Inflammation in Prostate Biopsy May Predict Lower Cancer Risk
Markers of inflammation should be analyzed and reported in prostate biopsies, according to the results of a new study. Researchers found that negative prostate biopsies that had markers of inflammation were less likely to be diagnosed with prostate cancer in a subsequent prostate biopsy.
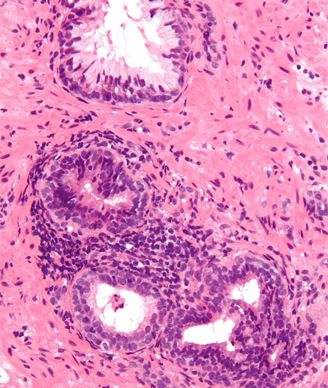
Micrograph of prostate gland with a chronic inflammatory infiltrate. Copyright © 2010 Nephron
Markers of inflammation should be analyzed and reported in prostate biopsies, according to the results of a new study. Researchers found that negative prostate biopsies that had markers of inflammation were less likely to be diagnosed with prostate cancer in a subsequent prostate biopsy. Inflammation is currently not routinely assessed by pathologists analyzing prostate biopsies.
Both acute and chronic inflammation were independently associated with a lower risk of prostate cancer and independent of prostate-specific antigen (PSA) levels.
The results, from the REDUCE (Reduction by Dutasteride of Prostate Cancer Events) trial, are published in the journal Cancer.
Inflammation has been known to play a role in tumorigenesis. Chronic inflammation in the gut has been linked to colorectal cancer, and inflammation associated with viral infections has been found to be associated with liver and bladder cancers. But for prostate cancer, the connection is less clear: some studies have linked inflammation with an increased risk of cancer and anti-inflammatory agents with a reduced incidence of prostate cancer, while others have not shown this association.
While tissue inflammation is often present in benign prostatic hyperplasia and prostate biopsies, whether inflammation in negative biopsies has clinical significance is not clear.
Daniel Moreira, MD, of the North Shore–Long Island Jewish Health System in New Hyde Park, New York, and colleagues analyzed retrospective prostate biopsy data from 6,238 men from the REDUCE study. All study participants were between 50 and 75 years old and had PSA levels between 2.5 and 10 mg/mL. All men had a negative biopsy and had subsequent biopsies 2 and 4 years later.
The 4-year study assessed the role of daily dutasteride in reducing the risk of biopsy-detectable prostate cancer in men who had a negative initial biopsy.
Acute inflammation was detected in 1% (46) of baseline biopsies while chronic inflammation was detected in 63% (3931) of the participants. Fourteen percent (892) of the patients had both chronic and acute inflammation at baseline.
Prostate cancer was detected in 14% (900 patients) at the 2-year time point. Both acute and chronic inflammation was associated with a lower prostate cancer risk by multivariable analysis (odds ratio [OR], 0.75; P = .012; OR, 0.65; P < .001; respectively).
Those with acute inflammation at the 2-year mark had a 25% reduced risk of prostate cancer and those with chronic inflammation had a 35% reduced risk of prostate cancer.
Baseline acute prostate inflammation was associated with an absolute decrease in the risk of prostate cancer detection at the 2-year mark of almost 5%, from 15.3% for those without acute inflammation to 10.4% for those with acute inflammation.
Baseline chronic inflammation was associated with an absolute decrease in the risk of prostate cancer detection at the 2-year mark of 6.7%, from 19.7% for those without chronic inflammation to 13% for those with acute inflammation.
Acute inflammation was most common among younger men who had lower PSA levels and smaller prostates. Chronic inflammation was linked to older men and larger prostate glands.
At the 4-year time point, acute inflammation (but not chronic inflammation) was associated with a reduced risk of prostate cancer (OR, 0.71; P = .031).
The researchers analyzed the pathology of biopsy samples by severity of inflammation. Chronic inflammation was characterized by lymphocytes as well as plasma cells and macrophages. Acute inflammation was characterized by neutrophils within the tissue.
“It is possible that patients with inflammation at baseline biopsy may be followed differently compared with patients without inflammation at baseline biopsy given their risk of subsequent cancer detection is lower,” said Moreira in a released statement.
The study authors propose that inflammation in prostate tissue could reflect immunosurveillance and recognition, by the immune system, of early cancer cells as foreign, leading to “favorable immunomodulation that could potentially explain why inflammation was associated with a lower risk of [prostate cancer] in repeat prostate biopsies in the current study.” Further studies are needed to understand the biological association between inflammation and a potential reduction in prostate cancer risk, which was not addressed by this study.