Increase in Thyroid Cancer Diagnosis
An analysis of thyroid cancer diagnosis and incidence in the United States suggests that there is an epidemic of diagnosis rather than an epidemic of thyroid cancer per se.
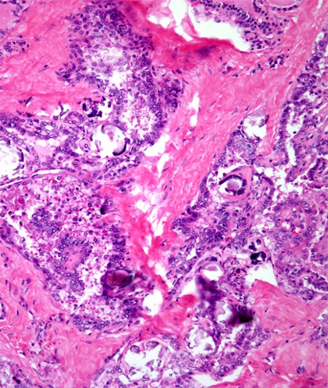
Papillary thyroid carcinoma showing numerous calcifications (psammoma bodies). Source: Cesar A. Moran, MD
An analysis of thyroid cancer diagnosis and incidence in the United States suggests that there is an epidemic of diagnosis rather than an epidemic of thyroid cancer per se. The issue affects more women than men, as the detection rate for women is threefold higher than that for men, even though women have a lower prevalence rate of thyroid cancer by autopsy. The analysis was published in JAMA Otolaryngology-Head & Neck Surgery.
Analyzing Surveillance, Epidemiology, and End Results (SEER) program data from 1975 to 2009 in nine US areas, Louise Davies, MD, MS, and H. Gilbert Welch, MD, MPH, of the Dartmouth Institute for Health Policy and Clinical Practice in Hanover, New Hampshire, found that the incidence of thyroid cancer has tripled since 1975 (absolute increase of 9.4 per 100,000 people). The rate of incidence was stable until the 1990s when it began to increase. The absolute increase in incidence among women was four times higher as compared with men during the same time period.
The mortality rate from thyroid cancer (about 0.5 deaths per 100,000) remained the same between 1975 and 2009, according to mortality statistics from the National Vital Statistics System.
Thyroid cancer has been shown to be a relatively common autopsy finding, even when the patient diagnosed had no documented symptoms throughout their lifetime, found at the time of death due to other causes. Thyroid nodules are also frequently identified by physical examination and imaging.
In 2006, the authors reported an uptick in the incidence of thyroid cancer. The epidemiological data showed that while the rate of thyroid detection increased twofold, mortality as a result of thyroid cancer had not changed-that “virtually all of the increase” was from papillary thyroid cancer diagnosis, the least aggressive form of the disease-and that 87% of the tumors diagnosed were 2 cm or smaller in size. These results had led the authors to conclude that this increased incidence was a result of overdiagnosis.
In 2009, of the approximately 56,000 people in the United States diagnosed with thyroid cancer, the median age at diagnosis was 49 for women and 53 for men. More than 90% of patients had surgery, and approximately 50% also received radiation therapy. Some underwent a lymph node dissection, which is more common in those who received radiation therapy. A total thyroidectomy was performed in about 85% of patients. This suggests that most patients are treated for their thyroid cancer even though this disease will not always harm them during their lifetime.
“These aggressive therapies persist despite guidelines suggesting that partial thyroidectomy is a reasonable approach for lower-risk cancers and data indicating that few patients with papillary thyroid cancer derive survival benefit from radioactive iodine,” stated the authors in their discussion, citing several literature sources.
In their discussion, the authors reasoned that the increased incidence (but stable mortality) is not due to a drastic improvement in treatment of thyroid cancer.
The authors propose several initiatives to cut down on overdiagnosis, including clinical trials to test active surveillance. Memorial Sloan-Kettering Cancer Center in New York City is currently recruiting patients to such an observational study. Another approach, said the authors, is to change the way we think about the word cancer. Both patients and clinicians need to take a more active role in the overtreatment of thyroid cancer, concluded the authors.