Hypertension Drug Improved Survival in Hypertensive Metastatic RCC Patients
The use of angiotensin system inhibitors significantly improved the survival of patients with metastatic RCC who were on the drug for the treatment of hypertension, according to the results of a retrospective study presented at the ASCO GU Symposium.
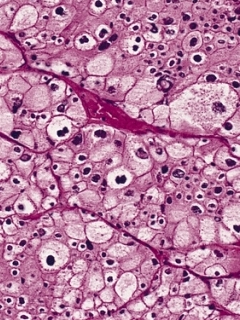
Renal cell carcinoma
The use of angiotensin system inhibitors, or ASIs, significantly improved the survival of patients with metastatic renal cell carcinoma who were on the drug for the treatment of hypertension, according to the results of a retrospective study presented at the 2014 ASCO Genitourinary Cancers Symposium.
“We demonstrated that ASI users had significantly improved survival when compared to ASI non-users, even after adjustment for the development of treatment associated hypertension,” said Rana McKay, MD, a clinical oncology fellow at the Dana-Farber Cancer Institute, during a press conference. “In addition, ASIs appear to have a synergistic activity in patients on VEGF therapy.”
Based on these results, McKay and colleagues said that ASIs should be considered for patients with metastatic renal cell carcinoma who need treatment for hypertension, as long as no treatment contraindications exist.
The prospective study looked at data from 4,736 patients with metastatic renal cell carcinoma taken from a clinical trials database. Patient information was gathered from phase II and phase III trials sponsored by Pfizer.
Patients included any who were taking an ASI at baseline or within 30 days of treatment initiation with a VEGF-targeted agent, such as sunitinib, sorafenib, axitinib, or bevacizumab, an mTOR-targeted agent such as temsirolimus, or interferon.
The majority of patients were aged less than 55 years, were men, and had excellent performance status. Twenty-nine percent of patients had received treatment with an ASI. At baseline, 84% of ASI users had hypertension and 33% of non-users had hypertension.
The researchers found that ASI use was associated with significantly improved progression-free survival (HR = 1.147; 95% CI, 1.044-1.259) and overall survival (HR = 1.213; 95% CI, 1.083-1.360). The median progression-free survival for ASI users was 8.3 months compared with 6.5 months for non-ASI users (P = .0042). Median overall survival was 26.68 months for ASI users compared with 17.05 months for non-ASI users (P = .0009).
McKay and colleagues also analyzed the effect of ASIs by the type of cancer therapy used. Median overall survival for patients taking an ASI plus VEGF-targeted therapy was 31.12 months compared with 21.94 months for non-ASI users on VEGF-targeted therapy, “suggesting a synergistic therapeutic action between VEGF therapies and ASIs,” McKay said. No significant difference between ASI users and non-users was found for patients assigned to mTOR-targeted therapy or interferon therapy.