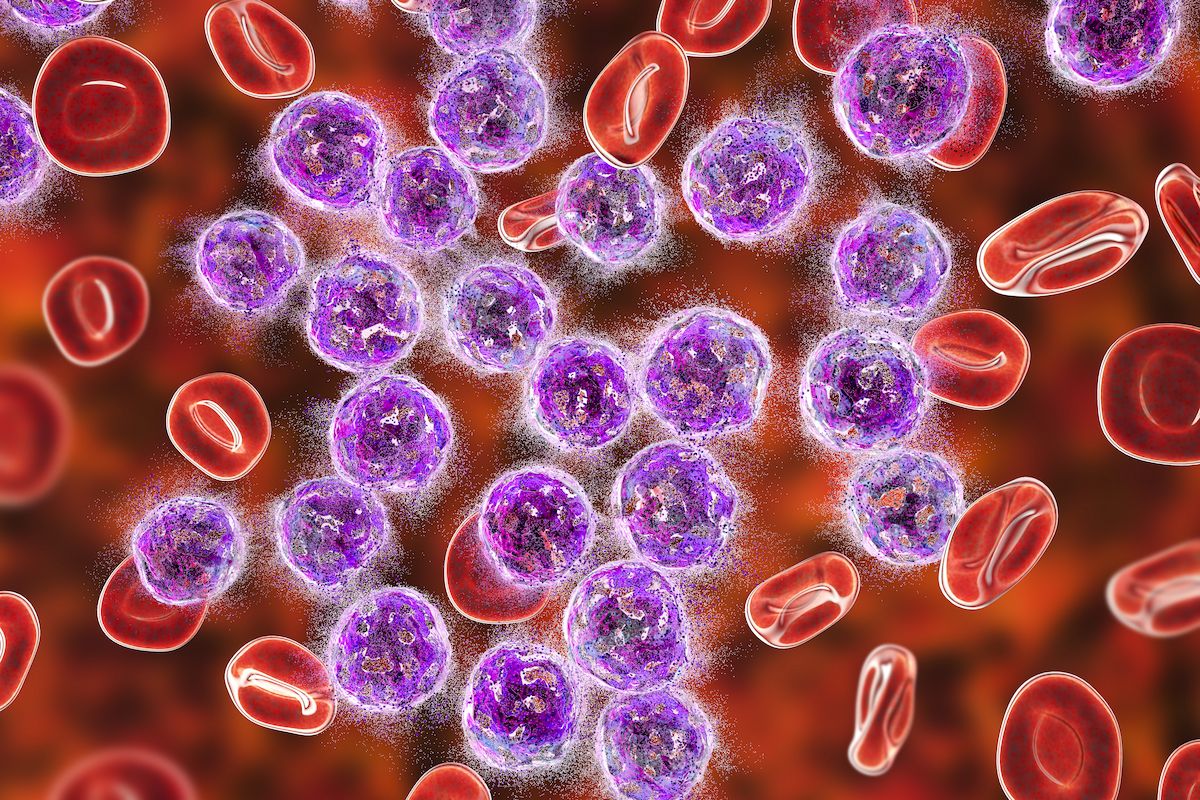
Use of homoharringtonine (HHT) may result in improved responses among patients with pediatric acute myeloid leukemia (AML) compared with etoposide-based induction therapy, according to findings from a study published in the Journal of Clinical Oncology.
The rate of complete remission (CR) was 79.8% (n = 474/594) in the HHT arm vs 73.9% (n = 487/659) in the etoposide arm (risk ratio [RR], 1.08; 95% CI, 1.02-1.15; P = .014). For patients with intermediate-risk disease, the corresponding values were 80.1% vs 72.0%, respectively (RR, 1.11; 95% CI, 1.001-1.24; P = .048). HHT was favored over etoposide after adjusting for age, sex, ethnicity, initial white blood cell count, the presence of transformed AML, the presence of myeloid sarcoma, the presence of testicular involvement fusion genes, and cytogenetic risk (odds ratio [OR], 1.49; 95% CI, 1.126-1.998; P = .006).
The 3-year rate of overall survival (OS) was 69.2% (95% CI, 65.1%-72.9%) in the HHT arm vs 62.8% (95% CI, 58.7%-66.6%) in the etoposide arm (P = .025); the corresponding values for event-free survival (EFS) were 61.1% (95% CI, 56.8%-65.0%) vs 53.4% (95% CI, 49.2%-57.3%), respectively (P = .022). The HR for death after adjusting for patient and disease variables in the HHT and etoposide arms was 0.75 (95% CI, 0.58-0.97; P = .031), and the HR for events was 0.77 (95% CI, 0.60-0.97; P = .028).
Moreover, the rate of EFS at 3 years was 58.9% (95% CI, 52.6%-64.7%) among patients who received HHT and all-trans retinoic acid (ATRA)–based maintenance therapy compared with 54.6% (95% CI, 49.0%-59.9%) among those who received etoposide- and cytarabine-based maintenance (P = .395). The 3-year OS rates were 68.4% (95% CI, 62.2%-73.8%) vs 65.3% (95% CI, 59.8%-70.3%), respectively (P = .489).
EFS rates at 3 years in the per-protocol population of patients who received maintenance therapy were 70.7% (95% CI, 61.1%-78.3%) with HHT and ATRA maintenance, 74.8% (95% CI, 67.0%-81.0%) with HHT and cytarabine maintenance (P = .933), 72.9% (95% CI, 65.1%-79.2%) with etoposide and cytarabine maintenance (P = .789), and 66.2% (95% CI, 56.8%-74.0%) with etoposide and ATRA maintenance (P = .336).
Notably, investigators reported that patients with AML1-ETO positivity who received HHT and ATRA had a 3-year EFS rate of 73.6% compared with 52.8% among those treated with etoposide and cytarabine (P = .013).
“Etoposide is widely used for many hematologic diseases. However, its potential risk of therapy-related secondary cancers has attracted attention, especially for AML with MLL rearrangement,” the investigators wrote. “Our results indicate that the HHT-based induction regimen could result in higher CR [rates] and improved survival, which may be a better alternative for the treatment of de novo patients with childhood AML, particularly those with AML1-ETO [positivity].”
These data derive from a prospective, open-label clinical trial conducted at 35 centers in China. A total of 1258 pediatric patients were enrolled between August 2015 and October 2019, 1253 of whom were included in the intent-to-treat (ITT) analysis. The median follow-up was 29.4 months (interquartile range [IQR], 8.4-47.4). In the ITT population, 185 patients (14.8%) were lost to follow-up, 70.0% of whom were followed for more than 12 months.
The median patient age was 75.0 months (IQR, 36.0-118.0). Cytogenetic assessment was performed in 98.3% of patients, and investigators found that 59.2% had abnormal karyotypes or fusion genes, and 30.6% had t(8;21)/AML1-ETO–positive disease.
Patients were randomly assigned to either the HHT or etoposide arms. The induction regimens consisted of either a combination of daunorubicin and cytarabine with etoposide at a dose of 100 mg/m2 or HHT at a dose of 3 mg/m2 once daily for days 1 through 5. The regimens also included daunorubicin at a dose of 40 mg/m2 once daily on days 1, 3, and 5, and cytarabine at a dose of 100 mg/m2 once every 12 hours on days 1 through 7. Additionally, idarubicin at 10 mg/m2 once daily on days 1, 3, and 5 could be substituted for the daunorubicin. All patients received 3 courses of consolidation therapy.
Maintenance therapy consisted of either ATRA at a dose of 20 to 30 mg/m2 once daily for the first 2 weeks followed by 6-mercaptopurine at 50 mg/m2 once daily for 10 weeks, or intravenous cytarabine at 40 mg/m2 once daily on days 1 through 4 every 4 weeks and 6-mercaptopurine at 50 mg/m2 once daily for the entire maintenance period.
The primary end points included the composite CR rate among patients who received 2 courses of induction therapy, as well as the 3-year EFS rates in the ITT and per-protocol populations comparing both HHT vs etoposide and the 4 possible complete regimens. Secondary end points included the 3-year OS rates across all arms.
There were 2 major limitations noted by investigators. First, due to a shortage of HHT during the study period, median follow-up was shorter in the HHT arm. Second, some patients assigned to receive ATRA maintenance preferred not to pay for unknown risks and therefore received cytarabine-based maintenance instead.
“Our trial was conducted at 35 centers nationwide with a large sample size, and selection bias was weakened to some extent,” the investigators concluded. “Our results are thus reflective of those that could be obtained from a real-world study.”
Reference
Li J, Gao J, Liu A, et al. Homoharringtonine-based induction regimen improved the remission rate and survival rate in chinese childhood AML: a report from the CCLG-AML 2015 Protocol Study. J Clin Oncol. Published online August 2, 2023. doi:10.1200/JCO.22.02836